Complement C3, (C3 Assay)
Complement C3, (C3 Assay)
What sample is needed for complement C3?
- It is performed on serum.
- Or plasma (EDTA) of the patient.
- The assay should be done immediately, or store the sample at -70 °C. Because C 3 is a very unstable protein at room temperature.
- It can be stored at 4°C for a short period.
- No preparation is needed.
- A random sample can be taken.
What are the Indications for complement C3?
- A complement test may be used to monitor patients with an autoimmune disorder and see if treatment for that condition is working. For example, patients with active lupus erythematosus may have lower-than-normal complement proteins C3 and C4 levels.
- To diagnose angioedema.
- This is done to monitor the activity of the disease in a patient with Systemic lupus erythematosus (S L E), Nephritis, membranoproliferative, and post-streptococcal Nephritis.
What are the precautions for the estimation of C3?
- The value will be low if the sample is left at room temperature, even for one hour.
- After getting the blood, try to separate the serum as soon as possible and freeze it for storage.
How will you discuss the pathophysiology of the complement system?
- A complement is a group of globulin proteins, and these act as enzymes.
- These enzymes facilitate the immune system and trigger the inflammatory response.
- These are circulating glycoproteins that promote inflammation.
- The complement system is important in destroying the foreign body, even cells (Antigens).
- Complement identifies and destroys foreign cells and microorganisms through lysis, opsonization, or the attraction of phagocytic cells.
- The complement consists of a group of 25 proteins, designated C1 to C9, and their subunits.
- These are present in the serum and give a nonspecific inflammatory response to various antigens.
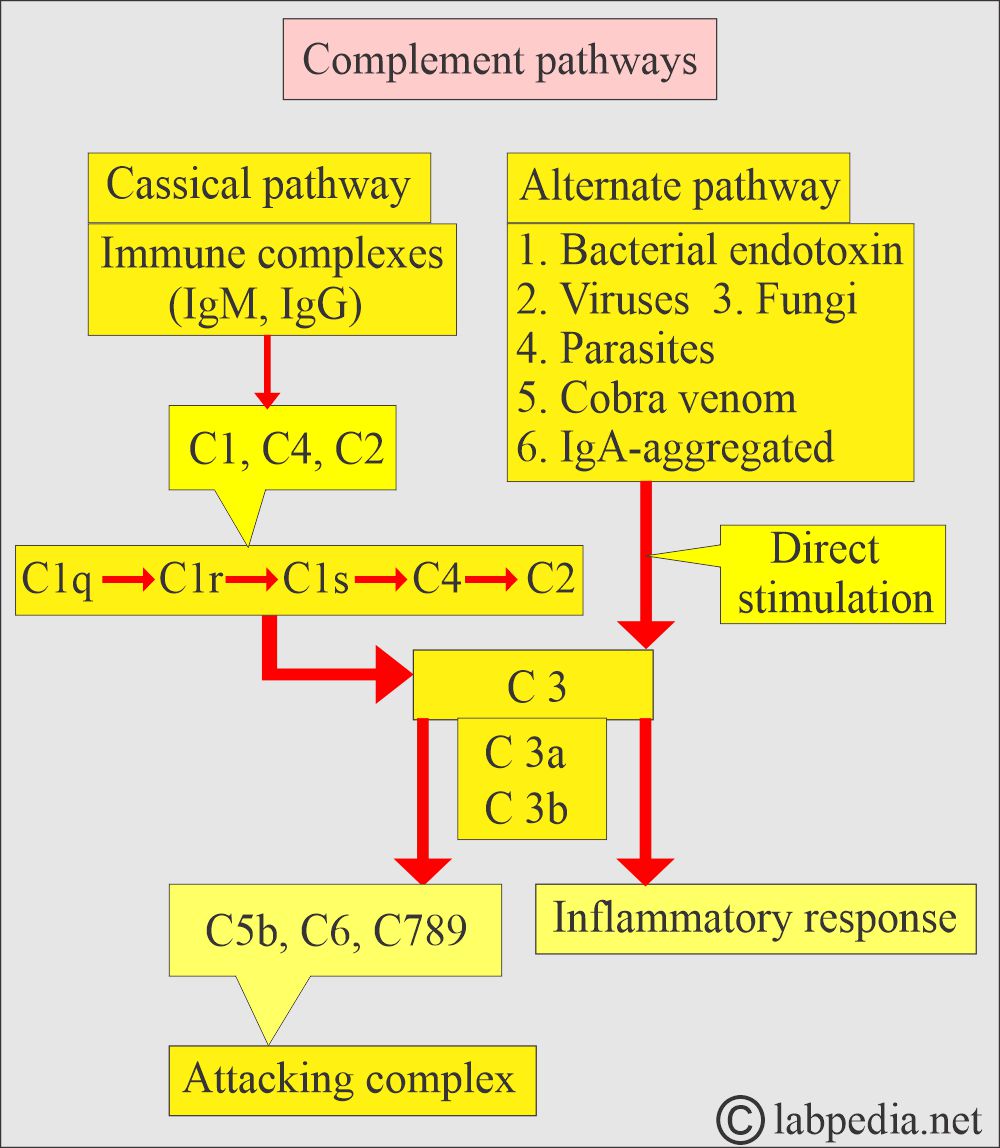
The classical pathway of Complement:
- The classical pathway may activate the complement, where immunoglobulin IgM and IgG activate complement C1 and ultimately, C8 and C9.
- The antigen-antibody complex, either IgM or IgG, binds to C1q and then enzymatically initiates a chain reaction that activates C4, C2, C3, and ultimately C8 and C9.
Alternative pathway of the complement system:
- Where there is direct activation of C3, and the same chain reaction leads to the activation of C8 and C9.
- There is direct activation of C3, and a bypass of factors 1, 2, and 4.
- These two complements (C8 and 9) cause damage to the membrane of antigens and destroy them. These act like drill machines.
- The activated C3 attracts inflammatory cells to the site ( chemotaxis). And also increase vascular permeability.
What does complement C3 indicates?:
- Complement is part of the immune system, and particularly, C3 is very significant in preventing infections and gives rise to the inflammatory response.
- C 3 is considered the heart of the system.
- Complement C3 is a blood test that measures the activity of a specific protein component of the complement system.
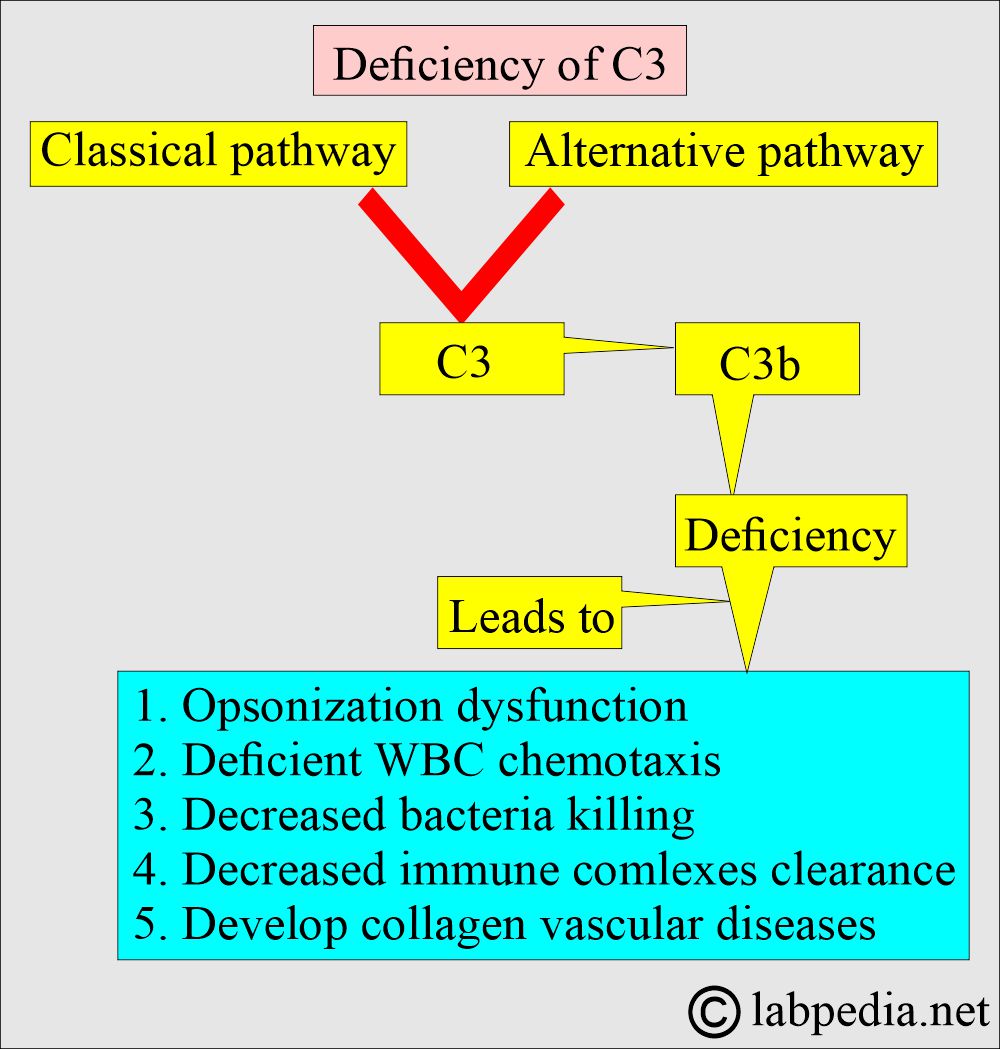
- This occupies the position where Classical and alternative pathways join, and from there, a common path or terminal pathway starts.
- This test is performed to find out the deficiency of Complement C3.
- What does complement C3 indicate?
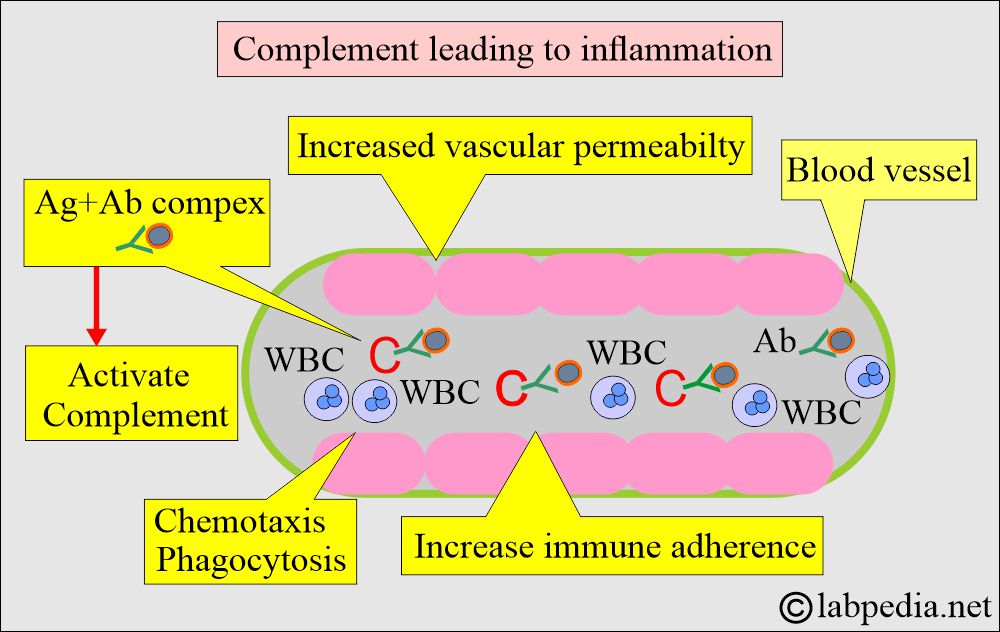
What is the effect of activated complement?
- Increased vascular permeability.
- Attracts White blood cells to the site of antigen and antibody.
- It acts as a chemotactic agent.
- It increases the phagocytic phenomenon.
- It increases the adherence of antibodies to the antigen.
- C3 is made in the liver and in smaller amounts in the spleen and other lymphoid organs.
- C4 is made in the lungs and bones.
What are the types of Complement C3 deficiency?
- Congenital, as seen in hereditary angioedema.
- Acquired, where the complement is consumed by antigen and antibody reaction, e.g., serum sickness, lupus erythematosus, infectious endocarditis, renal transplantation rejection phenomenon, vasculitis, and different types of Glomerulonephritis.
- The complement level can be reverted to normal after treating these diseases.
- Complement C3 deficiency leads to a defective inflammatory response.
What is the normal range of C3?
Source 1
| Sample | Normal value |
|
|
|
|
|
|
- For conversion into SI units x 0.01 = g/L
Another source = Adult value = 76 to 142 mg/dL
Source 2
- 55 to 120 mg/dL
What are the causes of decreased complement activity?
- Hereditary angioedema.
- Bacterial infections (especially Neisseria).
- Cirrhosis.
- Post-streptococcal Glomerulonephritis (present at an extremely low level).
- Hepatitis.
- Lupus nephritis.
- Malnutrition.
- Kidney transplant rejection.
- Systemic lupus erythematosus.
What is the presentation of Congenital C3 deficiency?
- C3 deficiency is associated with recurrent pyogenic infection.
- C3 may be decreased due to congenital deficiency of control proteins, factor H, and factor I.
What is the presentation of the Acquired C3 deficiency?
- This may be seen as a decrease in various types of infections and inflammatory conditions.
- The primary cause is an immune complex disease like SLE, Rheumatoid arthritis, and Subacute bacterial endocarditis.
- Viremia, parasitemia, and bacterial sepsis.
- In membranous glomerulitis.
Under what conditions will you see an increase in C3?
- As an acute-phase protein in Rheumatic fever, Viral Hepatitis, myocardial infarction, cancers, diabetes, and pregnancy.
- in Sarcoidosis and Amyloidosis.
- Thyroiditis.
- Inflammatory bowel disease (Ulcerative colitis).
- Typhoid fever.
- Pneumococcal pneumonia.
What autoimmune disease causes high C3 complement?
- Systemic lupus erythematosus leads to an abnormal C3 complement level.
Questions and answers:
Question 1: In which condition is the C3 level raised?
Question 2: What is the use of C3 estimation?