Cortisol Hormone, Hydrocortisone (AM and PM) and Cushing’s syndrome
Cortisol Hormone
What sample is needed for the estimation of Cortisol Hormone?
- It is performed on serum (3-5 mL of clotted blood to make serum).
- Also, it can be done on plasma.
- Collect the blood at 8 a.m.
- Then, collect blood at 4 p.m.
- The 4 pm value is one-third to two-thirds of the 8 am value.
- The sample can be stored at 4°C for up to 2 days.
- For a longer period, freeze the sample.
- Urine sample: This is a 24-hour urine sample. Add 20 mL of acetic acid (30%) to the container.
- Or preserve with 1 gram of boric acid.
What are the Indications for the Cortisol Hormone?
- This will measure the serum cortisol level.
- Cortisol level is estimated to rule out hypo- or hyperfunction of the adrenal gland.
What are the precautions for Cortisol Hormone?
- There is increased value during pregnancy.
- Emotional and physical stress can increase value.
- Drugs like amphetamine, estrogen, cortisone, oral contraceptives, and spironolactone can increase value.
- Drugs like androgens, betamethasone, exogenous steroids, lithium, danazol, Dilantin, and methyldopa can decrease the value.
How will you discuss the pathophysiology of the Cortisol Hormone?
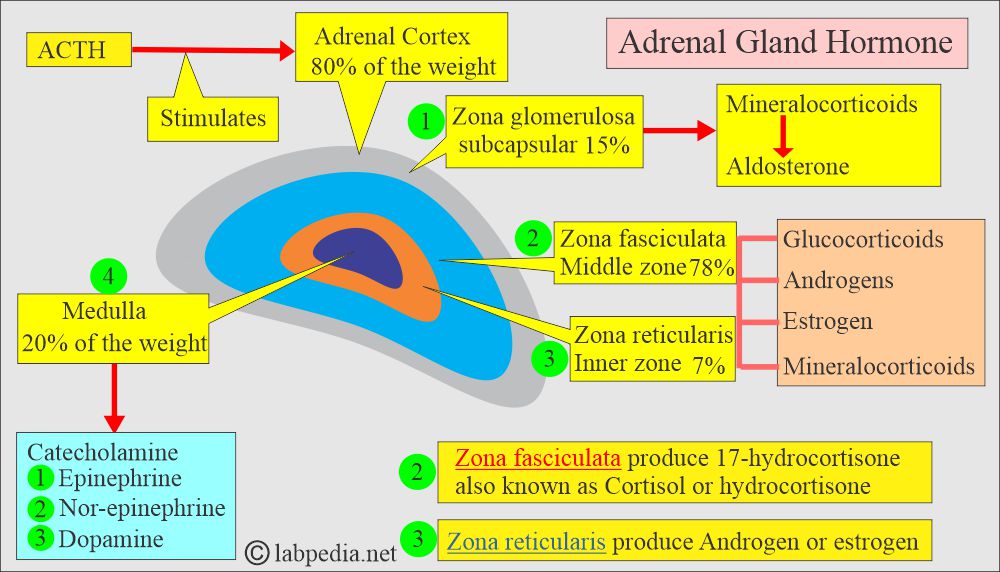
- This is a major adrenal gland glucocorticoid synthesized in the zona fasciculata of the adrenal cortex, and this will control the metabolism of:
- Glucose (Carbohydrate).
- Lipids (fats).
- Proteins.
- The zona fasciculata is the middle zone, and it produces 17-hydroxycortisone, also known as cortisol or hydrocortisone.
- The inner zone is the zona reticularis, which produces androgens or estrogen.
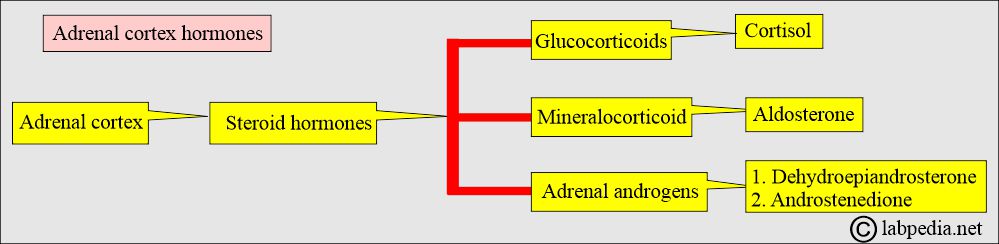
- The adrenal cortex produces a variety of steroid hormones.
- This hormone plays a crucial role in the body’s metabolism.
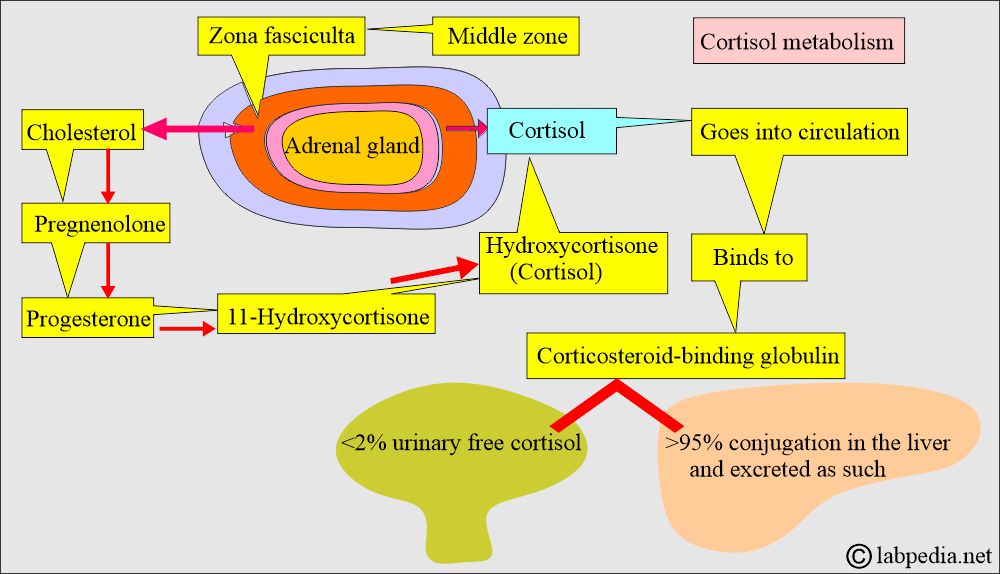
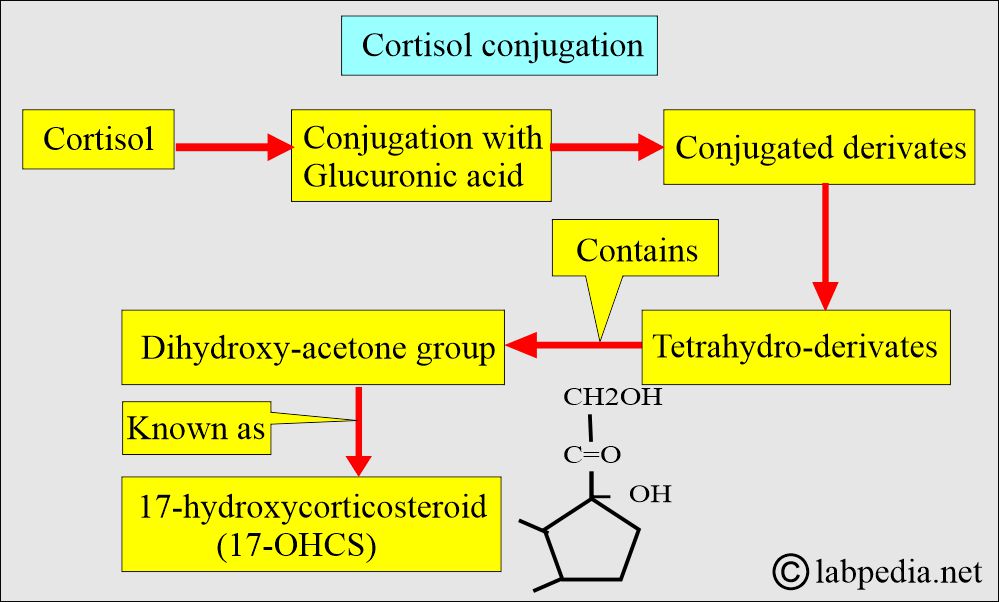
- Cortisone and its oxidation products are inactivated in the liver by two separate reduction processes (hydrogenation) into tetrahydro-derivatives.
- This will conjugate with glucuronic acid in the liver and then be excreted in the urine.
- Cortisol is a steroid.
- Because of its tight binding with Cortisol-Binding Globulin, cortisol is metabolized slowly.
What are the types of Cortisol present in the body?
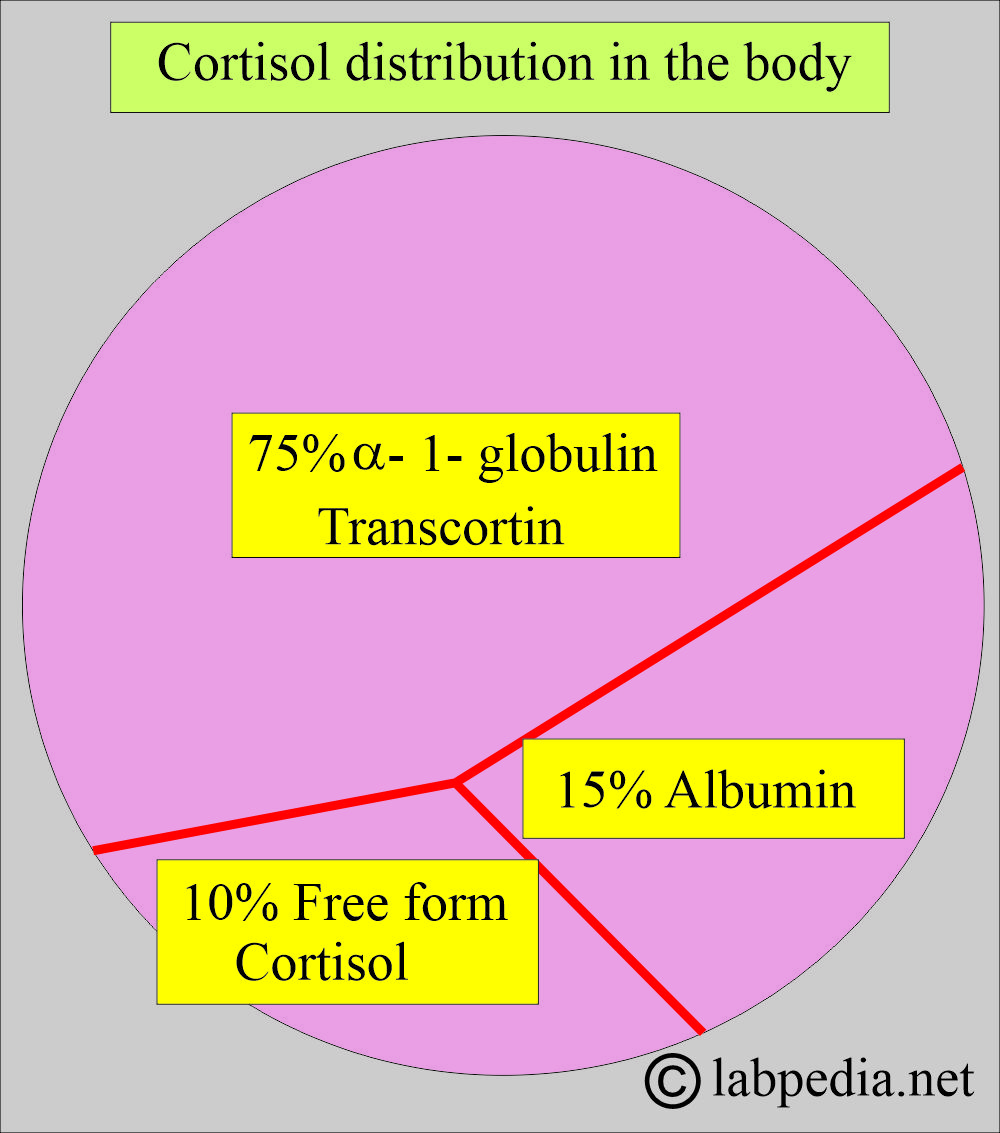
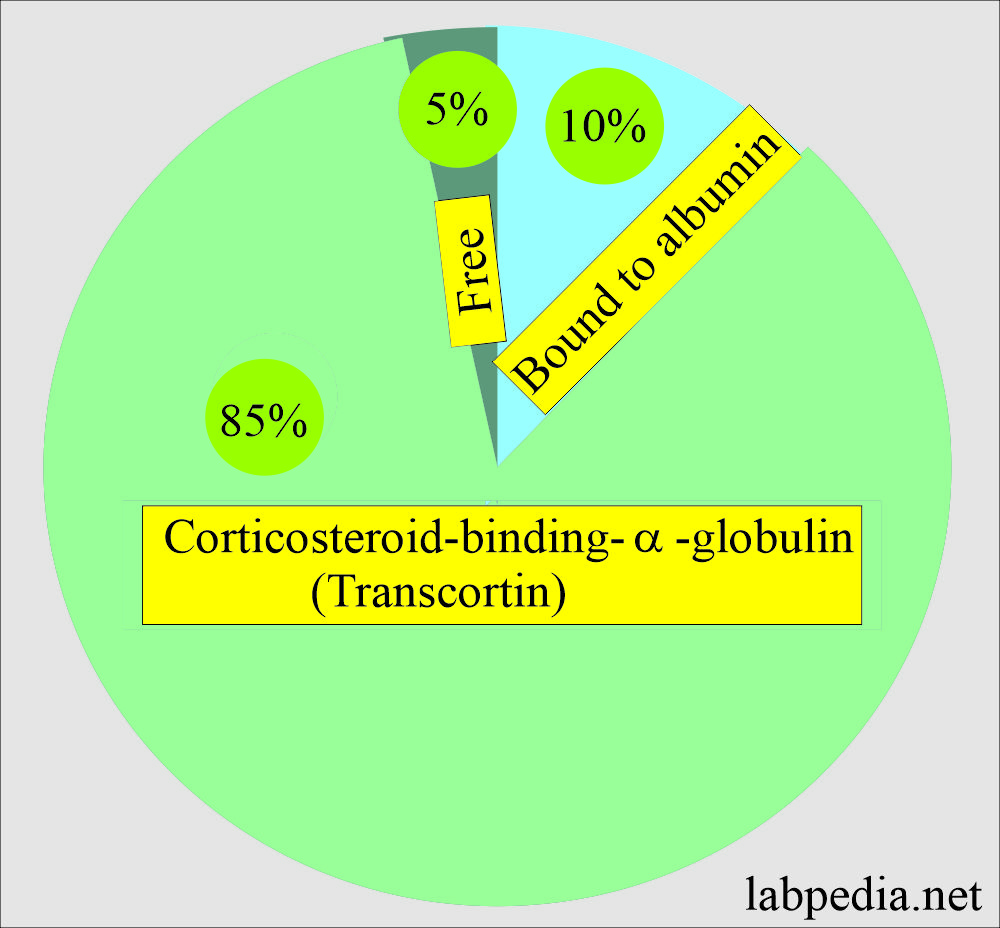
- One of the references gives the following figures.
- 75% is bound to alpha-1-globulins called transcortin.
- 15% is bound to albumin.
- 10% is unbound and is in free form.
- The bound form is not physiologically active.
- The kidney, liver, and thyroid diseases affect the secretion and metabolism of cortisol (adrenal gland steroids).
- Other factors that affect cortisol levels include age, stress, nutrition, estrogen therapy, and certain medications.
- The glucocorticoid hormone is secreted at a rate of 10 to 30 mg/24 hours, influencing carbohydrate metabolism.
- Adrenal Cortisol, roughly 25 mg, is produced in 24 hours, while plasma concentration is 5 to 25 µg/dL.
- Cortisol plays a role in the metabolism of carbohydrates, proteins, and fats.
- Cortisol breaks down the proteins.
- There is an amino acid formation.
- Amino acids are converted into glucose.
- Cortisol is an insulin antagonist.
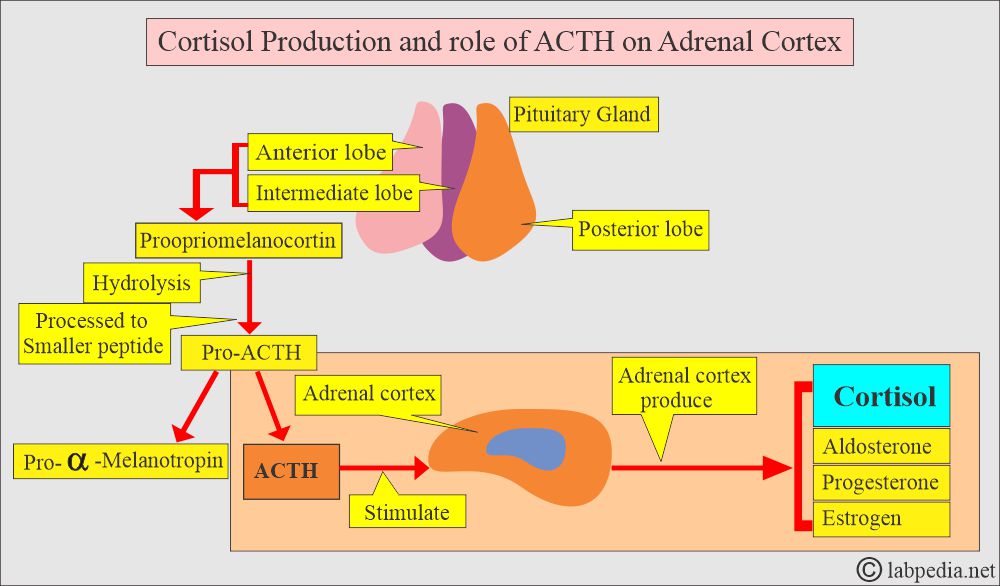
- Cortisol is a glucocorticoid secreted by the adrenal cortex in response to ACTH stimulation.
What is the metabolism of the Cortisol hormone in the body?
- The cholesterol gives rise to cortisol in the adrenal zona fasciculata and reticularis of the adrenal cortex.
- After entering the bloodstream, it binds with corticosteroid-binding globulin.
- Cortisol will be metabolized and conjugated in the liver.
- >95% cortisol metabolites conjugate with glucuronic acid and are excreted in urine as such.
- <2% unmetabolized cortisol is excreted in the urine.
How is the Cortisol hormone transported in the body?
- Another reference gave these figures:
- Freeform.
- Approximately 5% is free.
- Bound form.
- 85% binds the corticosteroid-binding α-globulin (transcortin).
- 10% bound to albumin.
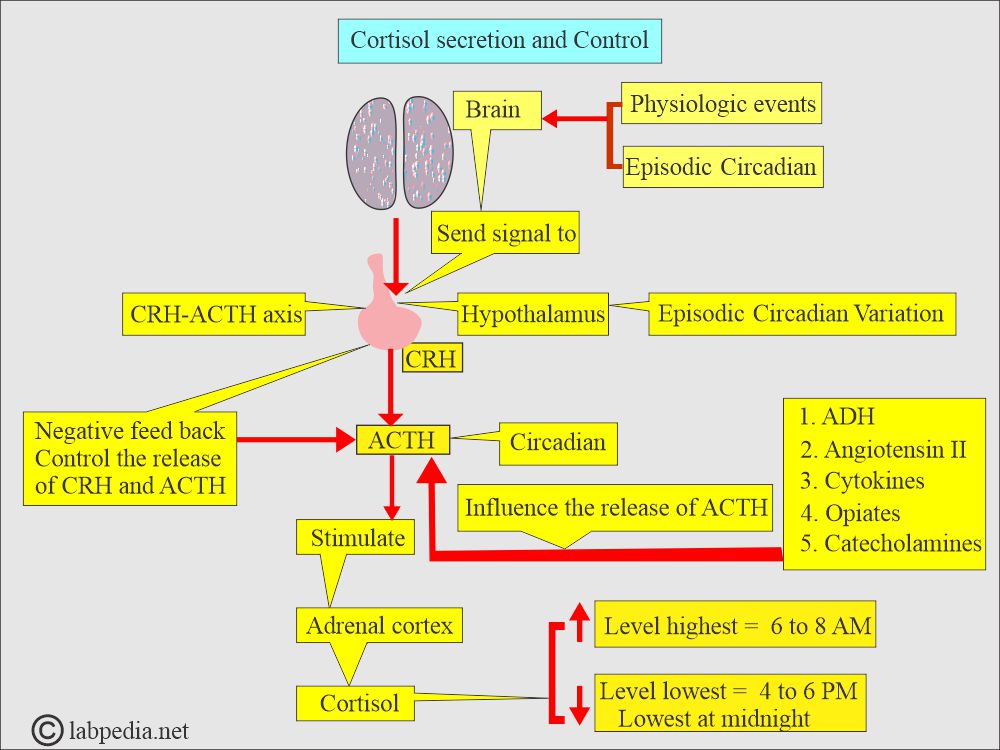
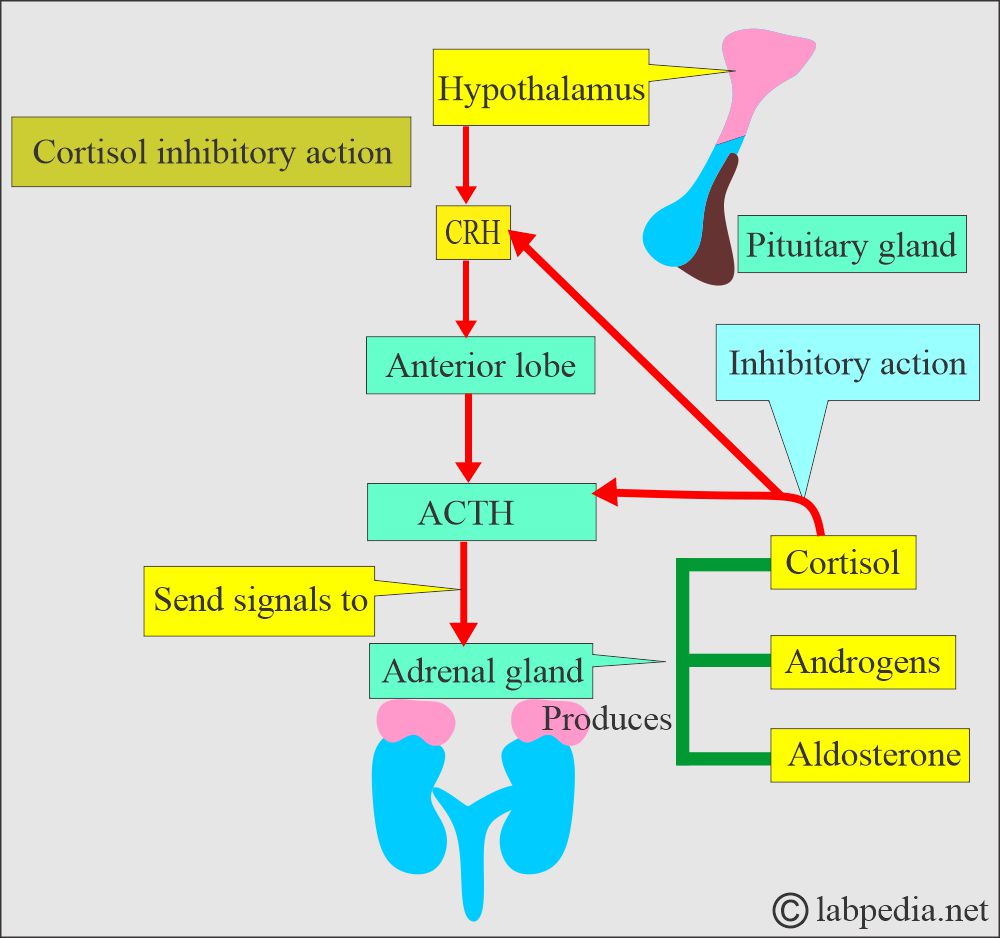
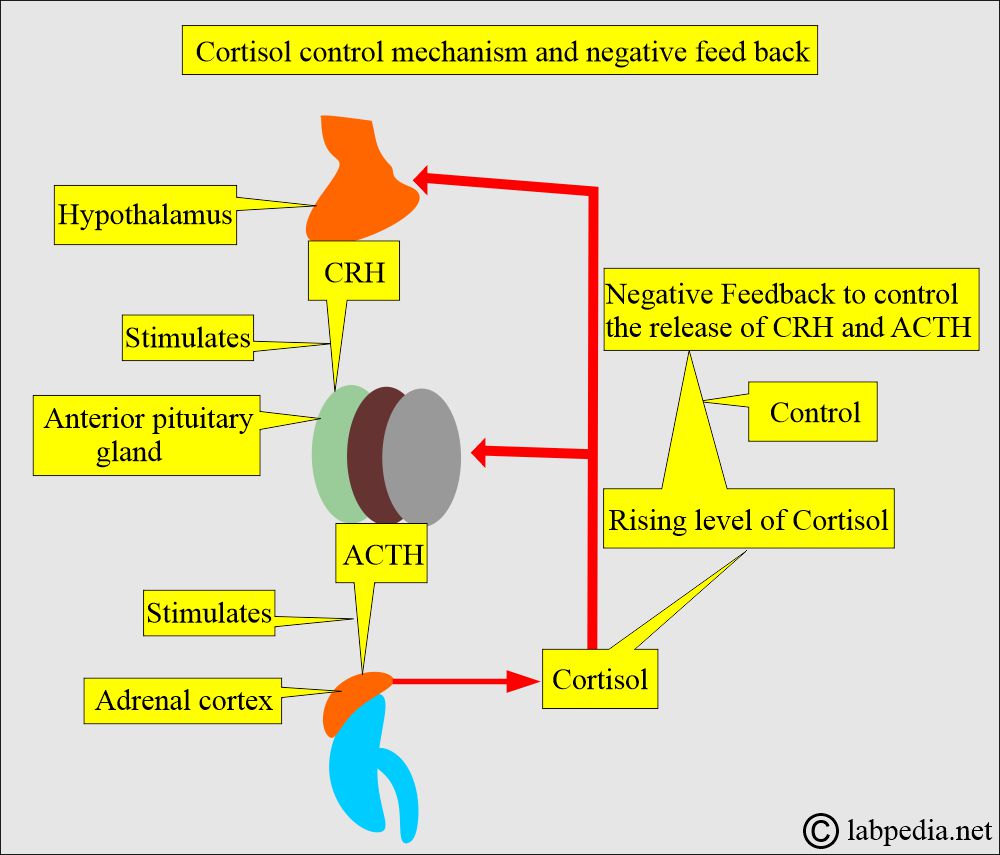
What is the cortisol hormone control mechanism?
- The hypothalamus controls ACTH, as well as Corticotropin-releasing hormone (CRH).
- In the case of increased ACTH, cortisol is excreted within a few minutes.
- Decreased ACTH level leads to the atrophy of the zona fasciculata (and zone reticularis).
- Exogenous glucocorticoids lead to suppression of ACTH and adrenocortical atrophy.
- Corticotropin-releasing hormone ( CRH ), made in the hypothalamus, stimulates the anterior pituitary gland to produce ACTH, which stimulates the adrenal cortex to produce cortisol.
- Cortisol in blood exists in the following forms:
- Cortisol-free.
- Cortisol in total.
- <2% cortisol is excreted unchanged in the urine.
What are the functions of the Cortisol hormone?
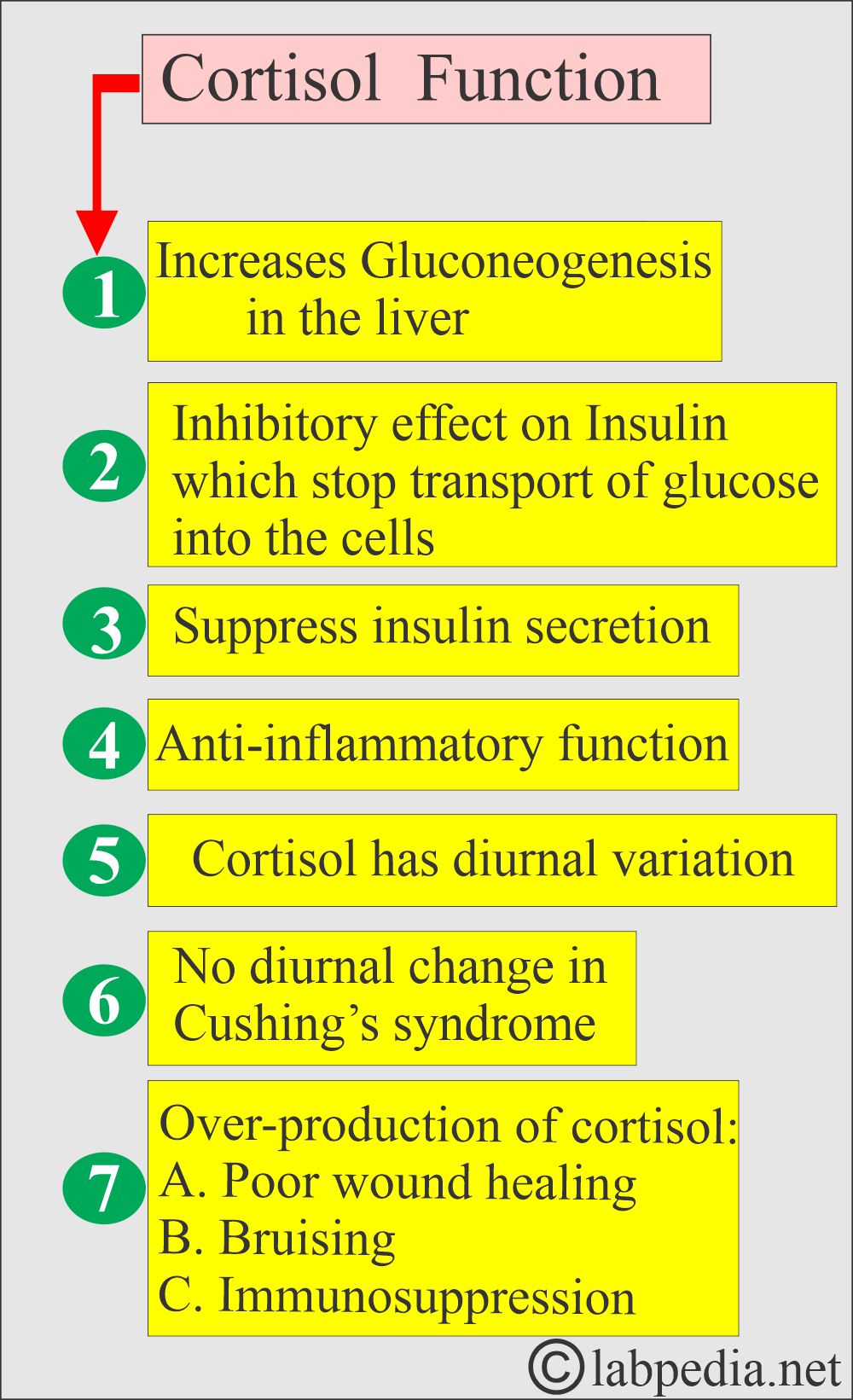
- Cortisol controls the glucose level in the blood:
- By suppressing the secretion of insulin.
- It inhibits the uptake of glucose by the peripheral tissues.
- It promotes hepatic glucose synthesis.
- Cortisol increases glucose levels by increasing gluconeogenesis in the liver (from the glucose store).
- Cortisol regulates the metabolism of carbohydrates, fats, and proteins.
- It has anti-inflammatory properties:
- By suppressing the cytokines.
- It decreases the eosinophils (inhibitory effect on eosinophils).
- It depresses the T-lymphocytes.
- In case of overproduction of cortisol hormones:
- It causes poor wound healing.
- There may be bruising.
- There is immunosuppression during infection.
- Cortisol regulates water-electrolyte balance:
- Water migrates into extracellular fluids through renal excretion.
- Excessive levels of Cortisol cause an accumulation of water in the face and other body areas.
- Cortisol plays a role in the immune system.
- It is influenced by factors such as heat, cold, infection, trauma, exercise, debilitating diseases, and obesity.
What are the conditions under which Cortisol level variations occur?
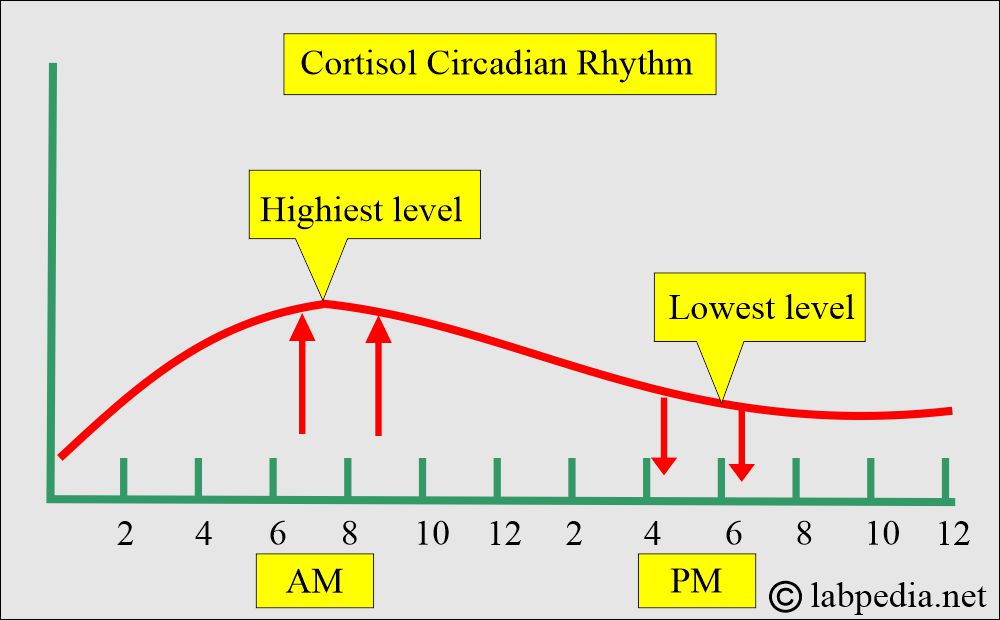
- There are diurnal variations in cortisol secretion, with higher levels in the morning (6 to 8 AM) and the lowest levels between 4 to 6 PM. The level also starts decreasing and reaches its lowest levels at midnight. So, a random sample is not helpful.
- The highest level is between 6 to 8 AM.
- The lowest level is between 4 to 6 PM. (Gradually false during the day, lower between 4 to 6 pm.)
- The lowest level is at midnight.
How will you describe the cortisol variation according to time?
| Cortisol pattern | Cortisol level | Mechanism |
|
|
|
|
|
|
|
|
|
| Significance of the cortisol level |
|
|
- Cushing’s syndrome typically has an elevated morning level.
- Cushing’s syndrome does not show diurnal change.
- There is no decline throughout the day.
- Addison’s disease has the lowest level.
- The variation is lost under stress.
What is the mechanism of Cortisol excretion?
- Mostly >1% of the total cortisol is synthesized daily and is excreted as such in the urine.
- Approximately 30% to 50% appears as glucuronide conjugates, specifically as tetrahydro-derivates of cortisol and cortisone.
- All these compounds contain the dihydroxyacetone group in the side chain, known as 17-hydroxycorticosteroid (17-OHCS).
- There is a higher concentration of these compounds in the urine.
- Chemical estimation of urinary 17-OHCS or 17-ketogenic steroids does not accurately estimate plasma cortisol concentration or output because they may form other steroids with similar structures.
What is the Normal Total cortisol hormone?
Source 2
- Serum AM (8 am) = 5 to 23 µg/dL
- Serum PM (4 pm) = 3 to 13 µg/dL
- Urine (free cortisol) = 20 to 90 µg /24 hours
- Children = 1 to 16 years old.
- 8 AM = 15 to 25 µg/dL
- 4 PM = 5 to 10 µg/dL
- Newborn = 1 to 24 µg/dL
- Maternal at birth = 51.2 to 57.4 µg/dL
- The blood sample was usually taken at 8 am and 4 pm; the 4 pm level is one-third to two-thirds lower than the 8 am level.
- Urine 24 hours
- Adult/old people = <100 µg/dL/24 hours (<276 nmol/day).
- Adolescent = 5 to 55 µg/dL/24 hours
- Child = 2 to 27 µg/dL/24 hours
Source 1
What are the values of total Cortisol (free and bound by RIA)?
| Age | µg/dL | nmol/L |
| Cord blood | 5 to 17 | 138 to 469 |
| Infants 1 to 7 days | 2 to 11 | 53 to 304 |
| Children 1 to 16 years | 3 to 21 | 83 to 580 |
| Adult | ||
| 0080 AM | 5 to 23 | 138 to 635 |
| 1600 PM | 3 to 16 | 83 to 441 |
| 2000 PM | <50% of 0800 AM value | <50% of 0800 AM value |
| Maternal at birth | 54.3 ± 3.1 | |
| Cortisol Free 24 hours of urine | ||
| Child | ||
| 1 to 10 years | 2 to 27/day | 6 to 74 |
| 11 to 20 years | 5 to 55 | 14 to 152 |
| Adult | 20 to 90 | 52 to 248 |
| Serum (free cortisol) | ||
| Adult | ||
| 0800 AM | 0.6 to 1.6 | 1.7 to 4.4 |
| 1600 PM | 0.2 to 0.9 | 0.6 to 2.5 |
- For conversion of µg/dL into SI unit x 27.6 = nmol/L
Source 4
Cortisol Hormone Level
- 0800 AM =5 to 23 µg/dL (138 to 635 nmol/L).
- 4.00 PM = 3 to 16 µg/dL (83 to 441 nmol/L).
- Midnight = <50% of 0800 AM level.
- Newborn = 2 to 11 µg/dL (55 to 304 nmol/L).
- Maternal at birth = 52.1 to 57.4 µg/dL (1413 to 1584 nmol/L).
- After the first week of life, cortisol levels reach adult levels.
What are the conditions where there is an increased level of cortisol?
- Cushing syndrome (Pituitary disease)
- Adrenal adenoma and carcinoma.
- Pregnancy leads to a raised level.
- Physical and emotional stress can increase levels.
- Ectopic ACTH-producing tumors.
- Hyperthyroidism.
- Stress.
- Major depression.
- Severe anxiety.
- Obesity. All steroid hormones are elevated in obese individuals, which may be due to increased deposition or synthesis in fat tissue.
- An extremely high level is seen in Ectopic ACTH syndrome.
What are the conditions where there is a decreased level of cortisol?
- Addison’s disease.
- congenital adrenal hyperplasia ( adrenogenital syndrome )
- Hypopituitarism.
- Hypothyroidism.
Cushing’s syndrome:
What is the definition of Cushing’s syndrome?
- Cushing’s syndrome is characterized by an increase in serum cortisol production.
- Basically, this condition is due to excessive body levels of glucocorticoids like cortisol, and this may be:
- Primary where there is overproduction due to the adrenal cortex.
- The secondary is due to therapeutic therapy.
What are the causes of Cushing’s syndrome?
- Approximately 70% of cases are attributed to the overproduction of cortisol by the adrenal cortex, resulting from pituitary hypersecretion of ACTH, which leads to bilateral adrenal cortex hyperplasia.
- 10% of the cases are due to an adrenal cortex gland adenoma.
- 10% of the cases are due to adrenal cortex carcinoma.
- Around 28% to 38% of the cases are ectopic production of ACTH, like lung small cell carcinoma.
- Few cases are caused by thymus carcinoid, pancreatic islet cell tumors, pheochromocytoma, and various adenocarcinomas.
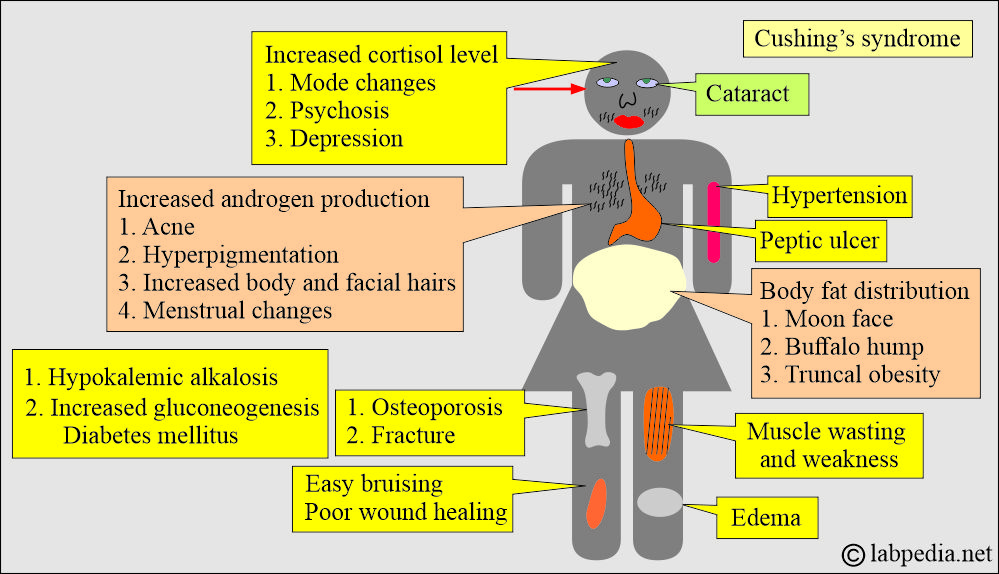
What is the clinical presentation of Cushing’s syndrome?
- Cushing’s syndrome is more common in females, 4 times more than in males.
- There is truncal obesity.
- Neuropsychiatric symptoms.
- There is hypertension.
- There is an intolerance of carbohydrates.
- There is hyperglycemia and decreased glucose tolerance.
- There are polyuria and polyphagia.
- There are hirsutism and acne.
- There are proximal myopathy and weakness.
- The patients are prone to easy bruising.
- There are sexual dysfunction and menstrual problems.
How will you diagnose Cushing’s syndrome?
- There is hypokalemic metabolic alkalosis.
- There is an increase in urinary-free cortisol.
- Single increased serum cortisol level.
- Or advise 24-hour urinary 17-OHCS.
- Measure urine 17-ketosteroids for the diagnosis of Cushing’s syndrome.
- It has increased from 50% to 55% of Cushing’s syndrome patients.
- Diurnal variation is absent in 90% of the cases.
- Take two blood samples, one at 8 A.M. and one at 8 P.M.
- There will be no diurnal variation.
- There is a lake of normal suppression by dexamethasone.
- Low-dose dexamethasone suppression test, where the cortisol level remains elevated.
- A high level of cortisol indicates Cushing’s syndrome.
- A low level of cortisol indicates Addison’s disease.
How will you differentiate Adrenal diseases?
| Disease | ACTH value | Cortisol value |
|---|---|---|
| Cushing’s syndrome causes | ||
| Adrenal adenoma | Low | Raised |
| Adrenal cancer | low | Raised |
| ACTH-producing Pituitary tumor | Raised | Raised |
| Ectopic ACTH (Lung cancer) | Raised | Raised |
| Addison’s disease causes | ||
| Adrenal gland failure (Infarction, Haemorrhage) | Raised | Low |
| Congenital adrenal hyperplasia | Raised | Low |
| Hypopituitarism | Low | Low |
What is the value of urinary cortisol per/day in various diseases?
| Disease | µg free cortisol/day |
| Normal | <100 |
| Adrenal tumors | >120 |
| Ectopic ACTH syndrome | >120 |
| Cushing’s syndrome | >120 |
What is the function of the cortisol hormone?
- It regulates the body’s response to stress.
- Cortisol stimulates the release of glucose from the liver in response to stress.
What happens when the cortisol level is high?
- High cortisol hormone level leads to:
- Weight gain.
- Headache.
- Irritability etc.
- It suppresses inflammation.
- It regulates blood pressure.
- It regulates blood glucose levels.
What is the effect of the cortisol hormone on behavior?
- Excessive levels of cortisol, like in Cushing’s syndrome, lead to depression.
Questions and answers:
Question 1: What is the precursor of the cortisol?
Question 2: When is the cortisol level high during the day?
Question 3: What is the cause of Cushing's syndrome?