Culture and Sensitivity, (C and S, C/S), and Antibiotics
Culture and Sensitivity
What samples are needed for Culture and Sensitivity testing?
- Culture can be done on any sample, like:
- Sputum.
- urine,
- pus
- blood
- Cerebrospinal fluid (CSF)
- Feces
- Throat swab for beta-streptococci.
What are the Indications for Culture and Sensitivity?
- For the growth of bacteria or viruses under controlled conditions.
- Culture identifies the organism.
- Culture helps to find a more effective treatment.
What are the precautions for various cultures?
- N. Gonorrhea can be destroyed by the lubricant and disinfectant.
- Menses may change the end result.
- Fecal material may contaminate the anal culture.
- In the case of cervical culture, the patient was advised not to do douching and tub bath.
What are the Drawbacks of culture and sensitivity?
- The major drawback is that it takes one day to grow the organism.
- One day or part of a day is needed to identify the organisms.
- Another day is needed if there is mixed growth to isolate the organism.
- Next, one day is needed for the sensitivity.
- Some organism takes a longer time to grow.
- Still, there are cases where the result is no growth.
- The negative or suppressive effect of the antibiotics therapy, although the patient has the issue.
- There may be a sampling error; the sample is not from the best area of infection.
- The quantity of the sample is not adequate.
- The delay in the transportation of the sample to the lab.
- Flase negative result if the patient is all ready on antibiotics.
- Contamination may give false positive result.
- Some bacteria may have difficulty to grow e.g viruses and M. leprae.
How will you Define culture?
- Culture is the definitive procedure for the detection and identification of the microorganism.
- This is the process of growing microorganisms on a special medium that will support the growth of that given material.
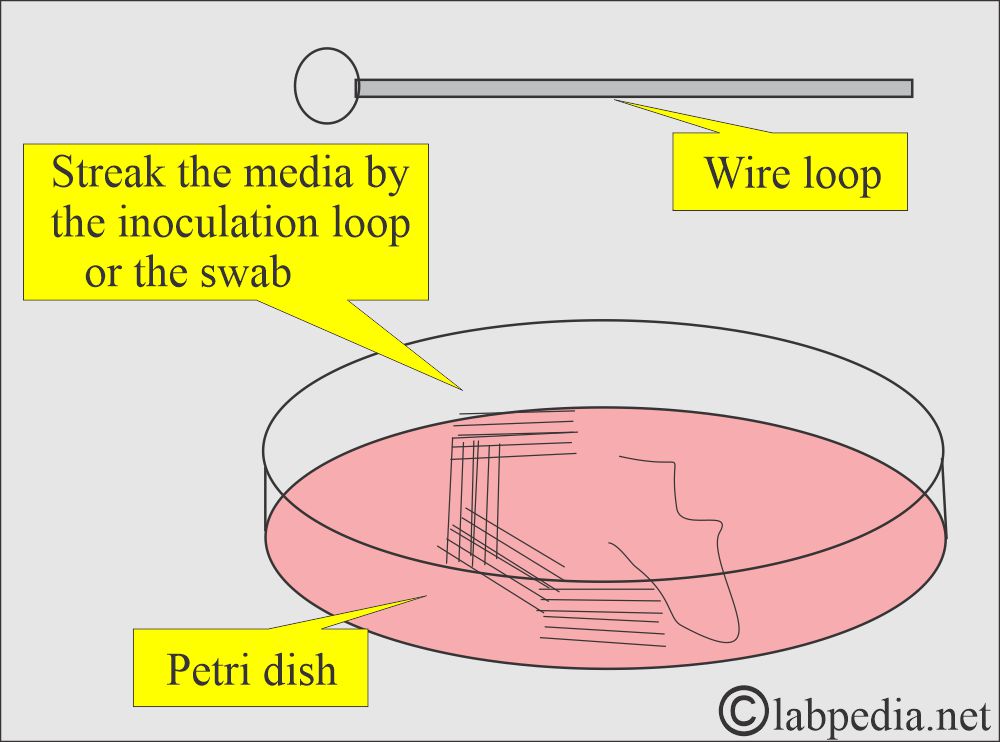
- Culture may be done in the test tube or the Petri dishes.
- Culture media may be liquid, semisolid, or solid.
- The growth of the microorganisms depends upon:
- Proper nutrient ingredients.
- Temperature.
- Presence or absence of oxygen.
- The anaerobic organism is the main flora of the body and is present in the upper respiratory, gastrointestinal, and genitourinary tract.
- So, main purpose of culture and sensitivity:
- Identification of the microorganism, that may be bacteria or fungus.
- What is the sensitivity to the chemical drugs (antibiotics and antifungal drugs).
What is purpose of culture and sensitivity?
- To diagnose the infections.
- To decide proper antibiotics and drugs.
- To find the drug resistence.
What are the sites for Culture?
- The infected wound or ulcer Culture is usually taken from the infected area.
- Material from the wound may show aerobic and anaerobic microorganisms.
- Blood cultures are collected when there is suspicion of bacteremia or septicemia.
- A blood culture may diagnose bacteria, viruses, fungi, or parasites.
- During acute febrile episodes, collect two blood samples and start the antibiotics.
- In the case of PUO (pyrexia for an unknown reason), take two blood samples at an interval of 45 to 60 minutes apart.
- If needed, take two more samples 24 to 48 hours later on.
- In the case of infants and small children, only 1 to 5 mL of the blood may be enough for the culture.
- How to clean the site for blood collection:
- Clean the skin with alcohol and leave it for at least 2 minutes for the alcohol to be effective.
- Or use alcohol followed by iodine or Betadine.
- Leave iodine or Betadine for at least one minute; then, it is removed by alcohol.
- Blood sample:
- Some people believe in one sample from two different sites simultaneously. This will increase the total blood sample.
- In the case of adults, take 10 to 20 mL of the blood directly into the culture tube.
- Mix the blood gently in culture media.
- A quantity <1 mL of blood is insufficient for bacterial culture.
- Results were reported as negative after 5 to 7 days of incubation.
- Eye and ear cultures show S.aureus and H.influenzae predominantly.
- Less common are Bacillus spp. for endophthalmitis, while the swimmer’s ear is usually by P. aeruginosa.
- In children, the most common organisms are S. pneumoniae, H. influenzae, and M.catarrhalis.
- Nasopharynx. The following organism is usually found in a healthy individual:
- C.albicans.
- Diphtheroid bacilli.
- Haemophilus hemolytic.
- Staphylococci, coagulase-negative.
- Streptococci, alpha-hemolytic.
- Lactobacillus.
- Micrococci.
- Nasopharynx culture may show the presence of B. pertussis and C. diphtheriae.
- Sputum culture: This sample should be deep cough material from the bronchi.
- A sputum smear provides a rapid diagnosis of pulmonary tuberculosis.
- Sputum culture usefulness is controversial.
- Upper respiratory bacteria mostly contaminate sputum or bronchoscopic specimens.
- A sputum culture may be done to diagnose the following condition.
- Bacterial pneumonia.
- Bronchiectasis.
- Chronic bronchitis.
- Pulmonary tuberculosis.
- Pulmonary mycotic diseases.
- Mycoplasmal pneumonia.
- Suspected viral pneumonia.
- Throat swab culture: These are important for the diagnosis of:
- A streptococcal sore throat.
- Thrush due to candida infection.
- Diphtheria infection.
- Tonsillar infection.
- Viral infection.
- Gonococcal infection as pharyngitis.
- For Bordetella pertussis.
- To find the beta-streptococcal carrier.
- Carrier of S. aureus.
- Carrier of Corynebacterium diphtheriae.
- Oropharyngeal culture: This culture is taken from male and female patients who are engaged in oral intercourse.
- Wound and abscess will show both aerobic and anaerobic organisms.
- Skin culture: The most common organisms are S. aureus and S.pyogenes.
- The common conditions are:
- Pyoderma as staphylococcal impetigo and Streptococcal impetigo.
- Folliculitis, Furuncle, carbuncle, and Erysipelas.
- Others are Athlete’s foot, ringworm, and Jock itch.
- The common conditions are:
- Stool and anal area culture: Diarrhea may be caused by food poisoning, where the causative agent is a bacterial infection.
- Staphylococcal aureus may generate toxins when it grows in some of the foods.
- Clostridium botulinum produces a neurotoxin that is not correctly canned food.
- This culture is done to rule out the possibility of:
- Salmonella infection.
- Shigella infection.
- A culture of yeast.
- Culture for Shiga toxin-producing E.coli.
- C S F culture: It is very important to find the cause of meningitis because the delay in the diagnosis and the treatment can lead to the patient’s death.
- C S F culture needed to diagnose:
- Bacterial meningitis.
- Viral meningitis.
- TB meningitis.
- C S F culture needed to diagnose:
- Urethral culture: Take the urethral smear before voiding the urine.
- The best time is to collect the morning sample before the micturition.
- Can take a sample by inserting the sterile swab into the anterior urethra.
- Another possibility is taking the sample by prostatic massage.
- Urine culture is used to diagnose bacterial urinary tract infections of the urinary bladder, kidneys, ureter, and urethra.
- The early morning sample is the best because it has a maximum number of bacteria.
- Collect 3 to 5 mL of urine in the sterile container.
- Other methods are catheterization or aspiration of suprapubic or indwelling catheters.
- Urine from the collection urine bag is not a good sample.
- Try to collect the urine sample before starting the antibiotics.
- A bacterial count of >100,000 colonies/mL indicates infection.
- A bacterial count <10,000 colonies /mL indicates contamination and less chance for infection.
- Pyuria is the pus in the urine, and bacteriuria indicates urinary tract infections.
- Cervical culture: Cervical culture is used to diagnose sexually transmitted diseases.
- A cotton swab is inserted into the endocervical canal and moved from side to side to get the culture.
- Put this swab in sterile saline or transport media.
- The specimen should not be refrigerated.
- Synovial fluid: Lie the patient on the back with the joint fully exposed and extended.
- Can give minimum local anesthesia to minimize the pain.
- Sterile the area and insert the needle into the joint space.
- Fluid is obtained for culture and analysis.
| Specimen | Common cause of the infection |
|
|
|
|
|
|
|
|
|
Infection by:
|
|
|
|
|
How will you Classify bacteria?
- Bacteria can be divided based on the following:
- Gram stain:
- Gram-positive.
- Gram-negative.
- Based on morphology:
- Coccus.
- Bacillus.
- Coccobacillus.
- Diplococcus.
- Based on oxygen requirements:
- Aerobic.
- Anaerobic
- Based on the acid-fast stain:
- M. tuberculosis.
- M. bovis.
- M. microti.
- M. leprae.
What are the types of bacteria?
- Streptococci:
- Lancefield group A streptococci.
- Lancefield group B streptococci.
- Lancefield group C, D, F, G streptococci.
- Streptococcus viridans.
- Streptococcus pneumoniae.
- Staphylococcus:
- Staphylococcus aureus.
- Staphylococcus epidermidis.
- Diplococci:
- Meningococci.
- Gonococci.
- Enteric bacilli:
- Salmonella.
- Shigella.
- Enterobacter.
- Klebsiella.
- Escherichia coli.
- Proteus.
- Pseudomonas.
- P. aeruginosa.
- P. putida.
- P. flourescence.
- Brucella:
- B. abortus.
- B. mellitensis.
- B. suis
- Anaerobic bacteria:
- Clostridium tetani.
- Clostridium botulinus.
What are the types of culture media?
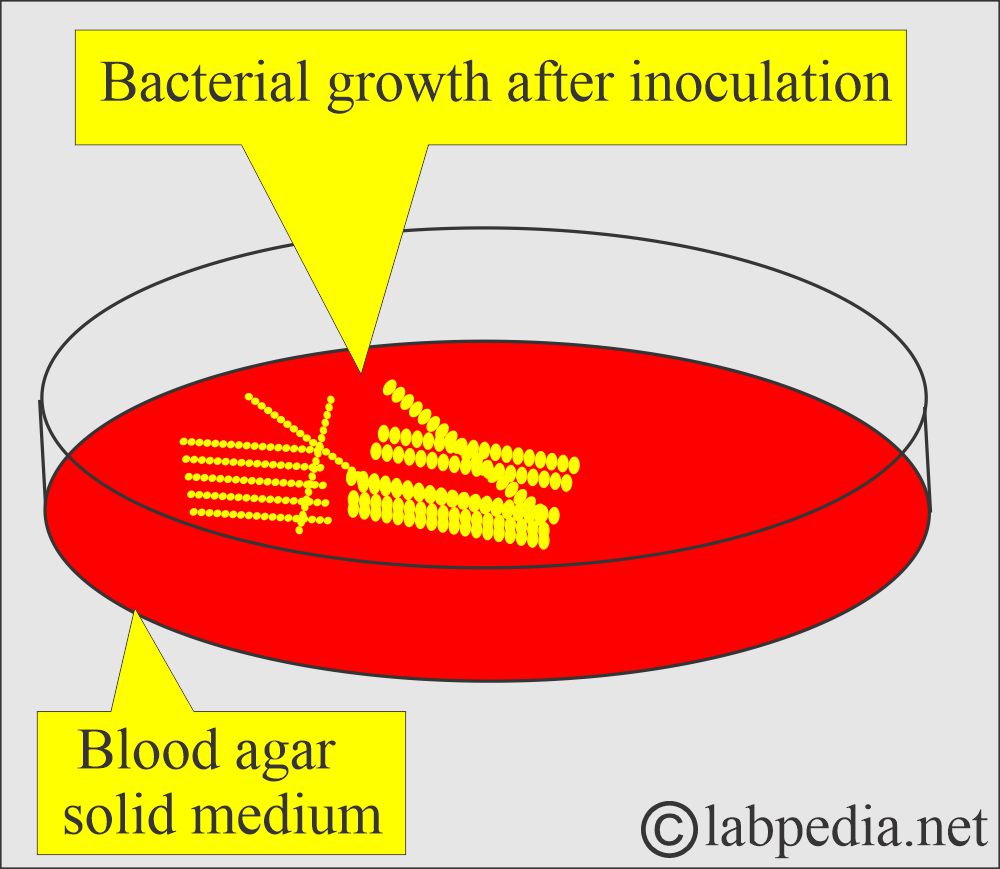
Solid medium:
- Nutrient agar media. This is general culture media.
- Blood agar. It is also general media used in bacteriology.
- Chocolate agar. For isolation of H. influenzae, N. gonorrhoeae.
- McConkey agar. It is used for enterobacteria, where lactose-fermenting colonies are colored pink.
- CLED (cystine-lactose-electrolytes deficient medium), where lactose fermenting colonies are yellow.
- Desoxycholate citrate agar. It is a selective media for salmonellae and shigellae.
- Xylose-lysine deoxycholate agar. It is also a selective medium for salmonellae and shigellae.
- Lowenstein-Jensen media is specific for mycobacterium tuberculosis.
Liquid medium:
- Peptone water is a general culture medium. It is also used for the sugar fermentation test.
- Nutrient broth is also a general culture media.
- Glucose broth is a culture medium for delicate microorganisms.
- Robertson’s meat medium is used for anaerobic and aerobic bacteria.
- Selenite F broth is an enrichment culture medium for salmonellae and shigellae.
- Tetrathionate broth is an enriched medium for salmonellae.
- Transport media is used for the transport of sensitive pathogenic bacteria. This was used for the N. gonorrhea.
Semisolid medium:
- This media contains agar of 0.5 grams as a concentration.
- Semisolid media are used to find the motility of the organism.
- Transport media are mostly semisolid.
- The swab from the suspected area obtains specimens.
What is the Procedure for culture and sensitivity?
- These are sent to a lab in sterile transport media or containers.
- Bacteria need at least 48 hours to get the growth.
- The culture and sensitivity report takes 24 to 48 hours.
- This growth can be subjected to sensitivity to find more specific and effective drugs.
- While the culture of Mycobacterium needs 4 to 6 weeks for growth.
- Viral cultures need at least 2 weeks.
What do you know about the sensitivity test?
- This is the most important part of diagnostic bacteriology, which will help and guide the physician in which antibiotic is important and is effective.
- The sensitivity test can be done in:
- Disc diffusion:
- This method is used widely. The Paper disc is impregnated with an antibiotic solution. This is based on the concentration of the drugs in the blood and the urine. These are placed on the culture plates where the growth is inoculated.
- Tube dilution:
- This is slightly difficult and done in special circumstances like bacterial endocarditis, where the treatment is difficult.
What are the antibiotics effective for bacterial growth?
- Gram-negative bacilli are sensitive to the following:
-
- Cephalosporin
- Cefepime
- Ceftazidime
- Penicillins:
- Piperacillin
- Ticarcillin
- Monobactam:
- Aztreonam
- Quinolones
- Ciprofloxacin
- Levofloxacin
- Gatifloxacin
- Moxifloxacin
- Aminoglycosides:
- Gentamicin
- Tobramycin
- Amikacin
- Carbapenems
- Imipenem
- Meropenem
- Ertapenem
What is the role of Penicillins for bacteria?
- These are bactericidal and inhibit cell wall synthesis.
- The antibacterial spectrum is gram-positive bacteria.
- The antibacterial spectrum is:
- Streptococci, pneumococcal infection, staphylococcal infection, clostridial infection.
- Meningitis.
- Gonorrhea.
- Syphilis.
- Anthrax.
- Actinomycosis.
What is the role of Ampicillin and Amoxycillin?
- The antibacterial spectrum is:
- Urinary and respiratory infections.
- Enteric fever (with a combination of other antibiotics).
What is the role of Cloxacillin and Flucloxacillin?
- The antibacterial spectrum is:
- Staphylococcal infection.
- Similar to penicillins but less active.
What is the role of Cephalosporins?
- These are chemically similar to penicillins.
- These are bactericidal, like penicillins.
- The antibacterial spectrum is:
- Mostly given to hospitalized patients.
- The first-generation cephalosporin is effective against:
- A wide range of gram-positive bacteria and effective against gram-negative bacteria.
- Strep. fecalis.
- H.influenzae.
- Staph. Aureus unless methicillin-resistant.
- A wide range of gram-positive bacteria and effective against gram-negative bacteria.
- The second generation is cefuroxime and cefamandole; cefoxitin is effective against:
- Wide range of both gram-positive and gram-negative bacteria.
- It has replaced first-generation cephalosporins and is effective in severe infections.
- H.influenzae.
- Bacteroides species.
- Wide range of both gram-positive and gram-negative bacteria.
- The third generation is cefotaxime and ceftazidime and is effective against:
- Similar to the second generation.
- Effective in sepsis due to aerobic gram-negative bacilli.
- Cefsulodin is effective for only ps. aeruginosa.
What is the role of Sulphonamides?
- Sulphonamide, in combination with trimethoprim with a ratio of 5:1, is administered orally, intramuscular, and intravenously.
- These are bacteriostatic.
- These are effective against gram-positive and gram-negative bacteria.
- Ps. aeruginosa is resistant to this drug.
- These are used:
- For urinary and respiratory infections.
- For invasive salmonellosis.
- For pneumocystis pneumonia.
What is the role of Aminoglycosides?
- This is a family of antibiotics consisting of:
- Gentamicin.
- Tobramycin.
- Netilmicin.
- Amikacin
- These are effective against:
- Severe infection in the hospital, like coliform bacteria.
- Streptomycin is only effective against:
- Mycobacteria.
- Kanamycin used for:
- Gut sterilization before surgery.
- In leukemias.
- In chronic liver disease.
- Neomycin is used like kanamycin.
- Neomycin can be used as a topical antibiotic.
What is the role of Monobactams?
- These are monocyclic β-lactam antibiotics.
- Aztreonam was available for clinical use.
- These are bactericidal and can be given intramuscularly and intravenously.
- These are effective for:
- Aerobic gram-negative bacteria in:
- Urinary tract infection.
- Septicemia.
- Gonorrhea.
- Aerobic gram-negative bacteria in:
What is the role of Tetracyclines?
- These are:
- Tetracyclin.
- Oxytetracycline.
- Chlortetracycline.
- Doxycyclin.
- Minocycline.
- These are bacteriostatic.
- Inhibit protein synthesis by preventing the attachment of amino acids to ribosomes.
- These are antibacterial for:
- Gram-negative bacteria.
- Gram-positive bacteria.
- Mycoplasma pneumoniae
- Rickettsia.
- Coxiella burneti.
- Chlamydiae.
What is the role of Macrolides?
- Erythromycin is the most common member of macrolides.
- This is bacteriostatic by inhibition of protein synthesis.
- It is bactericidal at higher concentrations.
- This is useful for the treatment of:
- Staphylococcal infection.
- Treating a respiratory infection, tonsillitis, bronchitis, pneumonia, and sinusitis.
- For whooping cough.
- Atypical pneumonia.
- Psittacosis.
- Diphtheria.
- Non-specific urethritis.
- Campylobacter enteritis.
What is the role of Glycopeptides?
- Vancomycin is available and is bactericidal by inhibition of cell wall synthesis.
- It is used for:
- Staphylococcal infection, including resistant strains to methicilin.
- Streptococci but less effective against strep. fecalis.
- For endocarditis.
- Septicemia due to streptococci and staphylococci (coagulase-positive).
- Teicoplanin is related to vancomycin and is used as a single dose.
What is the role of Ciprofloxacin?
- This is a group of new antibacterial agents developed from nalidixic acid.
- This can be given orally and intravenously.
- Its mode of action is that it inhibits DNA-gyrase activity and binds to chromosomal DNA.
- It has a broad spectrum against:
- Aerobic gram-negative bacteria like:
- Pseudomonas. aeruginosa.
- Staphylococcal (including methicilin-resistant strain).
- Aerobes are mostly resistant.
- Used for :
- Respiratory infection due to ps. aeruginosa.
- Chronic urinary infection.
- Gonnorhea.
- Prostatitis.
- Enteric fever and other GIT infections.
- Good for travelers’ diarrhea.
- Skin and soft tissue infections due to PS. aeruginosa.
How will you report of various cultures and sensitivity?
- This depends on the type of culture of bacteria. In the routine, it takes 48 to 72 hours.
- After the growth, sensitivity takes another 24 hours.
- For T.Bacilli, it will take 4 to 6 weeks.
What is the clinical significance of culture and sensitivity (C/S)?
- It will reduce the resistence of antibiotics.
- It will control hospital infection.
- It will avoid unnecessary use of antibiotics.
- It is used in the community for the surveillence.
Questions and answers:
Question 1: How much time do Acid fast bacilli (M. Tuberculosis) take?
Question 2: How much time is needed for sensitivity?

THIS INFORMATION IS SO PRACTICAL
Thanks a lot.
amazing content. Am studying for my lab med final, will use this for future classes as well. Thank you for creating this and helping others
welcome, thanks.
informative article. best wishes for labpedia.
Thanks.
Hi,
My wife is having abdomen puss after her hernia surgery and it is now over 4 months since she is suffering from this. Had multiple pus c/s tests and having medicines / drips since long. Please coordinate with me on my email or WhatsApp so that I can share complete treatment done so far from you.
It is really sad to hear about post-op infection. I think culture and sensitivity should solve the problem. Also, she needs daily good antiseptic dressings.
Hola, cómo o quién determina los antibioticos usados en el antibiograma de disco para los gram positivos, gram negativos y entorobacterias! gracias por su contenido.
You are right. There are so many sites where you can find antibiotics sensitivity.