Coagulation:- part 4 – Partial Thromboplastin Time (PTT) and APTT
Partial Thromboplastin Time (PTT)
What sample is required for a Partial Thromboplastin Time (PTT) test?
- The blood sample is taken with the anticoagulant.
- The PTT blood sample is 1.8 ml of blood, and the anticoagulant (maybe ESR solution) is 0.2 ml.
- Patient Blood 1.8 ml + 0.2 ml ESR solution.
- Draw blood in the 3.2% buffered citrated tube with a blood: citrate ratio of 9:1 (blood 9 parts + citrate one part).
- Citrate binds to calcium and prevents coagulation.
- If there are other lab tests, then draw the blood at the end for APTT/PTT.
What are the indications for Partial Thromboplastin Time (PTT)?
- Used to monitor the heparin therapy and control its dose.
- It is part of the coagulation panel workup.
- It evaluates:
- Extrinsic Pathway.
- Common Pathway.
- Advised to evaluate abnormal bleeding.
- It is recommended before the surgery.
- It evaluates factors I, II, V, VIII, IX, X, XI, and XII (1, 2, 5, 8, 9, 10, 11, 12).
- APTT evaluates all coagulation factors except factors VII and XIII.
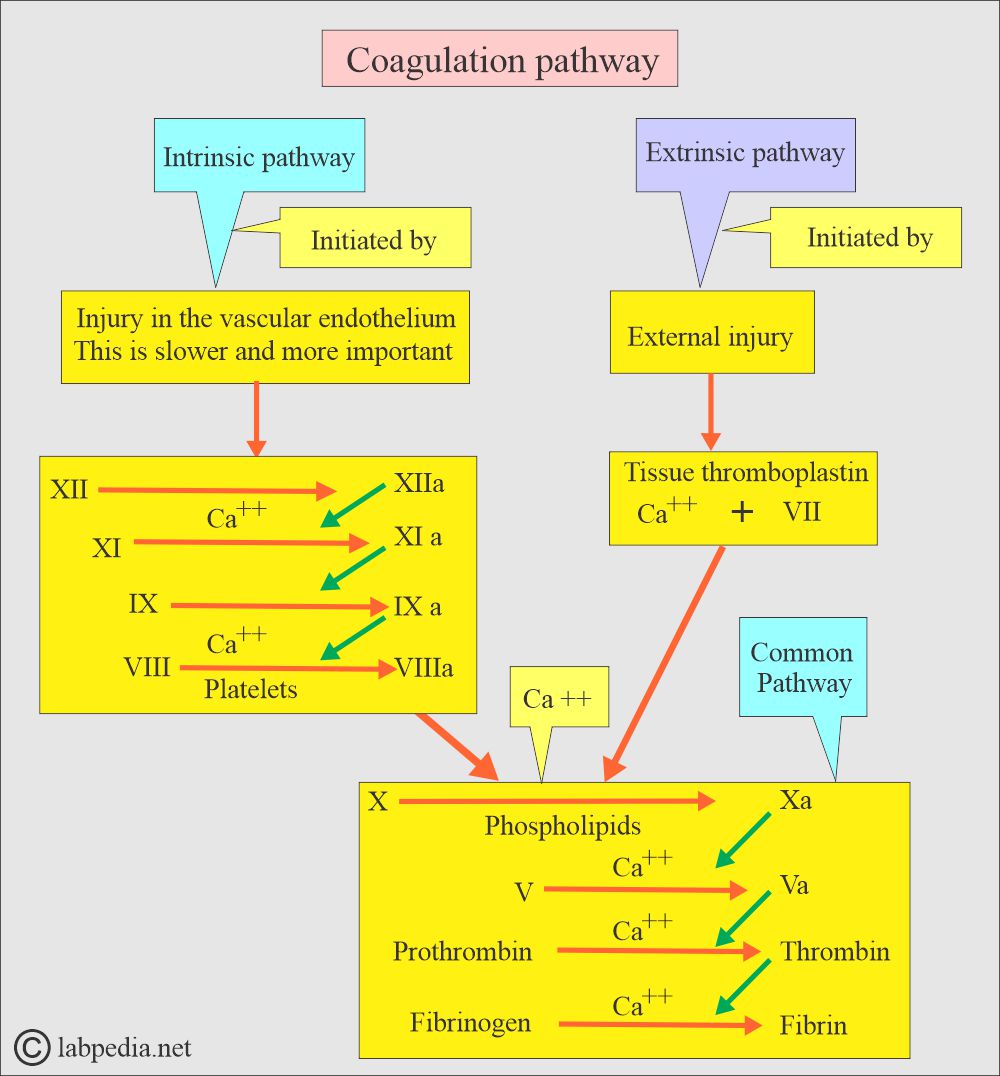
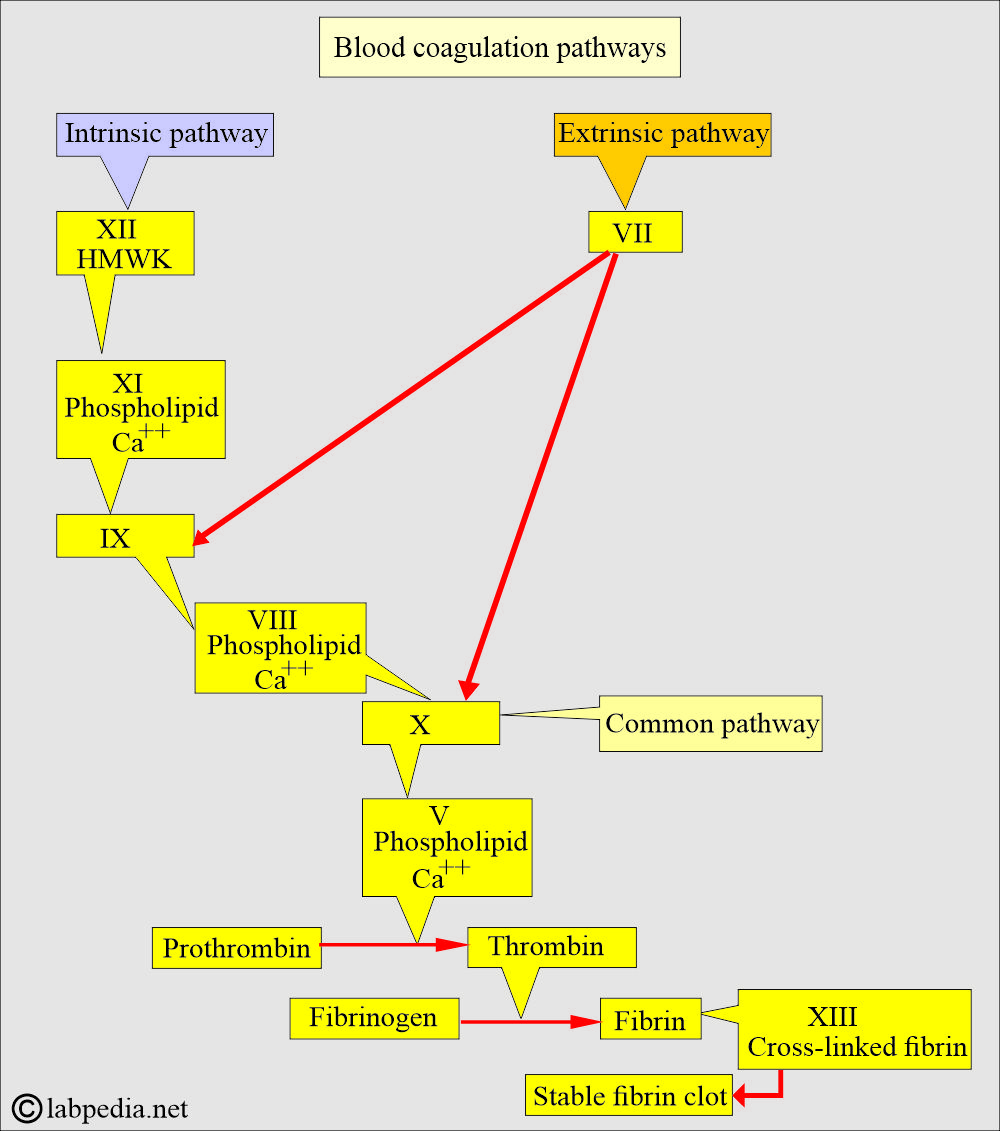
What are the possible pathways of the Coagulation System?
- To understand the coagulation mechanism, follow the diagrams, which give the various coagulation factors and their role.
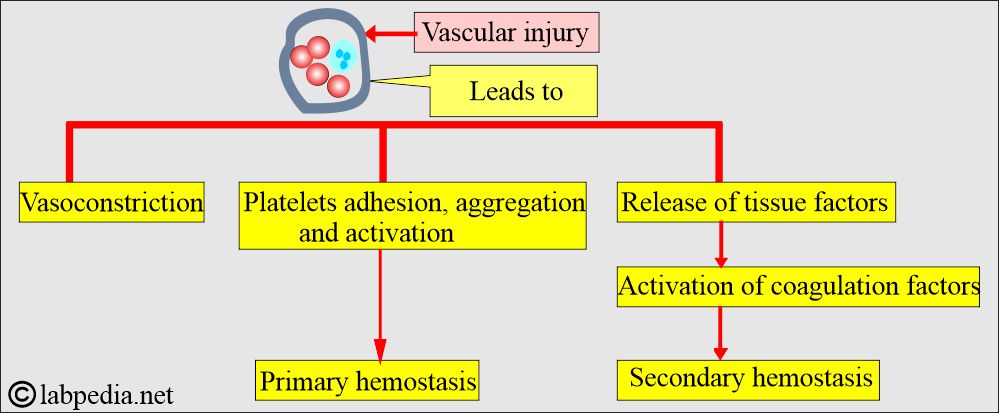
- Hemostasis and the coagulation process represent the hemostatic balance, which lies between the clotting factors and those that encourage clot dissolution.
- The first reaction of the body is the constriction of the blood vessels. In small blood vessels, this constriction may be enough to control the bleeding.
- In large blood vessels, a clot is needed to stop bleeding. This process will be as follows:
- The First stage is the changes in the platelets.
- The next phase is called the intrinsic system.
- Factor XII and other proteins form the complex on the subendothelial collagen in the damaged blood vessels.
- Activated factor XIa is formed, which in turn activates factor IXa.
- Now, complex forms consist of factors VIII, IX, and X.
- Activated factor Xa enters the common pathway.
-
- At the same time, the extrinsic system is activated.
- There is a complex formation between the tissue thromboplastin (Factor III) and factor VII. Activate factor VIIa forms.
- VIIa can directly activate factor X.
- VIIa can also activate factors IX and X.
How will you discuss the pathophysiology of partial thromboplastin time (PTT)?
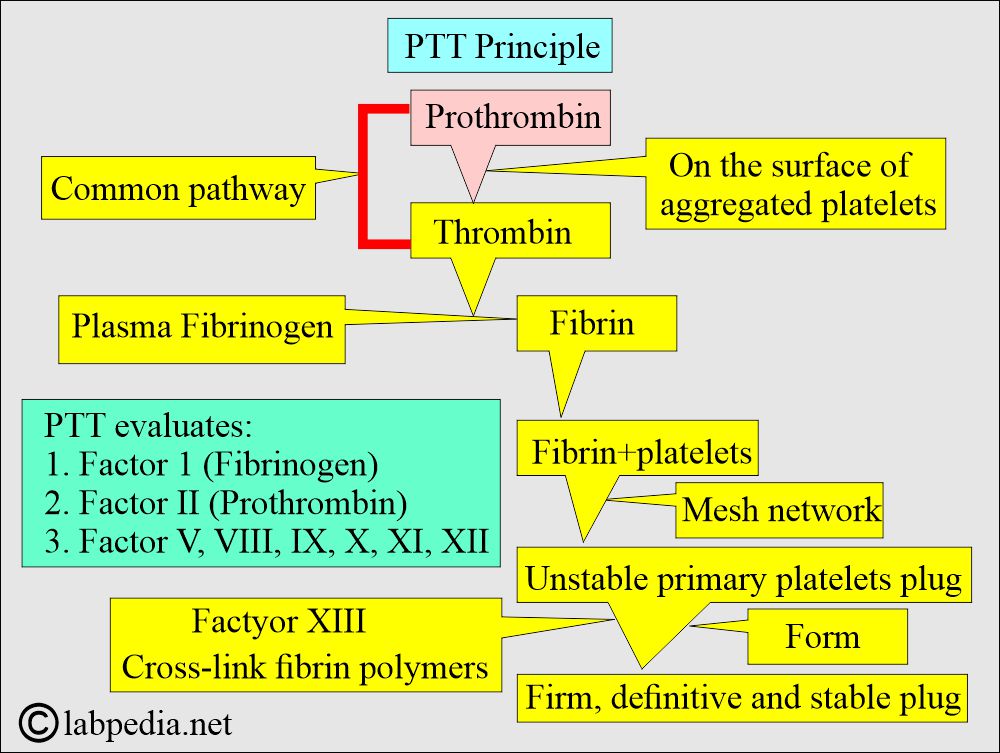
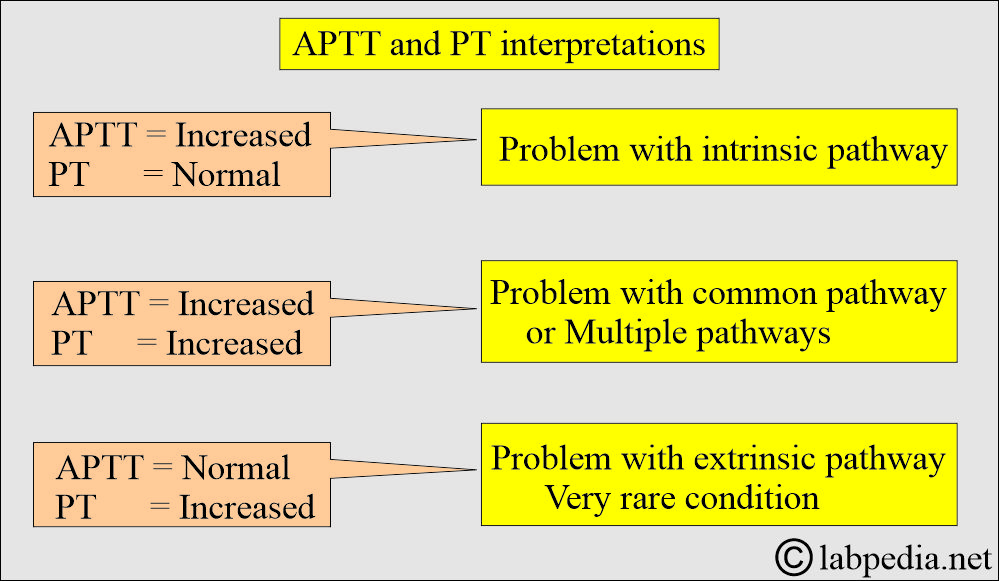
- PTT assesses the intrinsic and common pathways of the clotting system.
- PTT evaluates:
- PTT evaluates factor 1 (fibrinogen), factor II (prothrombin), V, VIII, IX, XI, and factor XII.
- PTT is prolonged in any deficiency of these factors, like in hemophilia A and B or consumptive coagulopathy.
- Coagulation factors are synthesized in the liver, so in liver diseases, PTT will be prolonged.
- Heparin inactivates prothrombin (factor II) and prevents the formation of thromboplastin.
- Heparin will prolong the intrinsic clotting mechanism for around 4 to 6 hours after each dose of heparin.
How will you describe Activated partial thromboplastin time (APTT)?
- When activators are added to the PTT reagent to shorten the clotting time, this process is called activated partial thromboplastin time APTT.
- The blood for APTT will be drawn 30 to 60 minutes before the next dose of heparin.
- If APTT is <50 seconds, then the dose of heparin is increased.
- When APTT is >100 seconds, it indicates an overdose of heparin.
How will you differentiate PTT and APTT?
| Parameters | PTT | APTT |
|
|
|
|
|
|
|
|
|
|
|
Activators are:
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What is the Heparin mechanism of action?
- Heparin inactivates prothrombin (Factor II), thereby preventing the formation of thromboplastin.
- It will prolong the intrinsic clotting mechanism, which may last between 4 and 6 hours after two doses of heparin therapy.
- The dose of heparin can be monitored by APTT.
Partial thromboplastin time (PTT and APTT) is a one-stage test.
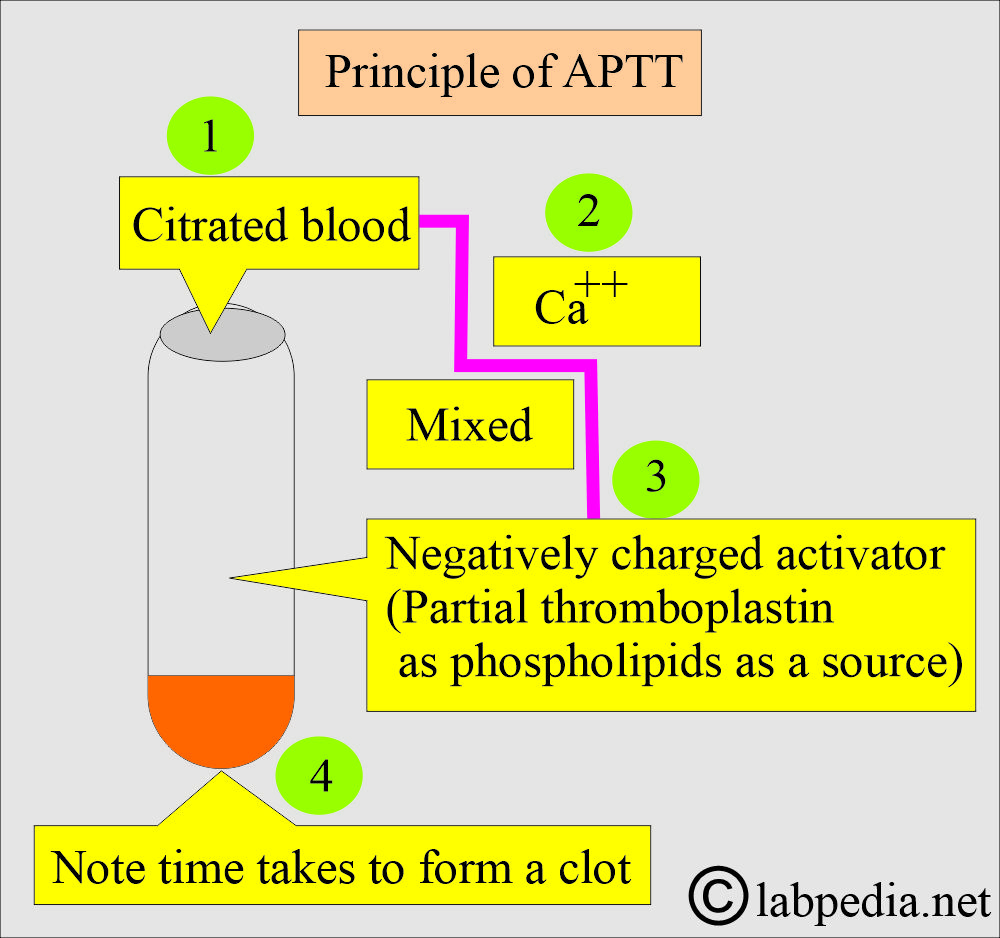
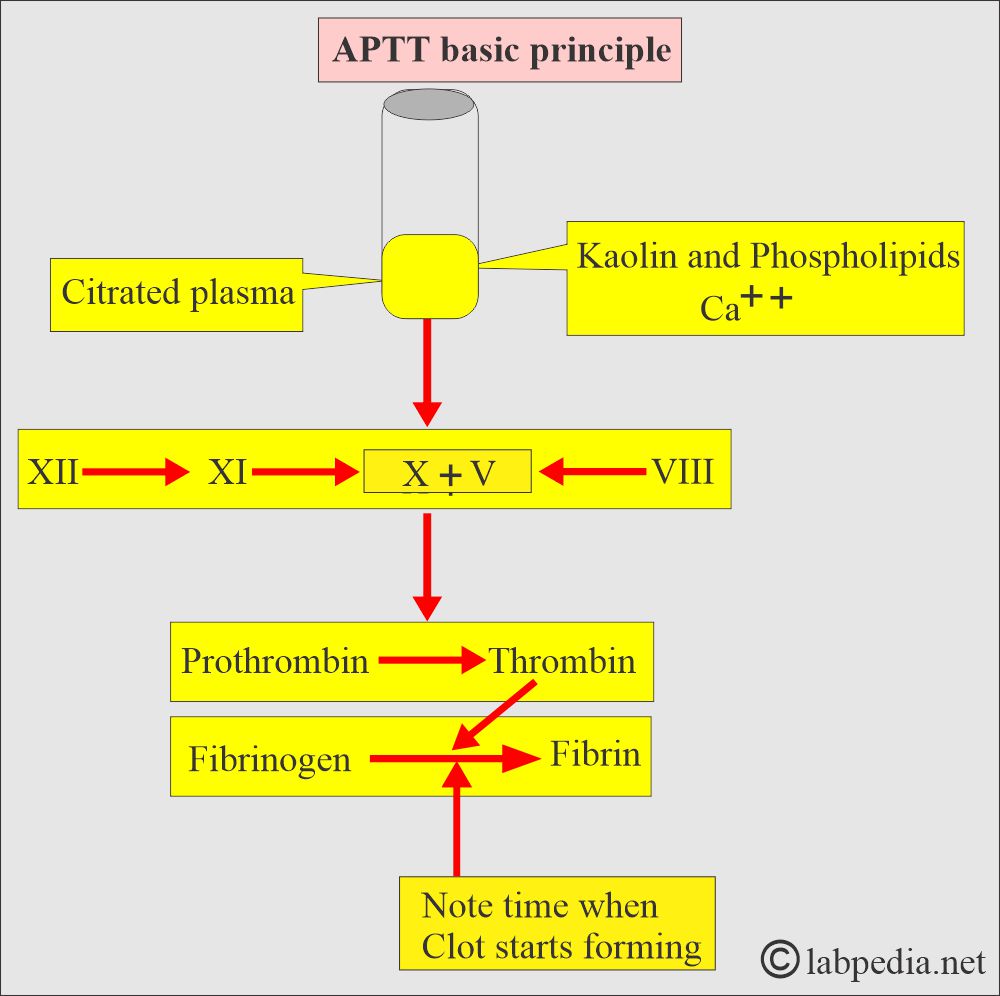
What is the principle of APTT?
- Citrate blood is mixed with a negatively charged activator (phospholipids as thromboplastin).
- Add calcium, which was removed.
- Note the time to clot formation.
- PTT serves the same function as APTT, but APTT is more sensitive.
- PTT detects the intrinsic pathway deficiency of the thromboplastin system and the common pathway.
- PTT also finds a defect in the extrinsic pathway.
- PTT screens intrinsic pathways and tests for the adequacy of factors XII, XI, IX, and VIII.
What is the normal value of Activated Partial Thromboplastin Time (APTT)?
- This is compared with the normal control, which may vary from lab to lab.
- Mostly with control, maybe 25 to 35 seconds.
- Another source = 30 to 45 seconds
- Patient taking anticoagulant therapy level:
- APTT level is 1.5 to 2.5 times the normal value.
What is the difference between PTT, APTT, and PT?
- APTT is actually PTT.
- An incomplete thromboplastin reagent and calcium are added to the patient’s plasma. The time necessary to form the fibrin clot is measured.
- The PTT reagent is only a phospholipid platelet substitute without other thromboplastin components.
- The PTT is useful in detecting intrinsic factors’ abnormality, but is insensitive to heparin therapy.
- The APTT is sensitive to heparin therapy.
- The APTT is very sensitive to coagulation factor deficiency in the intrinsic system before the prothrombin to thrombin stage.
- APTT is also abnormal in prothrombin or fibrinogen deficiencies, but only when the defect is very severe.
- APTT is not sensitive to prothrombin abnormality as PT because the extrinsic thromboplastin used in PT is more powerful than the intrinsic system prothrombin activator complex generated by the APTT.
- PT will detect even a small defect in the prothrombin.
- Platelet abnormalities don’t affect the APTT.
What are the effects of various anticoagulants on the Partial Thromboplastin Test (PTT)?
| Various anticoagulants | Effects of various anticoagulants on PTT |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What are the causes of increased abnormal PTT?
- Liver diseases like Cirrhosis.
- Vitamin K deficiency.
- Disseminated intravascular coagulopathy (DIC).
- Heparin therapy.
- Coumarin therapy.
- Factor XII deficiency.
- Malabsorption.
- Congenital factors are deficiencies as seen in:
- Von Willebrand’s disease.
- Hemophilia A and B.
- Hypofibrinogenemia.
What are the causes of decreased PTT level?
- Early stages of DIC.
- Extensive cancers like ovarian, pancreatic, and colon.
How will you discuss the differential diagnoses of bleeding disorders?
| APTT | PT | Platelets count | Causes of bleeding disorders |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What are the Critical values of PTT and APTT?
- PTT = >100 seconds
- APTT = >70 seconds
Questions and answers:
Question 1: What is the difference between PTT and APTT?
Question 2: When will you find increased APTT, PT, and decreased platelets?

Thank you for your efforts and for this valuable information and the wonderful simple method of explanation.
thank you so much
Thanks.