Coagulation:- part 1 – Blood Coagulation process, Coagulation factors, and factors deficiency
Blood Coagulation process
Sample for Blood Coagulation
- If the plasma is needed, take 5 ml of venous blood and add sodium citrate as the anticoagulant.
- Perform the assay immediately or as soon as possible.
- For factors II, V, VII, and X, place the citrated plasma on ice immediately, and the sample is stable for 2 hours.
- Freeze if it is delayed >2 hours.
Purpose of the test (Indications) for Blood Coagulation
- To measure the coagulation factor concentration in the blood.
- To find the inherited or acquired bleeding disorders.
- If there is a history of bruises or excessive bleeding.
- If there is prolonged PT or PTT.
- Acquired conditions like Vit. K deficiency or liver disease.
- Maybe it is advised to monitor the treatment of a patient with factor deficiency.
Definition of blood coagulation:
- Blood coagulation is the process that consists of a series of biochemical reactions that will transform the blood coagulation factors into an insoluble gel through the conversion of soluble fibrinogen into fibrin.
- The body’s first reaction to bleeding is constricting the blood vessels.
- This will be effective in small blood vessel injuries but not in large blood vessels.
Blood coagulation factors can be divided by physical properties:
- Contact proteins:
- Hageman factor (XII).
- Plasma thromboplastin component (XI).
- Prekallikeri (PK).
- High molecular weight kininogen (HMWK).
- Prothrombin protein:
- Prothrombin (II).
- Stable factor (VII).
- Christmas factor (IX).
- Stuart-Power factor (X).
- Fibrinogen group:
- Fibrinogen (I).
- Labile factor (V).
- Antihemophilic factor (VIII).
- Fibrin stabilizing factor (XIII).
Blood coagulation process:
- The blood coagulation process involves:
- Series of biochemical reactions.
- It transforms circulating substances into an insoluble gel.
- This gel is by the conversion of fibrinogen to fibrin.
- This whole process needs blood coagulation factors, phospholipids, and calcium.
- The blood coagulation process consists of:
- Extrinsic pathway.
- Intrinsic pathway.
- In blood vessel injuries, the clotting factors are activated to plug the injured site.
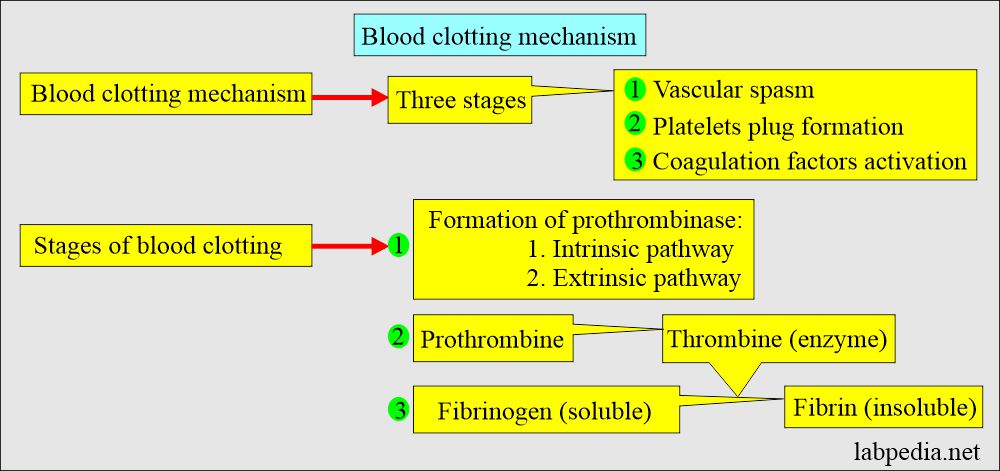
The blood coagulation process is divided into three phases:
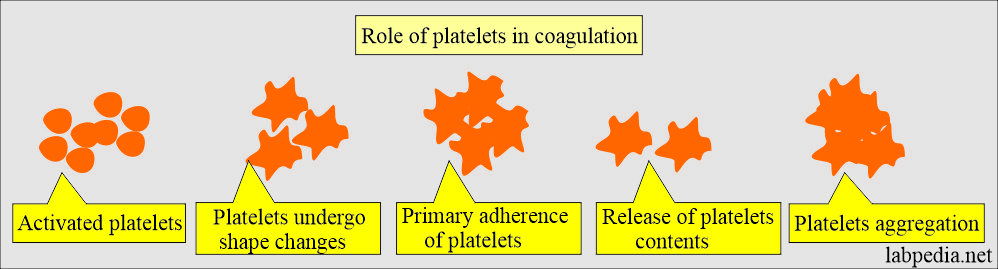
The first stage, the primary phase:
- It is initiated by platelet aggregation.
- Platelets adhere to collagen and have changes in shape.
- Platelets degranulate and release:
- Ionized Ca++.
- Magnesium.
- Serotonin.
- Epinephrine.
- Phosphate.
- ADP and ATP.
- Alpha granules release fibrinogen, platelet-derived growth factor, plasminogen activator inhibitor, albumin, β-thromboglobulin, fibrinonectin, and factor V (absorbed from plasma).
- The release of these chemicals leads to secondary aggregation, which is irreversible.
- Ultimately, platelets change shapes and adhere to each other.
The second stage, the secondary phase:
- It is the activation of clotting factors.
The third stage, in Phase Three:
- The factor X is activated by proteases (VIIa, IXa with XIIIa).
- Va can activate IX and X directly.
- The above reaction is responsible for thrombus formation.
- The adherent and aggregated platelets release factor V and expose factor 3 to accelerate the coagulation process.
- It will stabilize the platelets plug with a fibrin clot.
The blood coagulation pathways are:
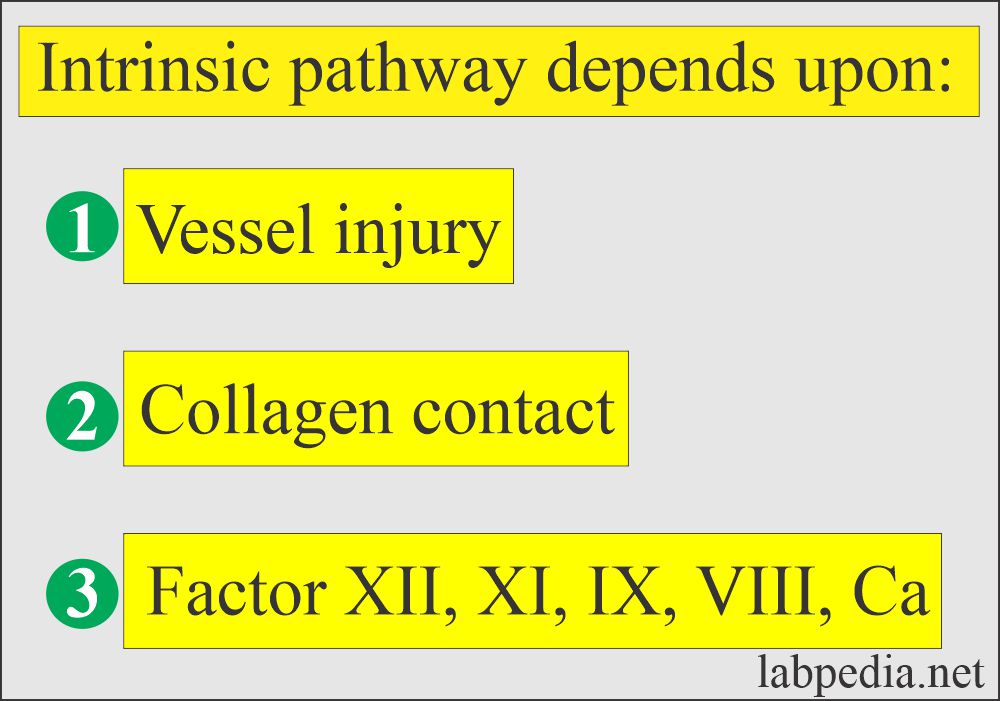
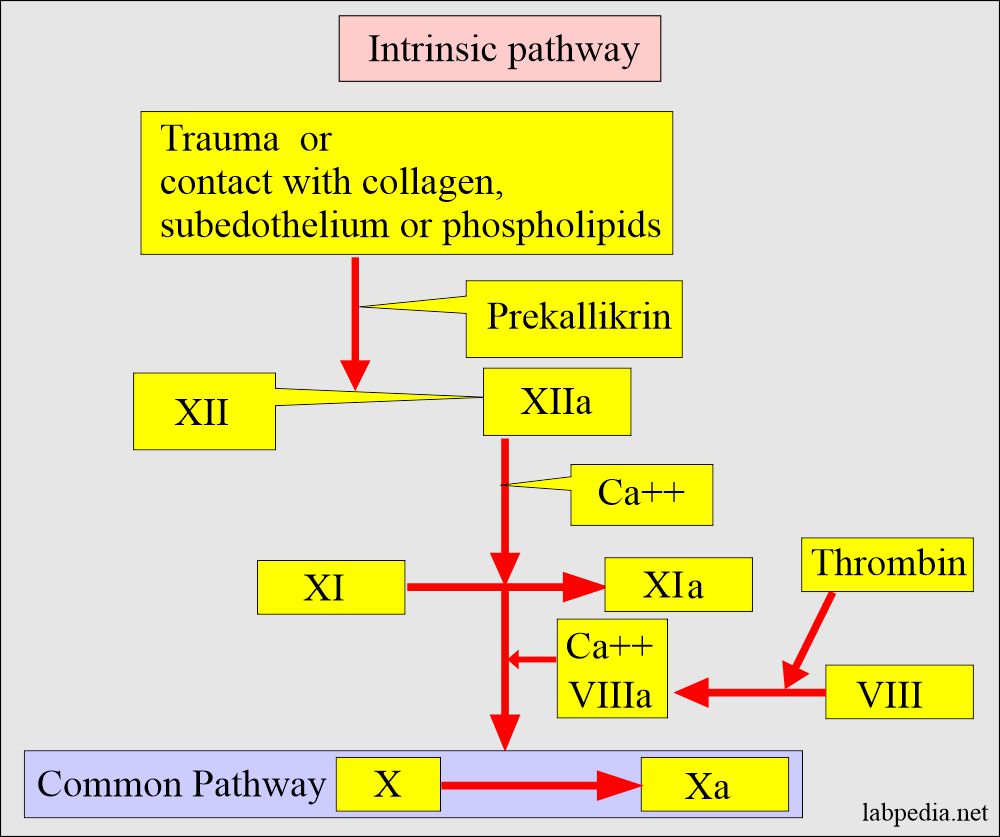
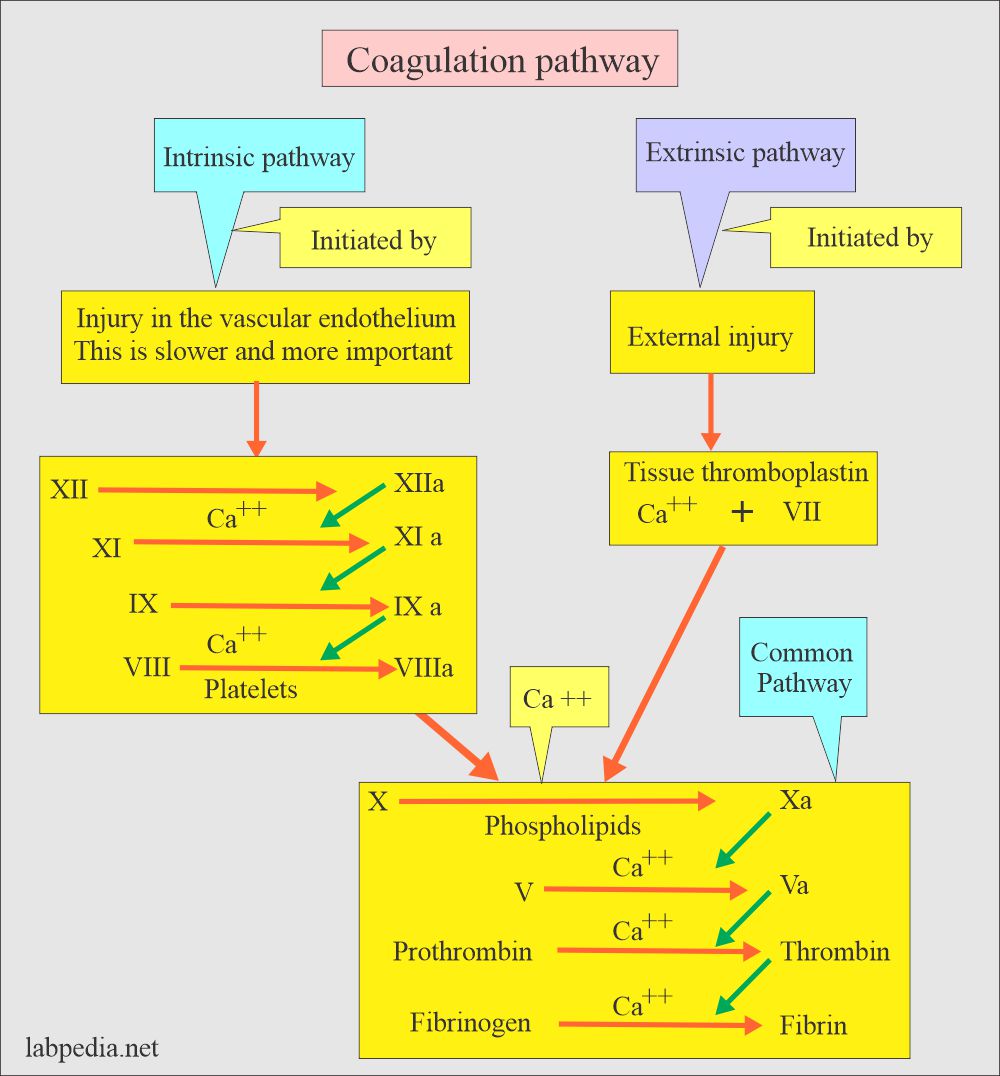
The intrinsic pathway:
- It is initiated by foreign substances like collagen, subendothelium, or phospholipids, which will activate factor XII, involving contact factors and factor XI.
- Where factor XII and other proteins form a complex on the injured endothelium.
- XII
 XIIa
XIIa  XI to XIa and form a complex of VIII + XI + X.
XI to XIa and form a complex of VIII + XI + X. - Activated Xa is formed.
- Then, the common pathway starts.
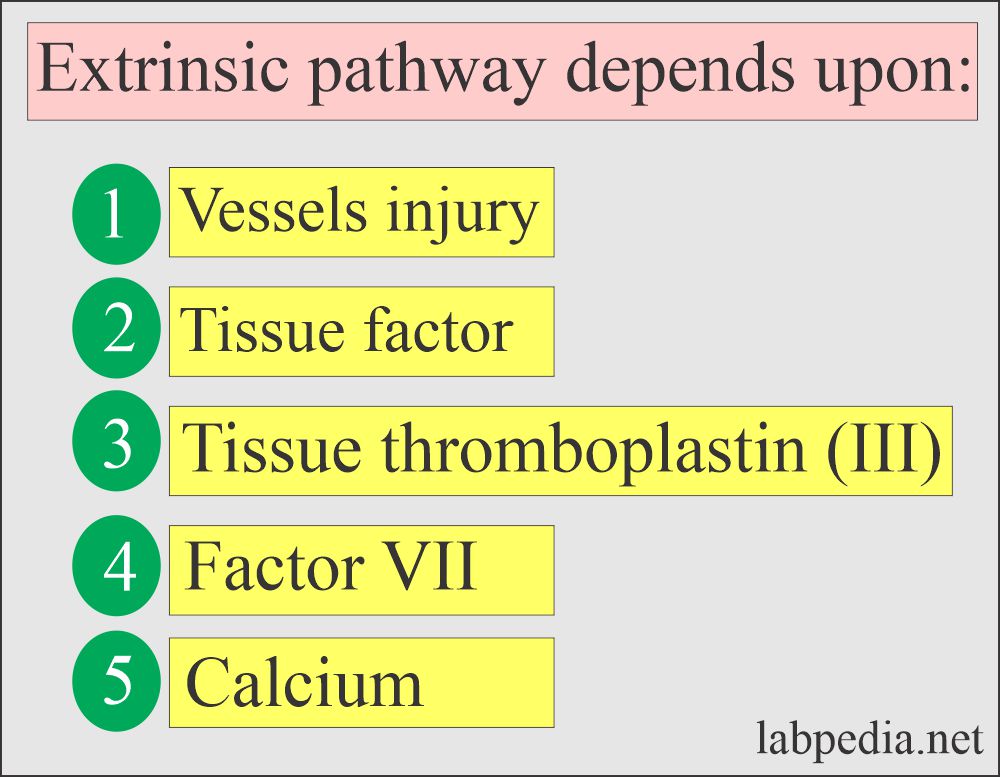
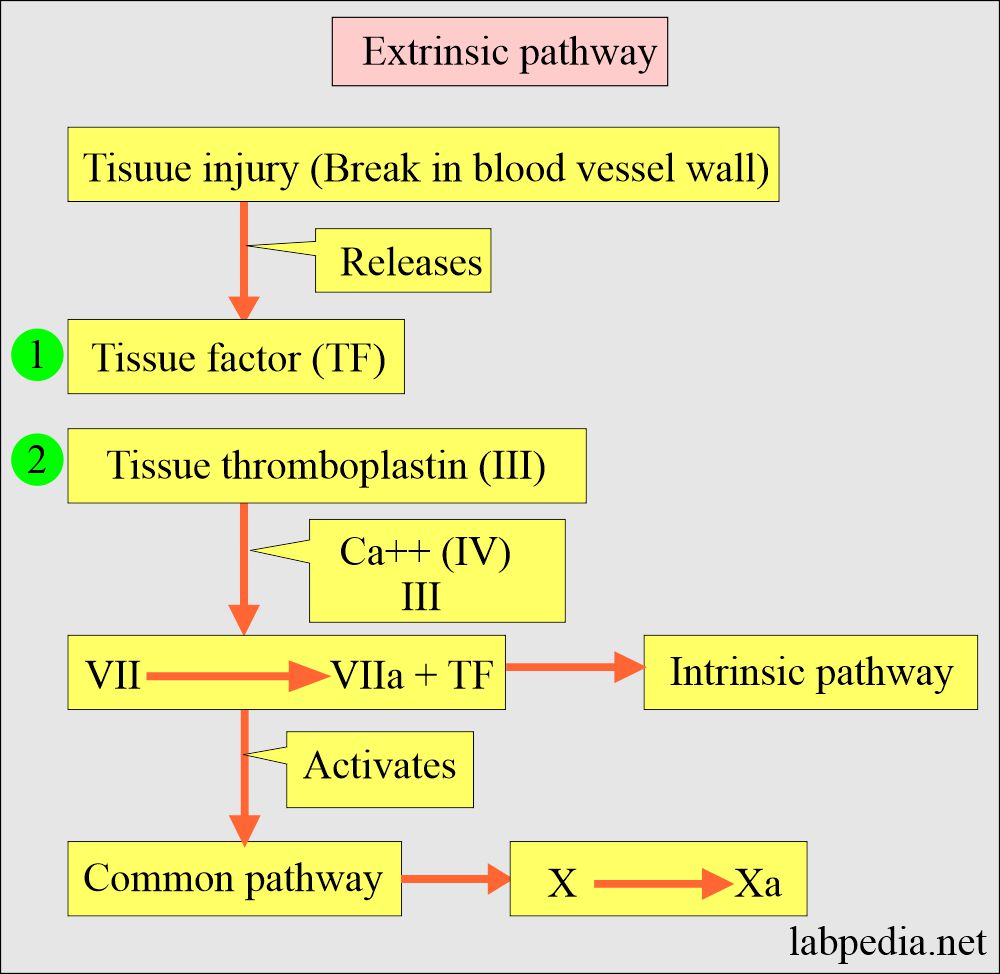
The extrinsic pathway:
- It is a complex formation between the Tissue factor (factor III or thromboplastin) and factor VII.
- Activated factor VIIa forms, which stimulates factor X.
- Alternately, factor VIIa activates factors IX and X.
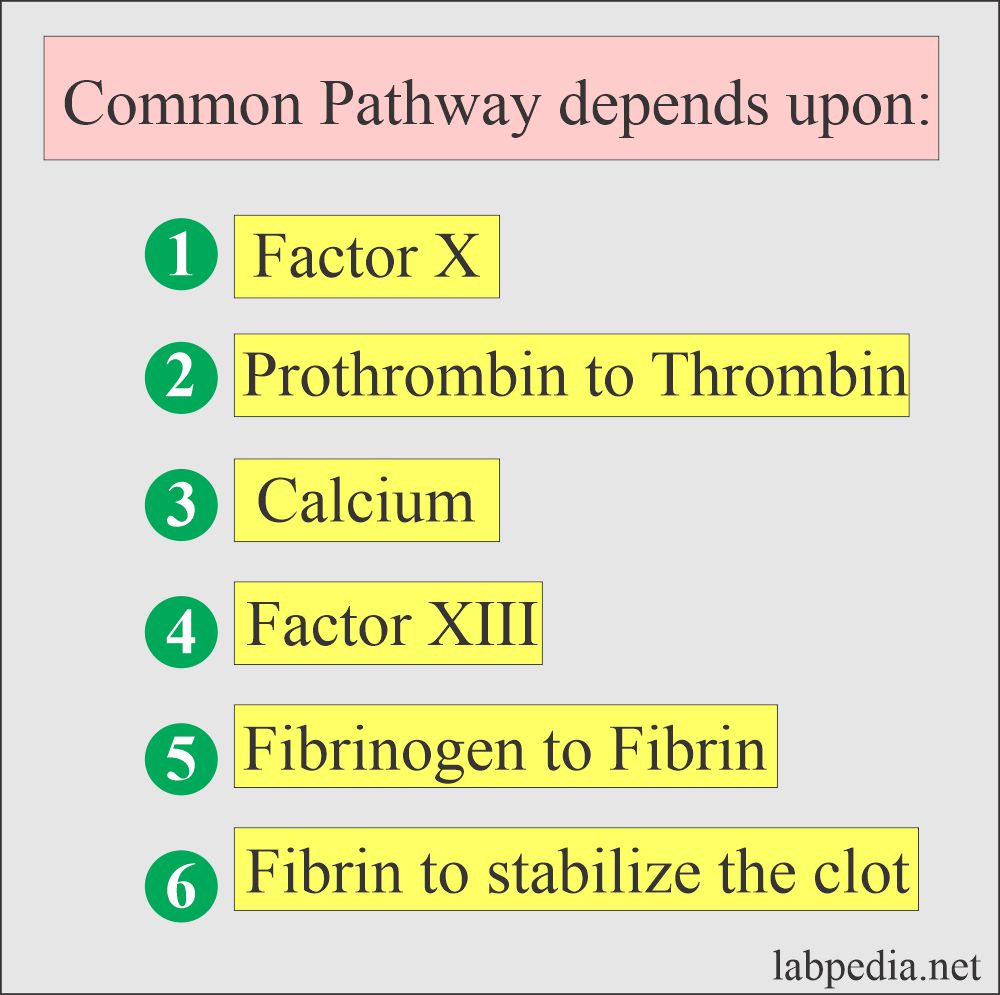
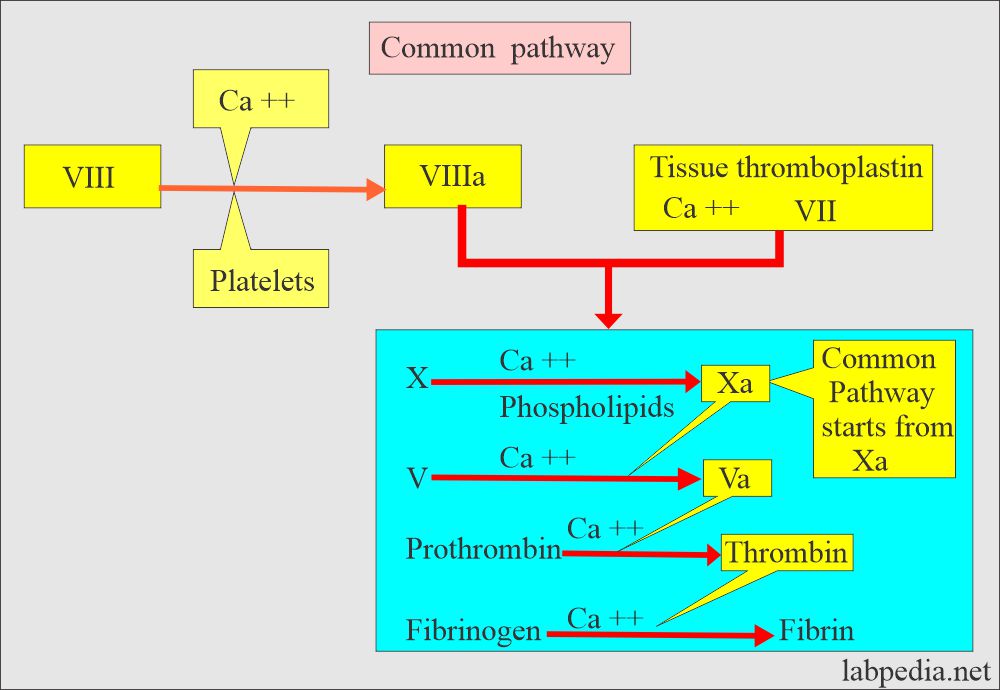
Common pathway:
- The common pathway starts with the activation of factor X by extrinsic or intrinsic pathways or both.
- (Xa) converts Prothrombin to Thrombin (active form) in the presence of factor V, calcium, and phospholipids on the surface of platelets.
- Thrombin converts Fibrinogen to Fibrin polymerized into a stable clot.
- Thrombin also activates factor VIII to stimulate platelet aggregation and fibrin polymerization.
- Prothrombin is a Vit K-dependent factor.
- Plasmin degenerates the fibrin polymer into fragments that are taken up by the phagocytic cells.
- Fibrinogen is considered an acute-phase protein and is increased in many diseases.
Normal values of clotting factors:
| Factors | Normal value Source 1 | Normal value Source 2 | Normal value Source 3 |
|
|
200 to 400 mg/dL | |
| Quantitation minimum hemostatic level mg/dL | Plasma concentration mg/dL | ||
|
|
|
10 to 15 |
| Factor III (Tissue Thromboplastin or tissue factor) | |||
|
|
||
|
|
|
0.5 to 1.0 |
|
|
||
|
|
|
0.2 |
|
|
|
1.0 to 2.0 |
|
|
|
0.3 to 0.4 |
|
|
|
0.6 to 0.8 |
|
|
|
0.4 |
|
|
2.9 | |
|
2.5 | ||
|
1.0 | ||
|
|
||
|
|
- Reference values are different from various sources.
The deficiency of blood coagulation factors may be due to the following:
- Inherited genetic defects.
- Acquired.
- Drugs therapy.
Causes of acquired factor deficiency are:
- Snake venom.
- Liver diseases.
- Uremia.
- Vit. K deficiency.
- Anticoagulant ingestion of warfarin.
- Massive blood transfusion.
- Some of the cancers.
- Disseminated intravascular coagulopathy.
- There is a balance between the factors leading to clotting and the factors causing dissolution.
Various blood coagulation factors:
- Factor XII deficiency was observed as an increased risk of Myocardial infarction and venous thrombosis.
- Fibrinogen is also considered a coronary risk factor that leads to stroke.
- Determine the exact factor deficiency for the replacement therapy.
Fibrinogen:
Fibrinogen level increase is seen in:
- Acute inflammatory reactions.
- Trauma.
- Coronary heart disease.
- Cigarette smoking.
Fibrinogen decreased level is seen in:
- Liver diseases like hepatitis and cirrhosis.
- DIC ( disseminated intravascular coagulopathy ).
- Fibrinolysis.
Prothrombin decreased level is seen in the following:
- Vit. K deficiency.
- Liver disease.
- Oral anticoagulants.
- Circulating inhibitors or lupus-like anticoagulants.
- Decreased synthesis.
Factor V deficiency:
- Liver diseases.
- Factor V inhibitor.
- Myeloproliferative disorders.
- DIC and fibrinolysis.
- Mild decrease in the newborn.
Factor VII deficiency:
- Liver diseases.
- Kwashiorkor.
- Normal newborn.
- Treatment with coumarin-like drugs.
Factor VIII increased in:
- Late normal pregnancy.
- Thromboembolic conditions.
- Liver diseases.
- Postoperative patients.
- Normal newborn.
- Rebound phenomenon after sudden stoppage of coumarin-like drugs.
Factor VIII deficiency:
- due to the presence of factor VIII inhibitors.
- DIC.
- Von Willebrand disease.
- Myeloproliferative disorders.
Factor IX deficiency:
- Liver diseases and cirrhosis.
- Nephrotic syndrome.
- Anticoagulant antibody formation.
- Normal newborn.
- Drugs like Dicoumarol.
- DIC.
- Vit K Deficiency.
Factor X deficiency:
- Vit K deficiency.
- Liver Diseases.
- Oral anticoagulants.
- DIC.
- Amyloidosis.
- Normal newborn.
Factor XI deficiency:
- Liver diseases.
- Intestinal malabsorption leads to Vit K deficiency.
- DIC.
- Newborn.
Factor XII deficiency:
- Nephrotic syndrome.
- Liver diseases.
- Chronic myelocytic leukemia.
- Normal newborn.
Factor XIII deficiency:
- Postoperative patients.
- Liver diseases.
- In persistent increased fibrinogen level.
- Acute myeloid leukemia.
- DIC.
- Circulating anticoagulants.
Diseases leading to coagulation factor deficiency:
| Disease | Factors deficiency |
| Disseminated intravascular coagulopathy | I, V, VIII (1, 5, 8) |
| Liver diseases | I, II, V, VII, IX, X, XI (1, 2, 5, 7, 9, 10, 11) |
| Autoimmune diseases | VIII (8) |
| Congenital deficiency | I, II, V, VII, VIII, IX, X, XI, XII (1, 2, 5, 7, 8, 9, 10, 11, 12) |
| Vit K deficiency | II, VII, IX, X, XI (2, 7, 9, 11) |
| Heparin therapy | II (2) |
| Warfarin therapy | II, VII, IX, X, XI (2, 7, 9, 10, 11) |
| Fibrinolysis | I, V, VIII (1, 5, 8) |
Questions and answers:
Question 1: What oral contraceptives cause factor deficiency?
Question 2: What will be the fibrinogen level in DIC?