Diabetes Mellitus:- Part 2 – Diabetes Mellitus, Diagnosis and Management
Diabetes Mellitus
What Sample for Glucose Estimation is needed?
- This test can be done on Serum. The Serum should be separated within 30 minutes of collection.
- The Serum can be stored at 25 °C for 8 hours and at 4 °C for 72 hours.
- Oxalated blood can also be used. Preservative sodium fluoride may be added.
- The plasma can be stored at 25 °C for 24 hours (with preservative sodium fluoride).
How much is the Stability of the sample for glucose?
- One milliliter of blood in an anticoagulant containing fluoride will remain stable for 3 hours.
- Oxalate plasma is stable at 2 to 8 °C for 48 hours.
- Mostly Serum is used, stable for 8 hours at 25 °C and 72 hours at 4 °C.
- A 6 to 8-hour fast is required for a fasting sample.
What are the indications for Diabetes Mellitus Patients?
- This test is done to diagnose diabetes mellitus.
- This test is also done to evaluate and monitor the patient with Diabetes mellitus.
What Screening indications for Diabetes are advised in individuals?
- People aged 45 or older are assessed at 3-year intervals.
- Younger individuals should be screened if they are obese (>120% of the desired weight) or have a body mass index ≥ 27.
- Individuals with H/O first-degree relatives with Diabetes.
- In the case of high-risk ethnic groups, African Americans, Hispanic Americans, Native Americans, and Asian Americans.
- Babies delivered weighing>9 lbs, and there is a previous H/O GDM (gestational diabetes mellitus).
- Individuals with hypertension ≥140/90 mm Hg and H/O atherogenic dyslipidemia.
- HDH-Cholesterol = ≤35 mg/dL.
- Triglycerides = ≥250 mg/dL.
How will you Define Diabetes mellitus?
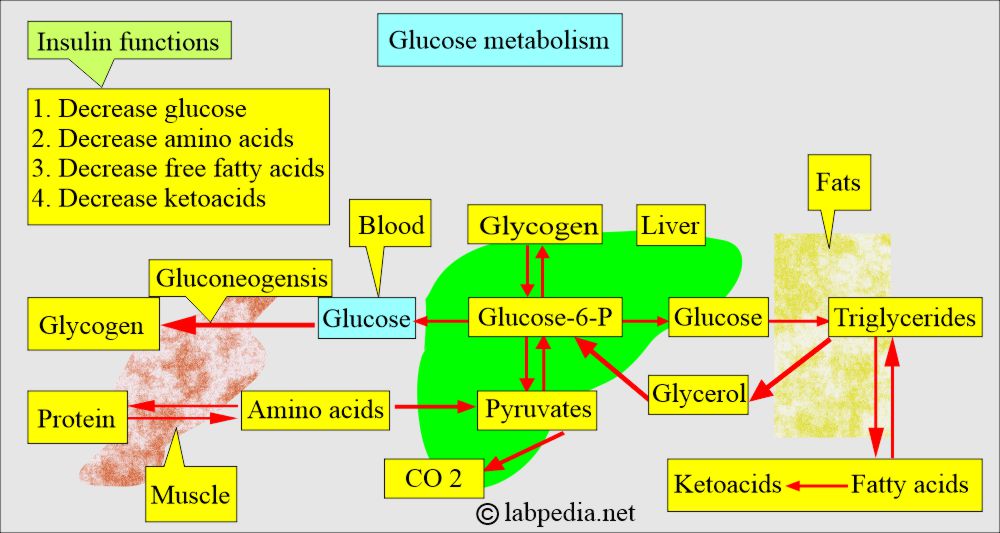
- Diabetes mellitus is a group of metabolic disorders characterized by impaired carbohydrate metabolism, leading to hyperglycemia.
- This is not a single disease but a group of disorders, and glucose intolerance is common among them.
- Diabetes mellitus describes a syndrome characterized by chronic hyperglycemia and disturbances of carbohydrate, protein, and fat metabolism.
- Diabetes Mellitus is a metabolic disorder characterized by hyperglycemia that results from defects in insulin secretion, insulin action, or both.
- This condition is also associated with abnormalities in protein and fat metabolism.
- Diagnosis is dependent upon hyperglycemia and glucosuria.
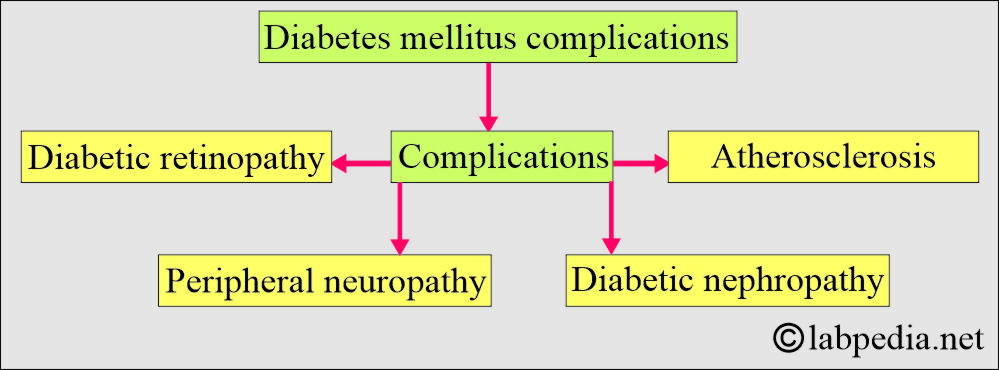
What are the Complications of diabetes mellitus?
- Chronic hyperglycemia leads to:
- Changes in the retina and lens of the eye (retinopathy)
- Damage to the kidneys.
- Microalbuminuria.
- Nephropathy
- The heart, arterial system, and microcirculation are adversely affected.
- Increased risk of heart disease problems.
- These patients may develop neuropathy.
- The foot needs care and may develop gangrene.
- These patients may develop hearing problems.
- There is a chance of Alzheimer’s disease.
Diabetes Mellitus
What are the Criteria for the Diagnosis of Diabetes Mellitus?
- Polyuria, polydipsia, and rapid weight loss.
- Fasting glucose level is high.
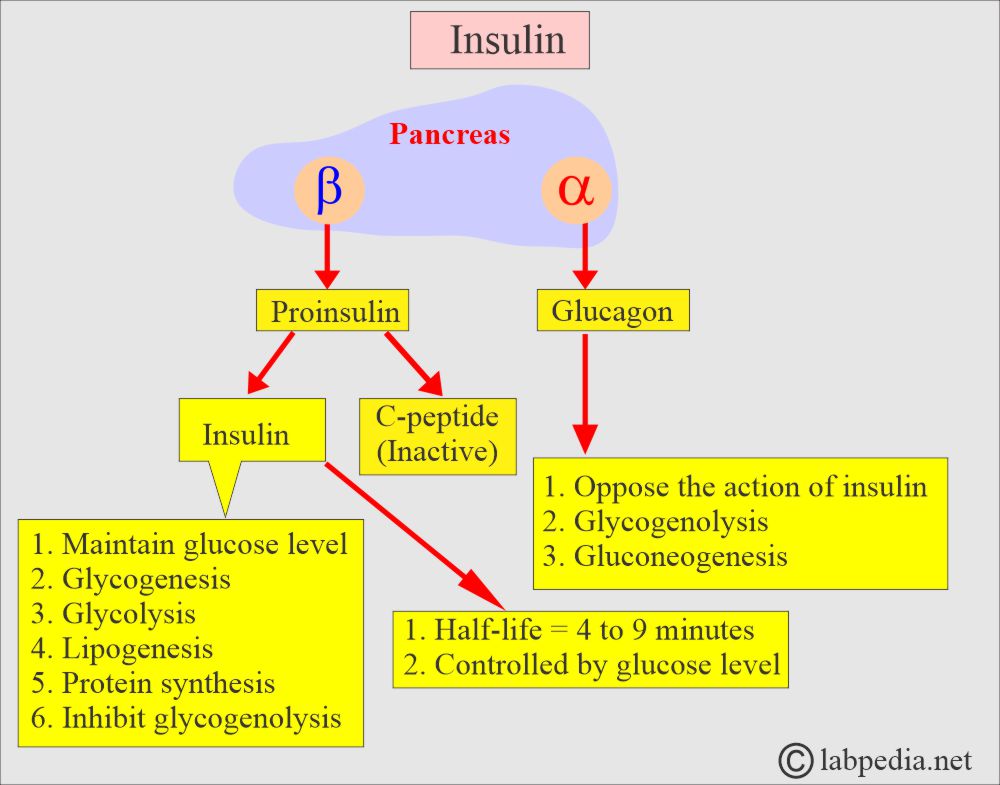
- Insulinopenia occurs when insulin secretion is reduced due to β-cell loss in the pancreas.
- Most patients have an autoantibody, which is an autoimmune process.
- When no cause is known, it is called idiopathic Type.
- Abnormal Glucose tolerance test.
What are the types of Diabetes Mellitus (classification of diabetes mellitus)?
- Type 1 diabetes mellitus (Insulin-dependent, IDDM).
- There is β-cell destruction, usually leading to absolute insulin deficiency.
- This may be immune-mediated.
- It may be Idiopathic.
- Type 2 diabetes mellitus (Noninsulin-dependent, NIDDM).
- There is predominantly insulin resistance with relative insulin deficiency. OR
- There may be predominantly an insulin secretion deficiency with insulin resistance.
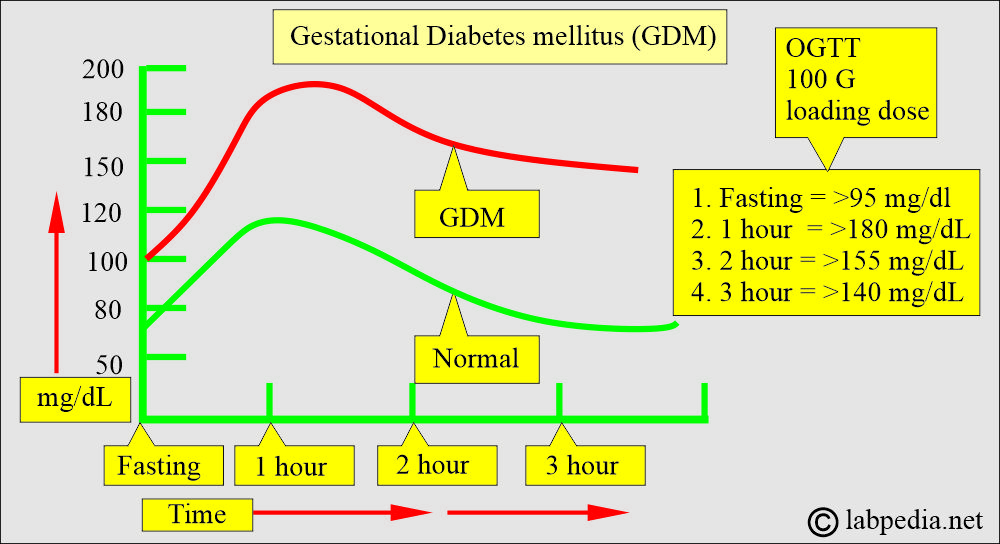
- Gestational Diabetes Mellitus (Gestational diabetes mellitus, GDM).
- It is detected early in pregnancy. This may be type 1 or type 2.
- This is detected in the 2nd or 3rd trimester in 4% of pregnant women.
- Other specific types are:
- The genetic defects of β-cell dysfunction.
- The genetic defect in insulin action (Type A insulin resistance).
What are the causes of diabetes mellitus?
- Diseases of the pancreas (exocrine glands).
- Pancreatitis.
- Trauma or pancreatectomy.
- Tumor of the pancreas.
- Drugs or chemicals induced.
- Thiazide.
- Glucocorticoids.
- Nicotinic acid.
- Infections.
- Cytomegalovirus (CMV).
- Congenital rubella.
- Endocrinopathies.
- Glucagonoma.
- Cushing’s syndrome.
- Acromegaly.
- Immune-mediated diabetes.
- Genetic syndromes associated with diabetes mellitus are:
- Turner syndrome.
- Down’s syndrome.
- Myotonic dystrophy.
- Friedreichs Ataxie.
Diabetes Mellitus Type 1 (Insulin-dependent diabetes mellitus, IDDM)
How will you define Type 1 Diabetes Mellitus?
- This is also called:
- Juvenile-onset Diabetes.
- Juvenile Diabetes.
- Ketosis-prone diabetes.
- Brittle Diabetes.
- Autoimmune Diabetes.
- Idiopathic Diabetes.
- There is a long preclinical period, followed by an abrupt onset of clinical manifestations.
- Patients are prone to developing ketoacidosis.
- There is a dependency on insulin.
- This often affects young people around puberty.
- The peak age of onset is 11 to 13 years.
- The risk for the sibling is 5% to 10%, while the risk for the offspring is 2% to 5%.
- There are several syndromes of autoimmune and genetic origin.
What is the pathogenesis of type 1 diabetes mellitus?
- The autoimmune phenomenon may be the cause of type 1 diabetes mellitus:
- Type 1 diabetes mellitus is due to cell-mediated autoimmunity that leads to the destruction of pancreatic β-cells.
- The islet cells are infiltrated by mononuclear cells, a condition called insulitis.
- The autoimmune process for type 1 diabetes begins years before the clinical presentation.
- An 80% to 90% reduction in the volume of β-cells is needed before clinical Diabetes appears.
- Destruction of the β-cells is more rapid in children than in adults.
- While other α, δ, and other islet cells are preserved.
- Antibodies that may play a role in type 1 diabetes are:
- There is a marker of β-cell autoimmunity in which antibodies in the serum are detected before Diabetes appears.
- Islet cell cytoplasmic antibodies.
- Insulin auto-antibodies.
- Glutamic acid decarboxylase antibodies.
- Genetic role:
- Type 1 diabetes is inherited, but the mode of inheritance remains unclear.
- Environmental factors:
- There are various factors reported, and one of those is the virus.
- Viruses such as mumps, Bella, and coxsackievirus B are blamed.
- Other factors like cow’s milk and chemicals.
- This is because of the severe or complete absence of insulin due to the loss of beta cells in the pancreas.
- Destruction of the islet cells may be due to the following:
- Genetics.
- Autoimmunity.
- Environmental factors.
- In 80% to 90% of cases, islet cell autoantibodies and antibodies to insulin and glutamic acid decarboxylase cause damage to the islet cells.
- Non-immune type 1 diabetes can occur secondary to other diseases, such as pancreatitis.
- Pathology: Beta-cell abnormalities are present long before the onset of type 1 diabetes mellitus.
- Both beta and alpha cell functions are abnormal, with a lack of insulin and a relative excess of glucagon produced by the alpha cells.
What are the signs and symptoms of diabetes mellitus Type 1?
- Glucose accumulates in the blood (hyperglycemia) and is excreted in the urine.
- Weight loss occurs due to the breakdown of proteins and fats.
- There is polyuria, polyphagia, and polydipsia.
- There is a wide fluctuation in the blood glucose level.
- There may be ketoacidosis because of the breakdown of protein and fat.
- There are increased ketone bodies.
- The pH drops, triggering the buffer system and leading to metabolic acidosis.
-
- There is a fruity odor in the breath due to the volatile ketone body acetone.
-
- The patient may go into a coma.
What are the clinical manifestation and their explanation?
| Clinical manifestation | Explanation |
|
There is fluid loss due to osmotic diuresis and to the breakdown of body tissue, as fat and protein are used for energy. |
|
Metabolic changes that impair nutrient utilization can contribute to lethargy and fatigue. |
|
This is due to the depletion of the body’s fat, protein, and carbohydrate stores, leading to cellular starvation and increased hunger. |
|
This is due to a raised blood sugar level, which osmotically attracts the water from the cells, leading to intracellular dehydration and ultimately stimulating the hypothalamus and thirst. |
|
Hyperglycemia acts as an osmotic diuretic, leading to glycosuria and water loss in the urine. |
What is the Treatment of Diabetes Mellitus Type 1?
- This will need a combination of the following:
- Insulin.
- Food planning.
- Exercise.
- More details are discussed at the end of this discussion.
Diabetes Mellitus Type 2 (NON-Insulin dependent NIDDM)
How will you define Diabetes mellitus type 2?
- This is also called:
- Adult-onset type diabetes.
- Maturity-onset Diabetes.
- Ketosis-resistant diabetes.
- Patients have minimal symptoms.
- This is not dependent on insulin to prevent ketonuria.
- The insulin level may be normal, decreased, or increased.
- Most patients have impaired insulin action.
- There is the interaction of metabolic, genetic, and environmental factors.
- It affects people after the age of 40 years, and mostly these people are obese.
How will you discuss the pathophysiology of diabetes mellitus type 2?
- The cause is unknown.
- Genetics may play some role, but it is not clearly defined.
- There is no evidence of the autoimmune mechanism.
- Cellular resistance is a factor in 60% to 80% of people with type 11 diabetes mellitus.
- Insulin resistance increases with obesity.
- There is a decreased response of the β-cell to blood glucose levels and abnormal glucagon secretion.
- There may be alterations in the insulin-receptor or post-receptor events.
- There may be an increase in insulin levels to compensate for insulin resistance in peripheral tissues, but there is still relative insulin deficiency.
- The changes in the pancreas are nonspecific:
- 10% to 40% of the cases show amyloidosis of the pancreas in type 2 diabetes mellitus.
- Pancreatic fibrosis occurs in 33% to 66% of cases with type 2 diabetes, leading to a decreased number of β-cells.
- Generally, there is a decrease in the weight and number of β-cells, and the cause is unclear.
- The most common factor is obesity. It increases 10 times in obese people.
- Also, excessive intake of calories predisposes to type 2 diabetes.
- Insulin can not facilitate the entry of glucose into the muscle cells, hepatocytes, and fat cells.
- One factor is decreased insulin action on peripheral tissues (insulin resistance).
What are the signs and symptoms of diabetes mellitus type 2?
- These are nonspecific.
- Most patients are obese and overweight.
- There is hyperlipidemia.
- Onset is slow and mostly not noted, which leads to late diagnosis.
- Classic symptoms like polydipsia, polyphagia, and polyuria are present.
- There may be nonspecific symptoms like pruritus, recurrent infections, paresthesia, and visual changes.
What is the Treatment of Diabetes Mellitus Type 2?
- This is just like type 1 diabetes. The aim is to keep blood sugar in the normal range.
- There is a need to decrease the calorie intake in an overweight person.
- Saturated fats and cholesterol are restricted.
- Some people recommend a high-fiber diet.
- Oral hypoglycemic drugs may be needed.
- Exercise also helps.
- Insulin may also be given.
What factors will affect glucose level?
- Stress, such as trauma, general anesthesia, infection, burns, and Myocardial infarction, can increase the glucose level.
- Caffeine may increase the level.
- Some pregnant women may experience glucose intolerance. A significantly elevated glucose level is called Gestational Diabetes.
- Drugs may increase the glucose level, such as an antidepressant (tricyclic), Beta-blockers, corticosteroids, I/V glucose, dextrothyroxine, diazoxide, diuretics, estrogen, glucagon, isoniazid, lithium, phenothiazine, phenytoin, and salicylates.
- Drugs like acetaminophen, alcohol, anabolic steroids, insulin, tolbutamide, propranolol, and clofibrate may decrease the glucose level.
What are the American diabetes association recommendations?
| Test | Normal | Goal |
|
|
|
|
|
|
|
|
|
What are the Clinical manifestations and their explanation in Diabetes mellitus?
| Clinical manifestation | Explanations |
|
|
|
|
|
|
|
|
|
|
|
|
Gestational diabetes mellitus
How will you define Gestational diabetes mellitus?
- Definition: Hyperglycemia develops for the first time during pregnancy.
- This is also called:
- Asymptomatic Diabetes.
- Chemical Diabetes.
- Borderline Diabetes.
- Latent Diabetes.
- Subclinical Diabetes.
- Gestational diabetes mellitus develops when glucose intolerance develops during pregnancy, so all pregnant women need to be tested.
- After delivery, glucose levels return to normal, remain impaired, or progress to Diabetes.
- This is first diagnosed during pregnancy and usually in the third trimester.
- Already known cases of diabetic women are not included in this group.
- This occurs in 6% to 8% of pregnant women (another source, only 2% of pregnant women may have this Diabetes).
- Out of this group, 60% may develop Diabetes in 15 years of gestation.
- Later on, these ladies are at increased risk of developing diabetes mellitus (6% to 62% of these ladies).
What are the risk factors for gestational diabetes?
- Risk factors in developing Gestational Diabetes are:
- Pregnant ladies with Glycosuria.
- If there is a family history of Diabetes.
- In obese ladies.
- If the ladies develop pregnancy at a late age.
- In multiparity of 5 or more.
- In the case of previous complicated pregnancies.
What are the diagnostic criteria for gestational diabetes mellitus?
- To diagnose gestational diabetes mellitus.
- Two blood samples on oral glucose tolerance tests (with 100 grams of glucose) are as follows:
| Blood sample timings | Blood glucose level |
|
|
|
|
|
|
|
|
What is the Treatment of gestational diabetes mellitus?
- Advise random or fasting blood glucose during pregnancy.
- It should be aggressive to prevent morbidity and fetal mortality.
Impaired glucose tolerance (IGT)
How will you define impaired glucose tolerance?
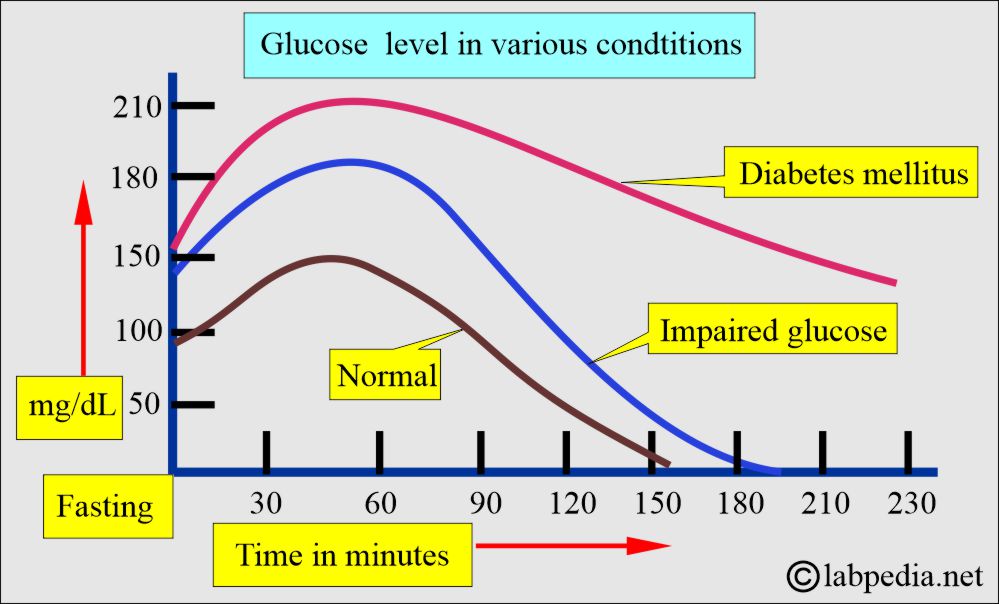
- This group has less fasting glucose than required for diabetes mellitus.
- An oral glucose tolerance test is needed to diagnose this group.
- The overt case develops at a rate of 1% to 5% per year.
- 10% to 20% will convert to type 11 diabetes within 10 years.
- Microvascular diseases are very uncommon in this group.
- Many of them are obese.
What are the Criteria for impaired glucose tolerance?
- With an oral glucose tolerance test:
- 2-hour sample = ≥140 mg/dL.
- Nonpregnant ladies = <200 mg/dL.
Impaired fasting glucose (IFG)
How will you define impaired fasting glucose?
- There is an abnormal response to an oral glucose tolerance test.
What are the Criteria for the diagnosis of Impaired fasting glucose?
- Fasting glucose = ≥110 mg/dL and <126 mg/dL.
- 2 hours of glucose = ≥ 140 mg/dL.
-
-
-
- =<200 mg/dL.
-
-
-
- This is diagnosed by fasting glucose values between normal and diabetic individuals.
- This is a metabolic stage between normal glucose and diabetes mellitus.
- There is an increased risk for the development of Diabetes and cardiovascular disease.
What are the Latest classification criteria for Diabetes mellitus?
- Diabetes mellitus:
- Presence of classic symptoms.
- If the fasting glucose level is 126 mg/dL (>7.0 mmol/L) or higher, it should be labeled as Diabetes Mellitus (when this value is found twice).
- One random glucose level>than 200 mg/dL (11.1 mmol/L) with symptoms of polyuria, polydipsia, and polyphagia is considered diagnostic of Diabetes.
- HbA1c =>6.5 is diagnostic of Diabetes.
- The 2-hour postprandial glucose level was≥200 mg/dl (11.1 mmol/L) during OGTT.
- Impaired fasting glucose = >126 mg/dl. (fasting glucose level 110 to 125 mg/dL (6.1 to 7.0 mmol/L).
- Impaired glucose tolerance when:
- Fasting glucose <126 mg/dl (7 mmol/L).
- OGTT 2-hour sample is 140-199 mg/dL (7.8-11.1 mmol/L).
What are the Criteria for the diagnosis of diabetes mellitus?
- Fasting blood glucose level:
- 126 mg/dL (7.0 mmol/L) or higher is considered diagnostic.
- Random/nonfasting blood glucose level:
- 200 mg/dL (11.1 mmol/L) is diagnostic.
- Oral glucose tolerance test with 75 G of glucose:
- A 2-hour sample of 200 mg/dL (11.1 mmol/L) or higher value is diagnostic.
What are the Values in diabetic patients and normal people?
| Diagnosis | Fasting glucose level | Random glucose level | 2-hour glucose level (in OGTT) | HbA1c |
|
<100 mg/dL (5.6 mmol/L) | <14o mg/dL (7.8 mmol/L) | <5.7% | |
|
100 to 125 mg/dL (5.6 to 6.9 mmol/L) | ≥140 to 199 mg/dL (7.8 to 11.0 mmoml/L) | ≥140 to 199 mg/dL (7.8 to 11.0 mmol/L) | 5.7 to 6.4% |
|
≥ 126 mg/dL (7.0 mmol/L) | 200 mg/dL (11.1 mmom/L) | ≥200 mg/dL (11,1 mmol/L) | ≥6.5% |
What are the Differences between Diabetes Mellitus type 1 and type 2?
| Parameters | Type 1 diabetes mellitus | Type 2 diabetes mellitus |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What is the normal fasting glucose level?
Source 1
| Age | mg/dL |
| Cord blood | 45 to 96 |
| Premature | 20 to 60 |
| Neonates | 30 to 60 |
| Newborn 1 day | 40 to 60 |
| >one day | 50 to 80 |
| Child | 60 to 100 |
| Adult | 74 to 104 |
| 60 to 90 years | 82 to 115 |
| >90 years | 75 to 121 |
- To convert to SI units x 0.0555 = mmol/L
- Values vary from the biochemical method used.
Source 6 for glucose level
| Blood glucose fasting | mg/dL | mmol/L |
| Cord | 45 to 96 | 2.5 to 5.3 |
| Premature infants | 20 to 60 | 1.1 to 3.3 |
| Neonatal | 30 to 60 | 1.7 to 3.3 |
| Infants | 40 to 90 | 2.2 to 5.0 |
| Child <2 years | 60 to 100 | 3.3 to 5.5 |
| Child >2 years to adult | ||
| Fasting | 70 to 100 | <6.1 |
| Elderly | Increase after 50 years |
Source Tietz
Plasma/ serum glucose level
- Adult = 74 to 106 mg/dL (4.5 to 5.9 mmol/L)
- Children = 60 to 100 mg/dL (3.5 to 5.6 mmol/L)
- Premature neonates = 20 to 60 mg/dL (1.1 to 3.3 mmol/L)
- Term neonates = 30 to 60 mg/dL (1.7 to 3.3 mmol/L)
The whole blood glucose level
- 65 to 95 mg/dL (3.5 to 5.3 mmol/L)
CSF glucose level
- 40 to 70 mg/dL (2.2 to 3.9 mmol/L)
- 60% of the plasma
Urine 24-hour glucose level
- 1 to 15 mg/dL (0.1 to 0.8 mmol/L)
The normal value of glucose from another source:
- Usually, glucose between 70 to 110 mg/dl is considered normal.
- Fasting glucose = < 100 mg/dl.
- Cord blood = 45 to 96 mg/dL (2.5 to 5.3 mmol/L)
- premature baby = 20 to 60 mg/dL. (1.1 to 3.3 mmol/L).
- Neonates = 30 to 60 mg/dL (1.7 to 3.3 mmol/L).
- Infants = 40 to 90 mg/dL (2.2 to 5.0 mmol/L).
- Child <2 years = 60 to 100 mg/dL (3.3 to 5.5 mmol/L).
- Child >2 years = like adult level.
- Adult fasting = 70 to 110 mg/dL (<6.1 mmol/L).
- Adult random = <160 mg/dL (11.1 mmol/L).
What are the various types of diabetes mellitus and glucose values?
| Diagnosis | Fasting glucose level | Random/non-fasting glucose level | 2 hours glucose after 75 grams of oral test |
|
>125 mg/dL | >199 mg/dL (classic S/S and glucose ≥200 mg/dL) | >199 mg/dL |
|
>99 mg and <125 mg/dL | – | ≥140 to <200 mg/dL |
|
<126 mg/dL | >139 mg and <200 mg/dL | |
|
>105 mg/dL |
|
Glucose values in whole blood, child/adult:
| Fasting | Child mg/dL | Adult mg/dL |
| Serum or plasma | 60 to 105 | 70 to 100 |
| Whole blood | 50 to 90 | 60 to 100 |
| 2 hours, postprandial | ||
| Serum or plasma | around 150 | around 140 |
| Whole blood | around 120 | around 120 |
Diabetes Mellitus classification based on oral 75 G Glucose overload:
| Patterns of Glucose | Fasting glucose mg/dL | Postprandial glucose mg/dL | 2 hours of glucose mg/dL |
|
|
|
|
|
|
|
|
|
|
|
|
Critical values of Glucose:
| Age | Critical low glucose level mg/dL | Critical high glucose level mg/ dL |
|
|
|
|
|
|
|
|
|
|
|
|
What are the causes of raised glucose levels (Hyperglycemia)?
- Diabetes mellitus, adult, and juvenile.
- Physiological causes.
- Strenuous exercise.
- Strong emotions.
- Shock and burns.
- Infections.
- Endocrine disorders.
- Thyrotoxicosis
- Acromegaly and gigantism.
- Pheochromocytoma.
- Cushing’s syndrome.
- Pancreatic diseases.
- Acute and chronic pancreatitis.
- Pancreatitis due to mumps.
- Cystic fibrosis.
- Hemochromatosis.
- Pancreatic cancers.
- Other causes are:
- Cerebrovascular accident.
- Chronic liver disease.
- Chronic renal disease.
- Acanthosis nigricans.
What are the causes of decreased glucose levels (Hypoglycemia)?
- Pancreatic disorders.
- Islet Cell Tumor.
- Glucagon deficiency.
- Tumors.
- Adrenal gland carcinoma.
- Carcinoma of the stomach.
- Fibrosarcoma.
- Liver diseases.
- In poisoning, e.g., arsenic, chloroform, carbon tetrachloride, phosphorus, salicylates, antihistamines, phenformin, and alcohol.
- Endocrine disorders.
- Hypopituitarism.
- Addison’s disease.
- Hypothyroidism.
- Functional disorders.
- Postgastrectomy.
- Gastroenterostomy.
- Autonomic nervous system disorders.
- Pediatric causes.
- Prematurity.
- Infant diabetic mothers.
- Idiopathic leucine sensitivity.
- Enzyme deficiency.
- Galactosemia.
- Fructose intolerance.
- Von Gierke’s syndrome.
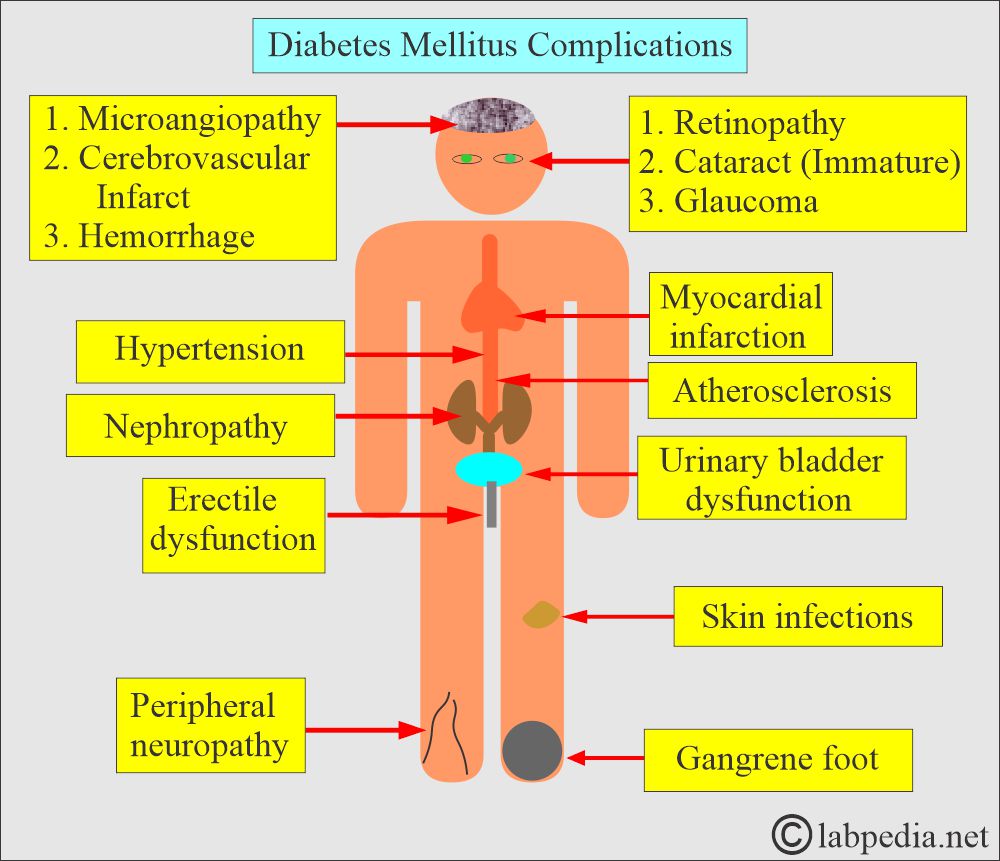
What are the complications of Diabetes Mellitus?
Acute complications are:
- There may be hypoglycemia.
- Patients with uncontrolled hyperglycemia of Type I may develop life-threatening complications like diabetic Ketoacidosis.
- Without treatment, the patient may become acidotic and dehydrated and lose consciousness.
- Type II may develop hyperosmolar coma.
Chronic complications are:
- Peripheral neuropathy.
- Diabetic retinopathy and cataract formation.
- Cardiovascular microangiopathy.
- Coronary atherosclerosis.
- Myocardial infarction is 3 to 5 times more common in diabetic patients.
- AMI is the leading cause of death in diabetes mellitus type 2.
- Peripheral vascular diseases like ischemia of the lower extremities, erectile dysfunction, and intestinal ischemia.
- Gangrene of the foot.
- Diabetic kidney disease (diabetic nephropathy) may lead to end-stage renal disease.
- Chronic pyogenic skin infection.
- Candidal infection of the skin.
- The bones and joints show contracture.
How will you monitor patients with diabetes mellitus?
- In the newly diagnosed patient, check glucose frequently.
- The best times are:
- Before meals.
- At bedtime.
- The goal of therapy is:
- To maintain euglycemia.
- Avoid hypoglycemia.
- Prevent cardiovascular diseases.
- Prevent neurological complications.
How will you treat patients with diabetes mellitus?
- It requires several modalities to treat diabetic patients:
- Diet control:
- This includes dietary fiber.
- Eat low glycemic index foods, which will not raise blood glucose. This glycemic index is 55 or low, including vegetables, fruits, pasta, grainy bread, and legumes.
- High-glycemic-index foods have a glycemic index above 77. This will include potatoes, white bread, and white rice.
- The addition of protein and fats can lower the Glycemic index.
- Artificial sweeteners can be used in cooking and baking.
- Fructose is a natural sweetener and does not increase glucose levels.
- Medications to lower hyperglycemia are:
- The first-generation sulphonylureas are tolbutamide, tolazamide, acetohexamide, and chlorpropamide.
- Second-generation sulphonylureas are glyburide, glipizide, gliclazide, and glimepiride.
- Repaglinide.
- Nateglinide.
- Drugs that lower the glucose level by their action on the liver, muscle, and adipose tissue are:
- Metformin.
- Thiazolidinediones.
- Medications that affect the absorption of glucose are:
- Acarbose.
- Miglitol.
- Incretins are oral insulin stimulators:
- GLP-1 receptor antagonists.
- DPP-4 inhibitors.
- Sodium-glucose co-transporter two inhibitors.
- Insulin has various preparations.
- Transplant of the pancreatic tissue.
What are the hormones produced by the pancreas related to glucose metabolism?
| Chemical substance | Clinical significance |
|
|
|
|
|
|
|
|
Questions and answers:
Question 1: What is the critical value of glucose level in the newborn?
Question 2: What is the fasting glucose level in impaired glucose tolerance?