Complications during blood collection and Treatment
Complications during blood collection and Treatment
What is the Skin puncture for blood sampling?
- Skin puncture is performed in the pediatric group and among diabetics.
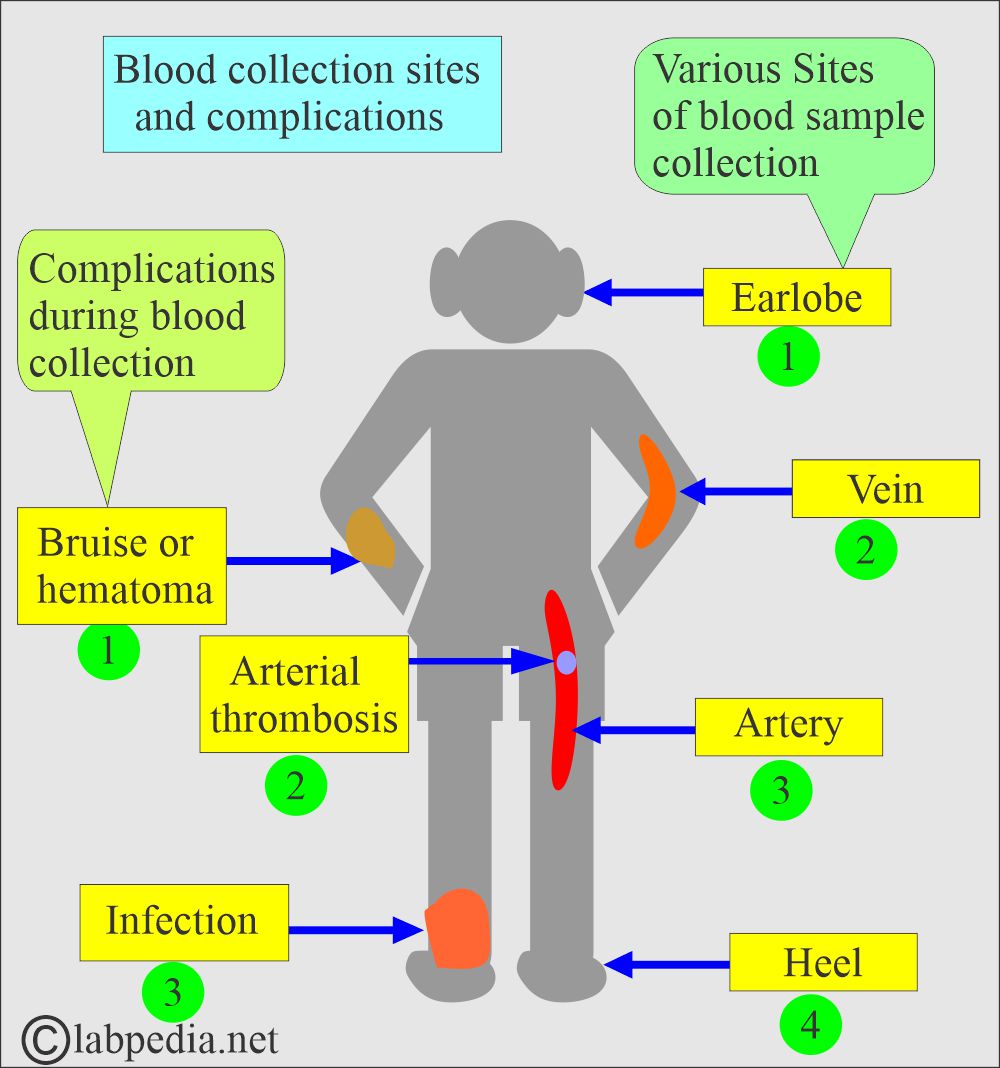
- The common sites are fingertips, heels, and ear lobes. Heels are common sites in children.
- Fingertips are used in adults (diabetics) and small children.
- Earlobes are used as a possible substitute for arterial blood to assess pH, pCO2, and pO2.
What are the complications during blood collection?
- There may be various types of complications of blood collection.
- The following are some of the possibilities:
- Fainting and dizziness.
- Hematoma formation.
- Hypersensitivity reactions.
What are the Complications during blood collection?
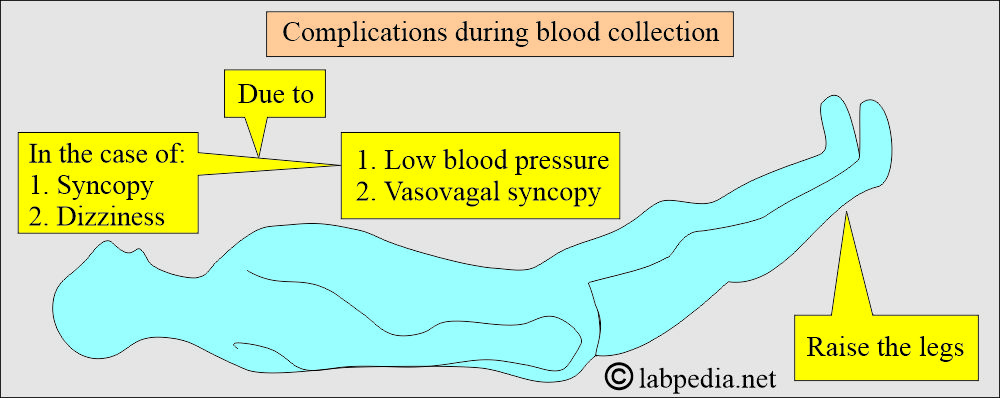
What is the reason for fainting during the collection of the blood?
- Patients may feel dizzy, which can occur during or after blood collection.
- There is a sudden decrease in blood pressure, and sometimes, the patient may temporarily lose consciousness.
- The reason is:
- This is due to vasovagal syncope.
- Please don’t leave the patient alone and refrain from allowing them to drive for another 30 minutes.
- Immediately lie the patient flat and raise their legs.
What is the reason for Hematoma formation?
- There is a leak of blood from the venipuncture site.
- There may be a bruise formation.
- Hematoma forms when:
- The needle is inserted into a small vein.
- It may pass through the vein.
- The needle is partially in the vein.
- The needle was removed while the tourniquet was still in place.
- Not adequate pressure was applied after the venipuncture.
- Blindly searching the vein.
- What is the treatment of a hematoma?
- Apply the pressure bandage to the area.
- The patients on anticoagulant therapy:
- These patients have a higher risk of bleeding.
- In these patients, keep pressure on the venipuncture site and don’t leave it until the bleeding has completely stopped.
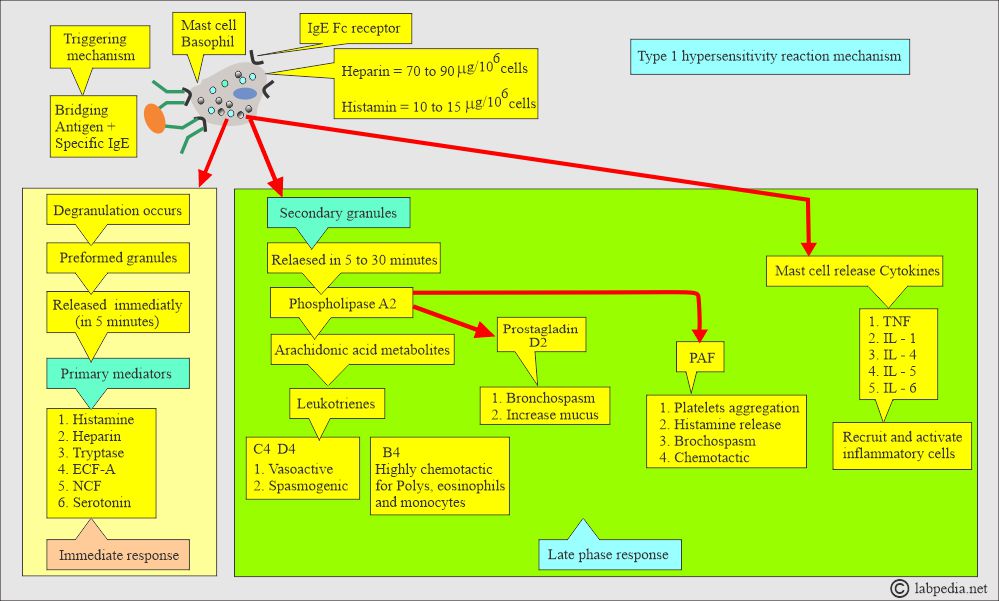
What type of Hypersensitivity Reactions are seen during blood donation?
- Allergies:
- There may be reactions to the antiseptic, band-aids, bandages, or latex.
- If it happens, give some antiallergic medication.
- Some patients may develop Type I hypersensitivity reactions just seeing their own blood.
- The patient will exhibit a typical picture of a type 1 hypersensitivity reaction.
- All symptoms are due to histamine or histamine-like substances produced in this hypersensitivity reaction.
- The patient may have an anaphylactic reaction, and this may be:
- Localized.
- Or a systemic reaction.
What are the chances of Infections during blood donation?
- The infection is more common in patients who are immunocompromised.
- Advise the patient to look for redness, pain, swelling, or tenderness.
What is the outcome of Pain due to nerve involvement during blood donation?
- The patient may experience sharp pain and tingling due to nerve involvement.
- It is best to take out the needle.
- Sometimes, permanent nerve damage can occur.
What are the causes of Phlebitis during blood donation?
- This is a rare complication that can occur after blood collection.
What are the chances of sepsis during blood donation?
- This is another rare complication of blood collection.
What is the Presentation (sign/symptom) of the patient during blood collection?
- Nervousness.
- Itching of the skin.
- A feeling of confusion.
- Nausea, vomiting, and diarrhea.
- Abdominal or back pain.
- There will be flushing, pallor, or cyanosis.
- Urticaria.
- Laryngeal edema leads to stridor.
- Tachycardia.
- There is low blood pressure.
- Convulsions.
- Respiratory depression.
- Bronchospasm leads to an asthmatic attack.
- Treat the patient for a type 1 hypersensitivity reaction.
What is the Treatment of blood collection complications?
- Treatment of blood collection complications:
- If the patient becomes faint, stop the blood-taking procedure and lie the patient down with a raised foot end.
- Remove the needle and reassure the patient.
- Talk to patients.
- Please don’t allow him to drive for another 30 minutes.
- Offer the patient juice or water.
- Ask the patient to breathe slowly (deep breathing).
- If a hematoma appears, remove the needle and apply pressure for two minutes.
- Remove the tourniquet.
- In patients with petechiae, ensure that there is no bleeding before the patient leaves the laboratory.
- In such patients, there are coagulation problems.
- There may be excessive bleeding in patients on aspirin or anticoagulation therapy.
- Don’t leave the patient until there is a complete stoppage of blood flow from the venipuncture site.
- If the patient feels sharp electric pain, immediately remove the needle.
- In case of an arterial puncture:
- Immediately remove the tourniquet.
- Hold pressure at the site for at least 5 minutes or till the bleeding stops.
- Check the pulse and blood pressure.
- In the event of a hypersensitivity reaction, administer antihistamines.
- Can give steroids.
Question 1: If the patient becomes faint, what should you do immediately?
Question 2: If a patient gets sharp pain, what should you do?

I have had several blood draws in the past couple weeks and my blood squirts and gushes out after the needle withdrawl, all over me , the floor and the wall! Phlebotimost insists I must be on anti-coagulant, but I am not. When I was on a blood thinner years ago, I never had excessive bleeding. Could this be an indication of a medical problem? Normally, I have one tiny spot on the cotton and never bleed anymore. It happened tonight in the ER and then, when I stood up after 2+ hours, it gushed again out from under the bandage that had been tightly wrapped and was all over me and the floor. They added an additional wrap on the site. This is extremely unusual for me and I have been ill recently; tonight my entire body was hugely swollen, including all extremeties, face, abdomen, etc. I weighed 18 bls more than I did on hosp discharge a week ago and have eaten very little because I have had an infected, tender tooth. I have been on 800 mg Amoxocillin and 500 mg Ibuprofin. I’m sorry to go on, but I can’t get anybody to tell me why this would happen and I am concerned. This has NEVER happened before. A response would be appreciated and directing me to the proper kind of doctor to find out what is going on. At the ER, I was told nothing is wrong on any of the lab, x-ray, ultrasound and CT, but the Dr never listened to my heart, never touched any of the huge swelling to see how long it takes the indentation to come back. With the 18 lbs, you can imagine how swollen I am. I have now developed sores (pussy) on the top of my feet; one very pussy so far. (Help! please) I need to know what to do. Thanks for “hearing” me. Oh, I am a 74 yr old female with many problems.
I will suggest doing a bleeding profile like CT, Bleeding time, PT, APTT, INR, and platelet count, including a complete blood picture. Also, do ANF to rule out autoimmune phenomenon. Next, consult a good hematologist. I hope these investigations will help to reach the cause of the problem.
Sorry to hear about your illness. I will suggest to workup for bleeding profile like bleeding time, clotting time, APTT, INR, Complete blood count, including platelets count.
Also, consult some good hematologists.
Hello
During blood drawing, when you feel a burning sensation on your forearm radiating to your wrist is needle touching a nerve. Does the nerve heal after? When do you usually get symptoms after such incident?
Thank you
I will suggest that as the patient feels pain and tingling, please take out the needle immediately if there is damage to the nerve, as the nervous system does not regenerate. Ideally, take out the needle immediately.
Hi, Is it normal to have lump and redness around puncture site?
No, it looks like the inflammatory process has started.
Hi, I inadvertently punctured the artery while doing a venipuncture. I immediately removed the tourniquet and applied pressure. There was no bleeding and the patient is fine. Should I be concerned?
Hi, If you inadvertently punctured the artery while doing a venipuncture and immediately removed the tourniquet and applied pressure. Hence, there was no bleeding and the patient is fine. Should you be concerned?
Definitely you have to look after the patient. Keep the pressure for as long as you are sure that there is no bleeding. Better keep the patient in the lab until you are sure there is no bleeding. Before the patient leaves the lab, apply a pressure bandage and then send him.
Hi there
Great article about Complications during blood collection and Treatment. Thank you for uploading useful article.
https://selftestdiagnostics.com/
Thanks for the appreciation.
I am a regular blood and plasma donor with 88 donations to date.
Recently I have been having issues with “blood spurts” when the attendant is inserting the needle (needle size has not been changed). This has happened 4 times now. I also have recently been diagnosed with hypertension, but was told I’m still good to donate as long as I’m below 180/100 and I feel well at the time I’m donating.
Note: after the first instance I have been warning the tech each time, and yet it’s still happening.
Could this relatively new occurrence be due to hypertension, and if so, am I REALLY still safe to continue with blood/plasma donations?
Please let me know the age. That is very important.
Donors can donate their blood at intervals of 8 weeks.
Healthy individuals can donate blood every 5 to 7 days for a limited period, around 1 to 2 months.
In the above donor, an iron supplement is needed.
High blood pressure or hypertension is one of the leading risks for heart attacks and there is evidence that regular blood donations may be beneficial. Being a regular donor may help with blood flow and reduce arterial blockages. High iron stores can increase a person’s risk of heart attacks.
Hello, really hoping you can answer my question! I was performing a blood draw and the site began to bleed while the needle was still in the patient’s arm and the tubes continued to fill. The patient was a very tough stick, so I maintained the site through 5 SSTs and 1 LAV tube, had a mess at the end of it all. Why did this happen? What did I do wrong? What should I do to improve? Thank you!!
I think you have punctured the vein, that may be the reason for bleeding. The other reason may be that the patient has the bleeding disorder.
Hi, I would like to know what causes the inability to draw blood out of a single vein after quiting injection for 2 weeks, yes, I know drugs is bad, I just don’t know what the cause is, even nurses or doctors can’t even pull blood, im diabetic that won’t help, my sugar lvls are oke, so is my blood pressure, heart rate to high after little exercise or movement, 160 beats per minute, and then all of a sudden this will go away( i hope?) like last time and then i could pull in seconden and be done in seconds, you have any idea?
Actually, when one prick is failed, then that vein will be collapsed and not possible to get blood from that area. There is no worry about that. I think your veins might be narrow and difficult to make those visible. You can try some expert phlebotomist.
I had a blood test last week which went smoothly. When the needle was withdrawn there was no bleeding and a gauze dressing was applied. A few minutes later my dressing was bloody and when replaced there was a small haemotoma lump at the puncture sight. This went down leaving a small bruise. After the bruising faded I have been left with a tiny lump and if I press it a bruise appears. I get a slight ache from time to time. Is it anything to worry about or will it settle down?
You need blood workup for bleeding disorders. You can have bleeding time, clotting time, APTT and PT. These parameters should be normal. These tests will rule out any bleeding disorders.