Activated Partial Thromboplastin Time (APTT), Partial thromboplastin time (PTT), Prothrombin time (PT)
Activated Partial Thromboplastin Time (APTT)
What sample is needed for Activated Partial Thromboplastin (APTT)?
- The blood is carefully collected in an anticoagulant with a fixed ratio.
- Take 0.2 ml anticoagulant (ESR solution may be used) and 1.8 ml whole blood.
- Draw blood from a 3.2% buffered citrated tube with a 9:1 = blood: citrate ratio.
- Citrate binds calcium and prevents coagulation.
- The APTT sample may be taken 30 to 60 minutes before the next dose of Heparin.
What are the precautions for Activated Partial Thromboplastin (APTT)?
- Plasma is stable for one hour at 4 °C and 28 days if frozen.
- Sample handling is very critical. If the blood and anticoagulant ratio is incorrect, then the results are false and raised.
What are the Indications for Activated Partial Thromboplastin (APTT)?
- APTT is used to monitor the heparin therapy.
- This is used for the diagnosis of bleeding disorders.
- APTT may be used to check treatment for patients taking Heparin or other blood-thinning medicines.
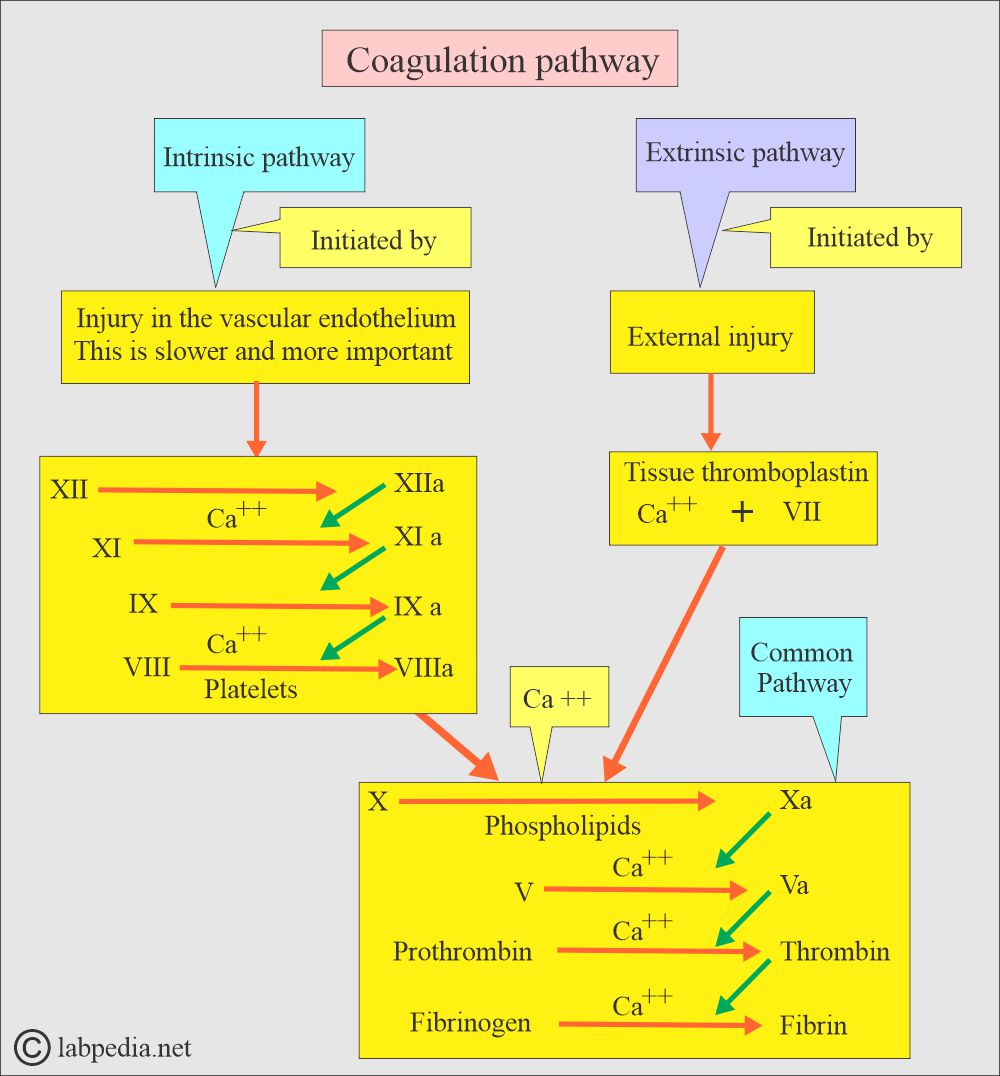
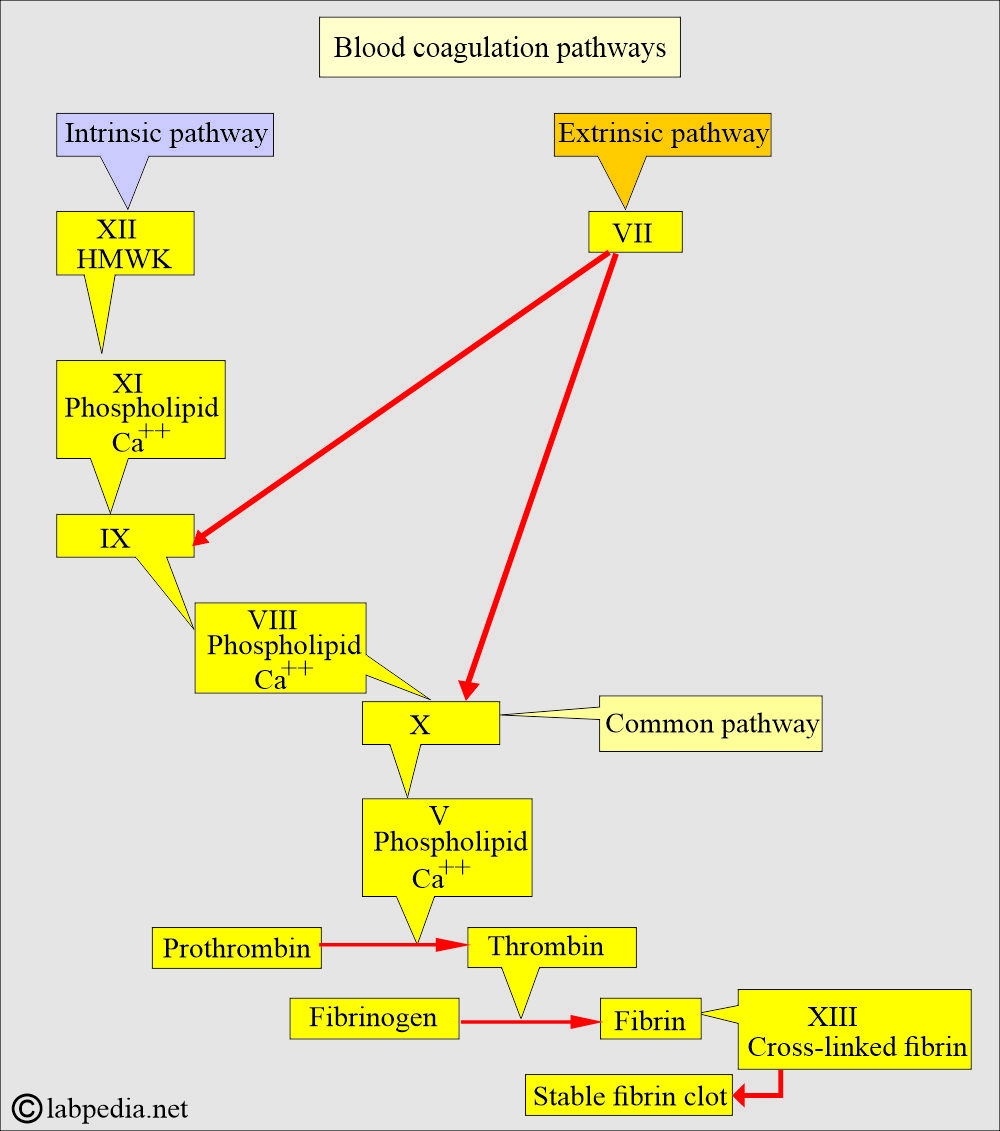
- APTT measures the intrinsic system and common pathways.
- APTT detects the functioning of factors XII, XI, X, IX, VII, V, II, and I (12, 11, 10, 9, 7, 5, 2, 1).
- For the diagnosis of Hemophilia and Christmas disease.
- APTT evaluates all coagulation factors except factors VII and XIII.
- PT is advised to monitor the extrinsic pathway.
- PT is also advised to monitor the warfarin therapy.
- PT also advised detecting factor VII deficiency.
What is the principle of Activated Partial Thromboplastin (APTT)?
- The PTT is a one-stage test.
- PTT evaluates Factor I (Fibrinogen), Factor II (prothrombin), Factor V, VIII, XI, X, XI, and XII (5, 8, 9, 10, 12) http://Blood Coagulation Factors.
- The partial thromboplastin time (PTT) and Activated Partial thromboplastin time (APTT) are for the same function, but APTT is a more sensitive version of PTT.
How will you define PTT and APTT?
The PTT is a one-stage clotting test.
- It screens for coagulation disorders.
- It can detect the deficiency of the intrinsic thromboplastin system.
- It also detects any deficiency of the extrinsic coagulation pathway.
Activated Partial Thromboplastin (APTT):
- APTT is PTT, but with the addition of an activator, the time for the clot formation is decreased.
- APTT is more sensitive than PTT.
What is detected by the Activated Partial Thromboplastin (APTT)?
- Deficiency of the intrinsic pathway.
- Incubating anticoagulants.
- Monitor heparin therapy.
- It is part of the coagulation panel.
What are the theories of coagulation?
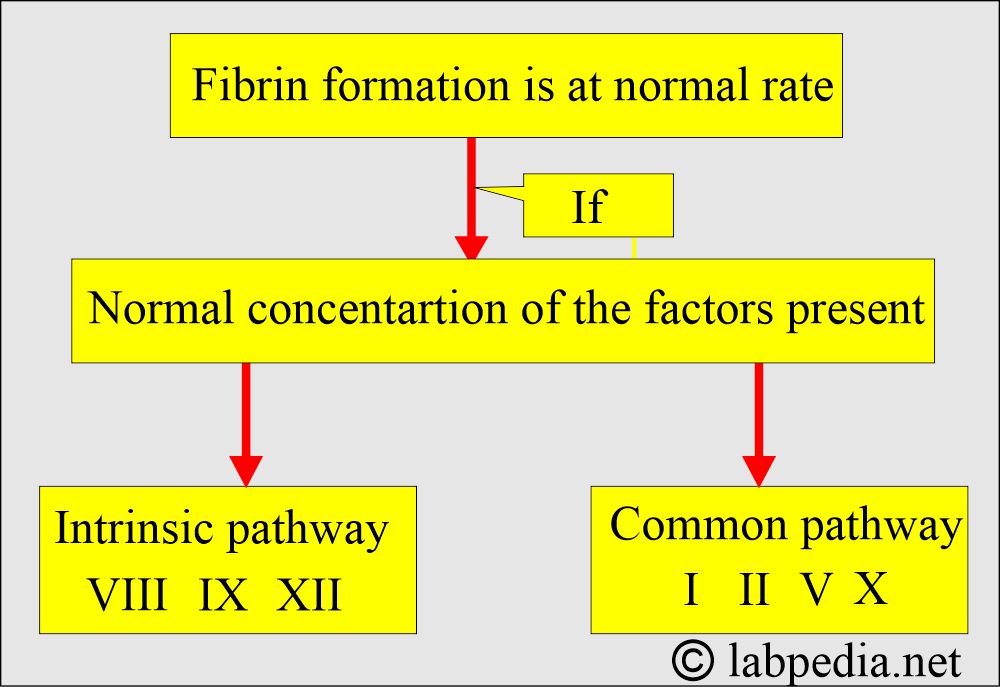
- To understand the basis of the PTT and APTT, we have to have the concept of the process of coagulation.
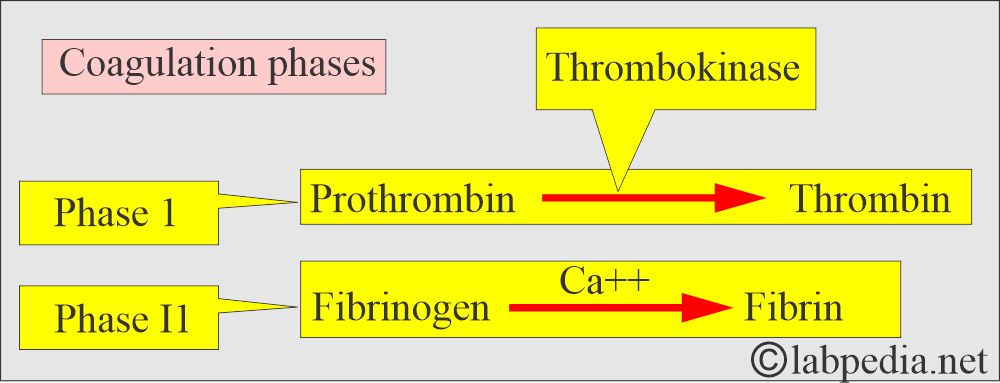
- In 1905 – 1906, P. Morowitz published the theory of blood coagulation. This was unchanged for 40 years. He divided coagulation into two phases.
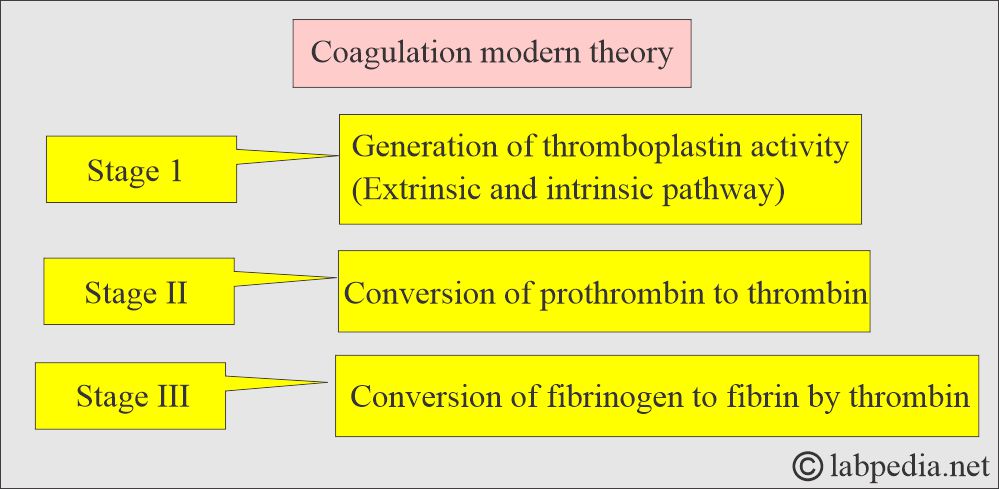
- Modern theory divided this process into three stages.
How is the coagulation cascade run?
What is the presentation of Bleeding disorders in various conditions?
- Platelet disorders give rise to:
- Petechiae.
- There is bleeding from the mucous membranes,
- Coagulation factors deficiency leads to:
- Deep hematomas.
- There is bleeding into the joints.
- There is hematuria.
- Bleeding disorders may be due to:
- Defects in the vascular system.
- Platelets disorders.
- Coagulation factors deficiency.
- Specific inhibitors.
- Fibrinolytic disorders.
Activated partial thromboplastin time (APTT):
How will you define APTT?
- APTT is very sensitive to coagulation factors deficiencies within the intrinsic pathway before the prothrombin to thrombin stage.
- APTT detects more deficiencies in the Intrinsic pathway.
- APTT is used to monitor heparin therapy.
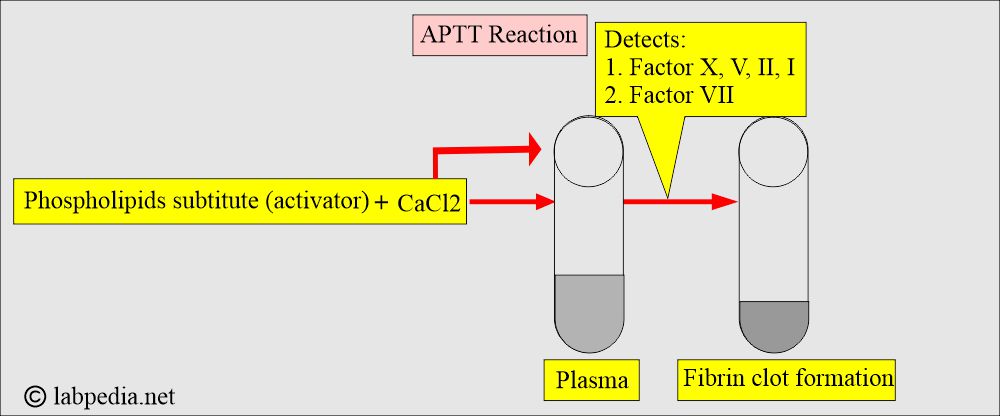
What reagents are used in APTT?
- Phospholipids substitute, activator.
- CaCl2 initiates fibrin clots.
What is the significance of APTT?
- PTT is used to detect coagulation disorder, specifically detecting the deficiency of the intrinsic thromboplastin system and finding the defect in the extrinsic pathway.
- APTT detects the intrinsic pathway and common pathway deficiency (XII, XI, IX, VIII, X, II, and I).
- PT and APTT abnormalities will tell us common pathways (X, V, II, and I).
What are the advantages of APTT?
- APTT reproducibility is adequate where there is <10% variation.
- Its reaction is less (30 to 50 seconds).
- It is easy to perform.
- It can be used in automation.
What are the disadvantages of APTT?
- Heparin above the required level causes APTT to be nonlinear and unreliable.
- Reagents from different companies produce different results, so it is not possible to compare the results.
- APTT is affected by warfarin.
Partial thromboplastin time (PTT):
How will you define PTT?
- PTT was useful in detecting intrinsic factor abnormalities, but it was relatively insensitive to the effect of heparin.
- However, APTT was sensitive to the heparin effect.
- The APTT was sensitive to coagulation factors deficiency within the intrinsic pathway before the prothrombin was converted to thrombin.
What are the indications for PTT?
- Detect the Intrinsic thromboplastin system.
- Detects Common Pathway.
- Factor I (fibrinogen), Factor II (prothrombin), V, VIII, IX, X, XI, and XII.
- Detects extrinsic coagulation.
- It is a one-stage clotting test.
What is the significance of PTT?
- In Hemophilia, PTT is prolonged.
- Coagulation factors are synthesized in the liver, so in liver diseases, they are decreased.
- PTT is prolonged in the abnormality of the deficiency of factors I, II, VII, XII, X, XI, and XII.
Prothrombin time (PT):
How will you define prothrombin time (PT)?
- Prothrombin is a protein produced by the liver.
- Prothrombin production is dependent upon an adequate amount of vitamin K.
- It is one of the important screening tests for coagulation abnormality.
What are the indications for Prothrombin time (PT)?
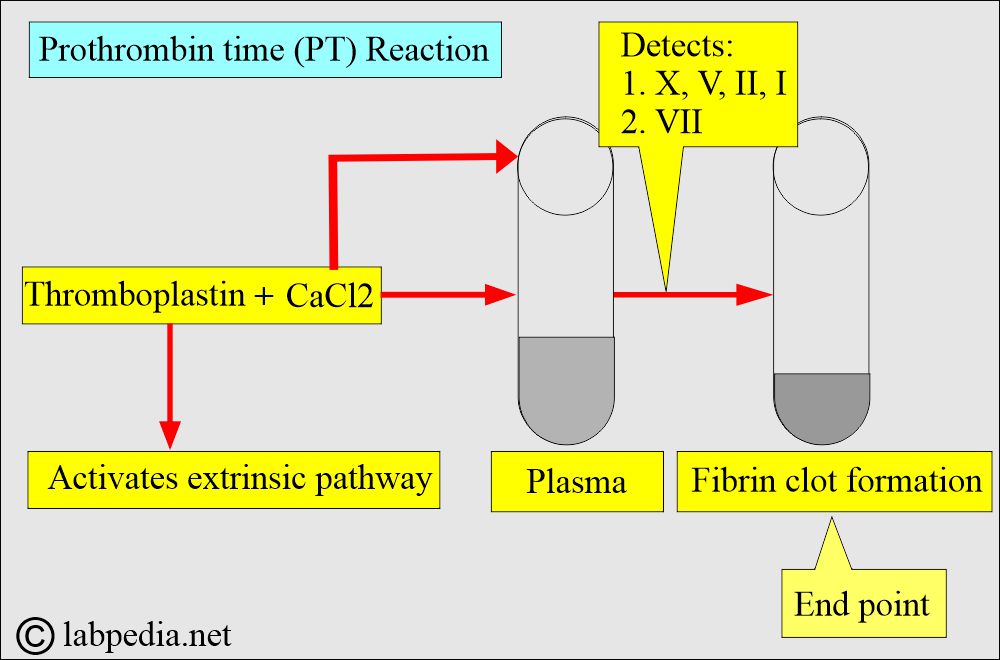
- It measures potential defects in stage II of coagulation, extrinsic pathway.
- To monitor anticoagulant therapy with Coumadin.
- It is advised for coagulation disorder.
- It may be part of liver functions.
What are the contents of prothrombin time (PT) reagents?
- The plasma of the patient.
- Complete tissue thromboplastin (this will activate the extrinsic coagulation system).
- Phospholipids act as platelet substitutes.
- CaCl2.
What is the significance of prothrombin time (PT)?
- The PT test measures factors of extrinsic and common pathways (VII, X, V, II, and I).
- Factor VII is listed as the extrinsic system.
- Common pathways have the factors X, V, II, and I.
- PT test is ideal to detect early vitamin K deficiency.
- PT also monitors oral anticoagulant therapy.
- In case of severe fibrinogen deficiency, it produces an abnormal PT test.
- PT does not detect deficiency of factors XII, XI, IX, VIII, or XIII.
What is the normal value of PTT and APTT
Source 1
- Varies from lab to lab.
- Normal control is always run with the patient sample.
- In general, it is <35 seconds.
- PTT: 60 to 70 seconds.
- APTT: 30 to 40 seconds.
- If APTT is less than 50 seconds, then the therapeutic goal is not achieved, and the Heparin dose may increase.
- When APTT is greater than 100 seconds is risky for the patient, and there are chances of spontaneous bleeding.
- Panic value Usually, it is considered above 70 seconds.
- Heparin’s effect is immediate and short-lived as compared to warfarin.
Source 2
- APTT = 30 to 40 seconds
- PTT = 60 to 70 seconds
- PT = 11.0 to 13.0 seconds
- Possible critical values
- APTT = >70 seconds
- PTT = > 100 seconds
What are the causes of increased APTT value?
- All congenital deficiencies (Intrinsic system coagulation factors).
- Cirrhosis.
- Disseminated intravascular coagulopathy (DIC ).
- Fibrin breakdown products.
- Factor XII deficiency.
- Hemophilia A and B.
- Hypofibrinogenemia.
- Malabsorption.
- Von Willebrand’s disease.
- Vit K deficiency.
- Fibrin breakdown products.
- Leukemia.
- Drugs.
- Heparin therapy.
- Warfarin therapy.
- In the case of streptokinase and urokinase.
- Circulating anticoagulant inhibitors. These may be specific for factor VIII.
- These are seen as anti-factor VIII and anti-factor IX in 5% to 10% of hemophilic patients.
- These are also in multiple plasma transfusions.
- Drug reactions.
- In the case of tuberculosis.
- In autoimmune diseases like SLE and rheumatoid arthritis.
What are the PT and APTT levels in various diseases?
| APTT | PT | Platelets count | Causes of bleeding disorders |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What is the value of these tests for laymen?
- This test is advised for patients treated with Heparin or blood-thinning drugs.
- PTT and INR also have been done in patients with blood-thinning drugs (warfarin).
- For more information, please see PT and PTT.
Questions and answers:
Question 1: What will be the coagulation profile in factor VII deficiency??
Question 2: What will be the coagulation profile in acute DIC?

[…] and APTT are prolonged in factor V […]