Complement, C3 and C4, Acute Phase Protein
Complement, C3 and C4
Acute-phase protein (Acute Phase Reactants)
- Acute-phase protein is raised in inflammatory conditions.
- When there is an increase in a protein called positive acute-phase protein.
- In the case of a decrease in the acute phase protein, it is called negative phase protein.
- The acute phase proteins (positive) are proteins whose concentration increases in the plasma, and after the disease episode is over, then it decreases and may become normal.
Complement C3 and C4
What sample is needed for Complements?
- The patient’s venous blood is needed to prepare the serum.
- This can be done on EDTA plasma.
What are the indications for the complement, C3, and C4?
- Advised to diagnose angioedema.
- To monitor:
- The patient with systemic lupus erythematosus nephritis.
- In post-streptococcal nephritis.
- In membranoproliferative nephritis.
What are the precautions for a complement?
- C3 is very unstable at room temperature.
- It is advised to do the test immediately.
- Or freeze at -70 °C.
How will you define the complement system?
- The serum complement system is an important enzyme system that consists of 10% of the serum globulins.
- The complement system has many activities, some of which are still unknown.
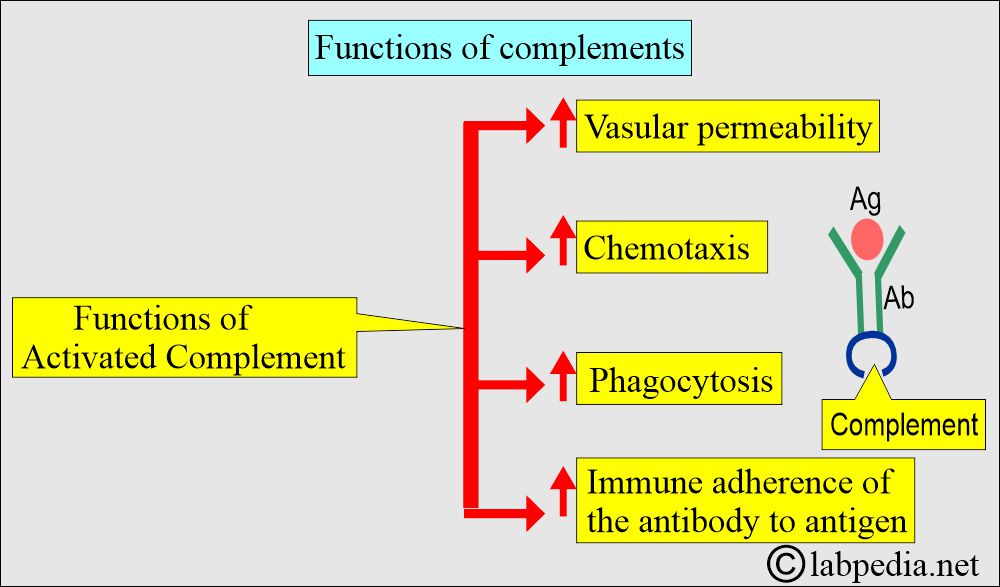
- Increase vascular permeability.
- Leads to chemotaxis.
- Give immune adherence.
- Helps in phagocytosis.
- Ultimately, immune cell lysis.
How will you discuss the Pathophysiology of the complement system?
- Complements are a group of globulin proteins that act as an enzyme.
- These enzymes facilitate immunological and inflammatory responses.
- These are heat-labile plasma proteins.
- These consist of at least 14 proteins, which have a biological function in the immune system. The more common complements are labeled as C1 to C9.
- Besides the major components (C1 to C9), subcomponents and inhibitors are involved in the system.
- The complement acts as an enzyme.
- This will help in the immunologic response and inflammation.
- They help in the chemotaxis and activation of the WBCs.
- There is an increase in vascular permeability, allowing the Antibody and the WBCs to be delivered at the site of the immune complex (Ag+Ab).
- Complement plays a crucial role in the process of phagocytosis and the immune adherence of antibodies to antigens.
- The complement activation leads to the lysis of the antigen or the bacteria.
- The complement is the biological amplifier.
- First, there is the activation of a few molecules of C1q.
- In the next stage, more and more molecules are activated.
- In the final stage, there are thousands of molecules.
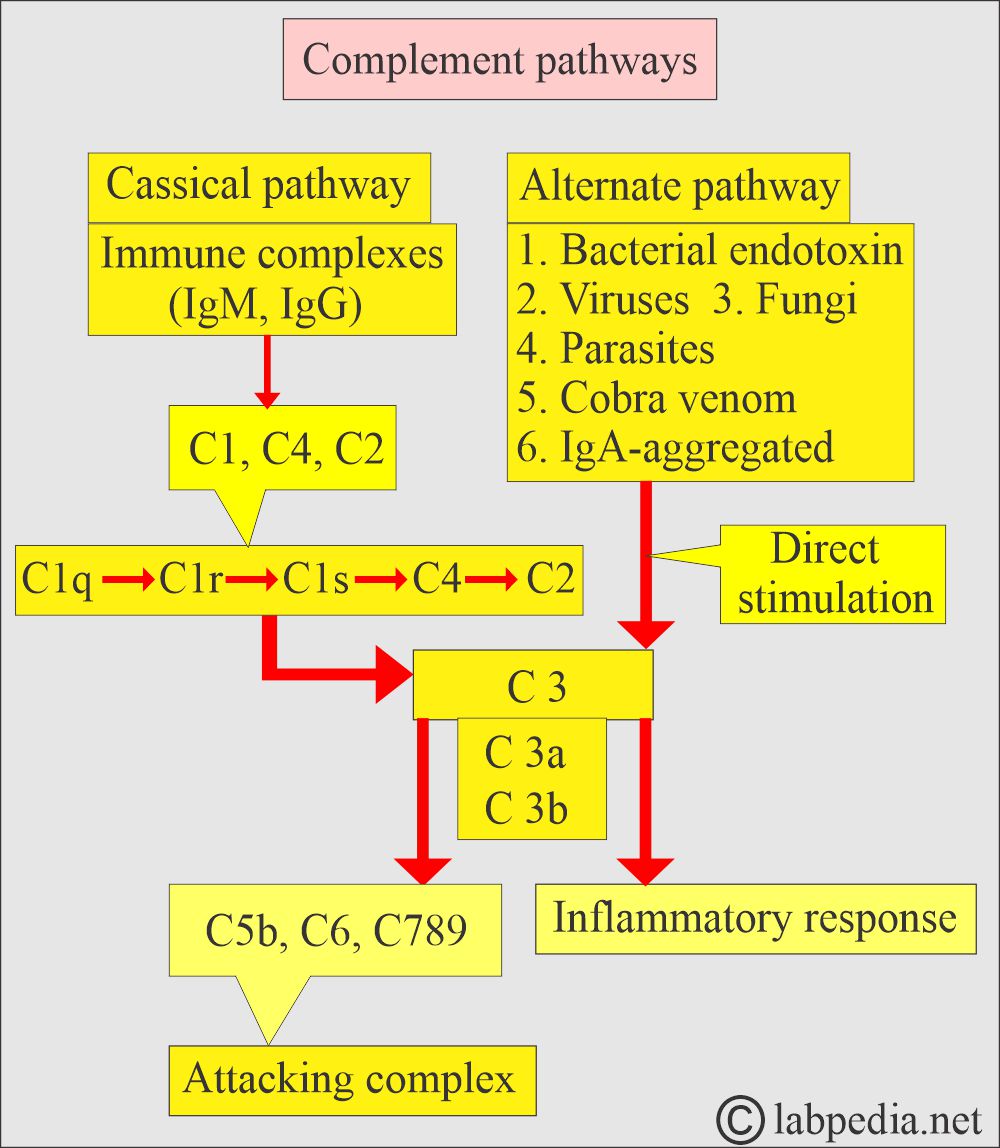
- The classical pathway is activated by C1, and ultimately, there is the activation of C1 to C9.
- In the alternate pathway, there is a bypass of the C1q and direct activation of C3.
- The alternate pathway may be activated by IgA.
- This is activated in the absence of the antibody.
- Polysaccharides of the bacterial cell wall can activate C3 and lead to the destruction of the bacteria.
- In the case of antigen and antibody complexes, the complement is consumed, leading to decreased complement.
What are the causes of Complement deficiency?
- Congenital angioedema. There is a congenital lack of a C1 -inhibitor, often called C1 esterase.
- The Complement system is activated, and the complement is consumed or used up, leading to a fall in the complement level.
- The acquired decreased level is seen in chronic diseases where there is the presence of Ag+Ab complexes, leading to overactivation of the complement system, which consumes complement, and there is a fall in the level of complement, e.g., serum sickness, infectious endocarditis, lupus erythematosus, vasculitis, and glomerulonephritis.
- A decreased level of C4 suggests some defect in the classical pathway.
- A decreased C3 level with a normal C4 level suggests an abnormality in the alternate pathway.
Complement C3:
How will you define Complement C3?
- The C3 molecular weight is 185 kDa, with a normal serum level of 1,200 µg/mL.
- C3 is an acute-phase protein; serum level increases by 30%.
- C3 chromosomal location is 19 p 13.2-13.3.
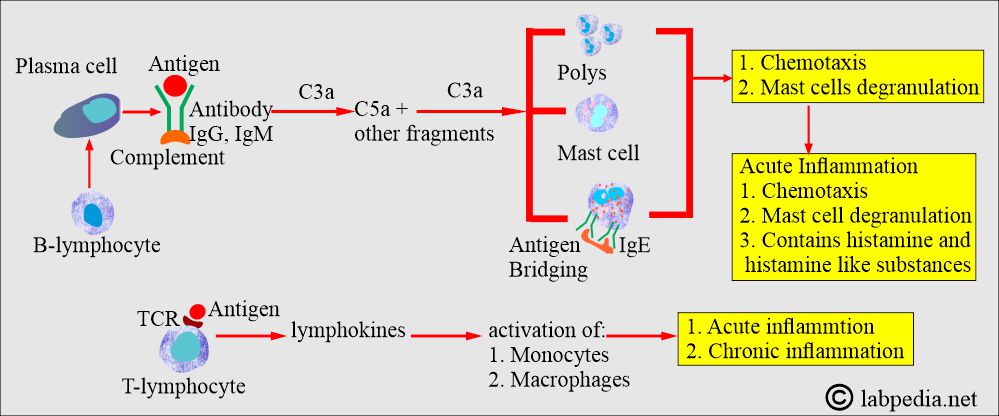
- C3, after activation, is converted into C3a and C3b.
- C3a is an anaphylatoxin that binds to mast cells, triggering the release of histamine and other mediators.
- This will lead to vasodilation, erythema, and swelling.
- This will also lead to bronchoconstriction.
- C3a, when injected into the skin, leads to a wheel and flare.
- C3b attaches to the antigen-antibody complex through the C3b receptor on the inflammatory cells and leads to its adherence to the following:
- Neutrophils.
- Basophils.
- Eosinophils.
- Monocytes.
- This will lead to enhanced opsonization of the antigen-antibody complex and phagocytosis.
- C3 b-coated particles also activate B-lymphocytes to produce antibodies.
- In the early phase of viral infection, C3b leads to the neutralization of the viruses when the antibody level is limited.
- C3 has a vital role in the classical and alternative pathways.
- This is a major opsonin after activation, mainly by C3b.
What are the uses of C3?
- C3 is also an acute-phase protein.
- C3 use helps in screening classical and activation of alternative complement pathways.
- C3 may increase in subacute inflammation, biliary obstruction, corticosteroid therapy, and nephrotic syndrome.
- C3 may be decreased in immune complex diseases, especially SLE (lupus nephritis), Acute poststreptococcal glomerulonephritis, massive necrosis, tissue injury, viremia, sepsis, in infants, hypercatabolism, and hereditary deficiency.
- It may be used in the monitoring of SLE.
Complement C4:
How will you define complement C4?
- C4 has a highly pleomorphic gene located in the HLA complex chromosome 6 (chromosome 6p21.3).
- C4 has a molecular weight of 200 kDa and a normal serum level of 600 µg/mL.
- As an acute serum phase protein, an increase of 34% occurs.
- Partial deficiency of the C4 predisposes to SLE.
What are the uses of C4?
- It may be decreased in immune complex diseases, e.g., SLE.
- It may be decreased in hereditary deficiency, acute GN, infants, hereditary angioneurotic edema, and when the classical pathway is activated.
- Normal C3 and decreased C4 indicate C4 deficiency in hereditary angioedema, SLE, and malaria.
- Decreased C3 and C4 indicate active viral hepatitis and immune complex disease.
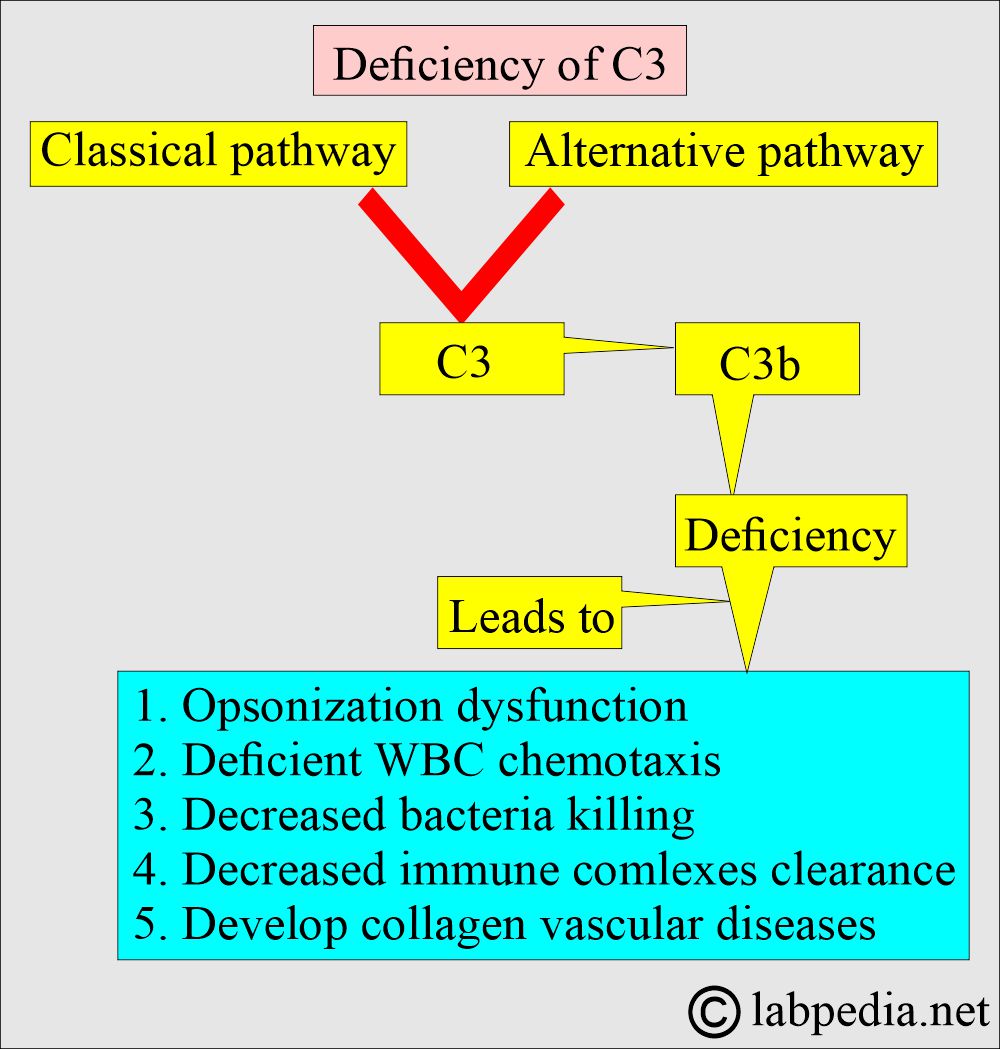
What is the presentation of a deficiency of complement C3?
- Any decrease in C3b leads to defective opsonization.
- In C3b deficiency, Neisserial infections are very common.
- In the case of deficiency, there are recurrent pyogenic infections, particularly due to encapsulated bacteria.
- When it occurs in childhood, then there is a recurrent bacterial infection, mainly by the gram-negative bacteria, such as:
- Neisseria meningitidis.
- Enterobacter aerogenes.
- Escherichia coli.
- Haemophilus influenzae.
- Infection with gram-positive bacteria may also occur.
- C3 deficiency may cause:
- Upper and lower respiratory infections, including pneumonia.
- There are episodes of sinusitis.
- Tonsillitis.
- Otitis media.
- 26% of C3 deficiency patients may develop an autoimmune complex disease like systemic lupus erythematosus.
- Approximately 26% of patients with C3 deficiency develop membranoproliferative or mesangiocapillary glomerulonephritis.
What are the causes of deficiency of C4a and C4b?
- Scleroderma.
- IgA-associated nephropathy.
- Diabetes mellitus.
- Chronic hepatitis.
- Membranous nephropathy.
- Henoch-Schonlein purpura.
- A complete deficiency of C4 is rare.
What is the normal level of total complement?
- Total complement = 75 to 160 units/mL
What is the normal level of C3?
Complement C3
- Cord serum = 65 to 111.8 mg/dL
- Children = 86.6 to 135.8 mg/dL
- Adult = 83 to 177 mg/dL
Source 2
- C3 = 55 to 120 mg/dL
What is the normal level of Complement C4?
Source 1
- Cord serum = 13.7 to 44.9 mg/dL
- one month = 27.5 to47.3 mg/dL
- 6 months = 30.5 to 58.7 mg/dL
- Adult = 28.7 to 67.5 mg/dL
Source 2
- C4 = 20 to 50 mg/dL
- (Values vary from different sources)
What are the causes of decreased levels of complement (C1 to C9)?
- Congenital as seen in angioedema.
- Autoimmune diseases like SLE, serum sickness, rheumatoid arthritis, Sjogren’s syndrome, and lupus nephritis.
- Malnutrition.
- Cirrhosis.
- Hepatitis.
- Acute kidney transplant rejection.
- In the case of septicemia (sepsis).
What are the causes of increased levels of complements (C1 to C9)?
- Acute rheumatic fever.
- Ulcerative colitis.
- Acute myocardial infarction.
- Malignant tumors.
What is the value of acute-phase proteins in acute and chronic inflammation?
| Acute-phase proteins | Acute Inflammation | Chronic Inflammation |
| Albumin | decreased | decreased |
| Prealbumin | decreased | decreased |
| CRP | increased | increased |
| Alpha-1-antitrypsin | increased | increased |
| Ceruloplasmin | increased | increased |
| Haptoglobin | increased | increased |
| Transferrin | decreased | increased |
| Fibrinogen | increased | increased |
| Complement (C3) | increased | increased |
Give examples of Positive and Negative acute-phase proteins?
| Positive acute-phase proteins | Negative acute phase proteins |
|
|
|
|
|
|
|
Questions and answers:
Question 1: What infection is common in case of C3 deficiency?
Question 2: In which autoimmune disease C4 decreases?