Cholinesterase, Functions and Interpretations
Cholinesterase
What sample is needed for Cholinesterase?
- It is done on the serum of patients.
- Enzyme activity in the serum is stable for several weeks.
- Another reference says
- stable for 6 hours at room temperature.
- One week at 4 °C.
- 6 months at -70 °C
- The serum is stable at room temperature and also in refrigeration.
What are the precautions for Cholinesterase?
- Avoid hemolysis.
- Avoid repeated freezing and thawing.
- Pregnancy decreases the test value.
- Drugs that may cause a decrease in the test values are atropine, caffeine, codeine, morphine, oral contraceptives, theophylline, quinidine, estrogen, and vitamin K.
What are the indications for Cholinesterase?
- Advised that when you are exposed to chemicals called organophosphates, which are used in pesticides.
- This test can help determine your risk of poisoning.
- This test is done to rule out poisoning (Organophosphorus).
- For insecticide poisoning.
- e.g., parathion, sarin, and tetraethyl pyrophosphate.
- To diagnose liver disease.
- Before you receive anesthesia with succinylcholine, which may be given before certain procedures or treatments, including electroconvulsive therapy (ECT).
- Particularly in the case of pseudocholinesterase deficiency before anesthesia.
- Monitoring patients with liver disease, particularly those undergoing liver transplantation.
- Identifying patients who are homozygous or heterozygous for an atypical gene with low pseudocholinesterase levels.
How will you define cholinesterase?
- Cholinesterase includes both enzymes, such as acetylcholinesterase and butylcholinesterase.
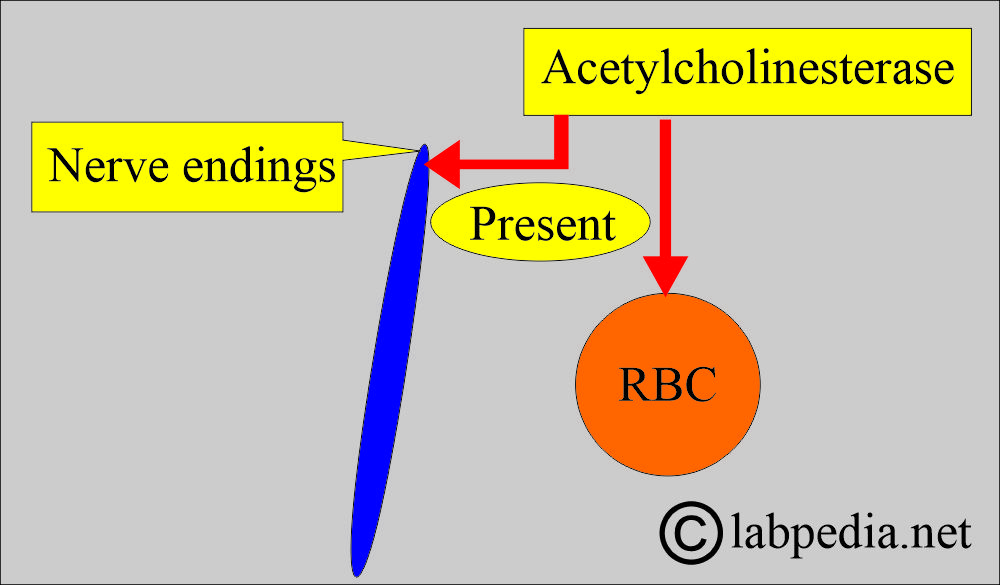
- Acetylcholinesterase is a specific enzyme that helps in neurotransmission, present at nerve endings and RBCs.
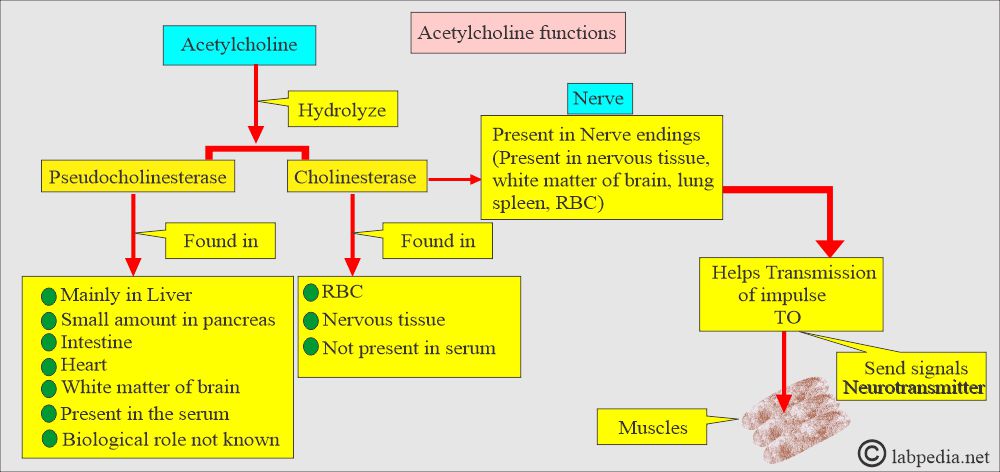
- Cholinesterase hydrolyzes acetylcholine and other choline esters, thereby regulating nerve impulse transmission at nerve synapses and neuromuscular junctions.
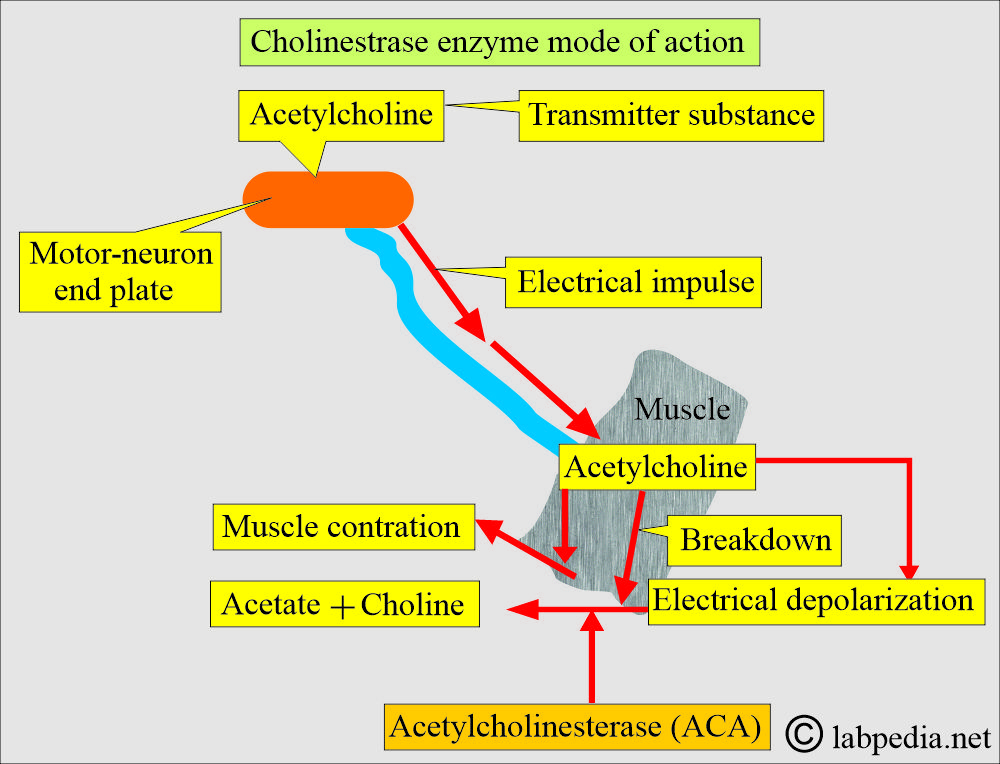
- Acetylcholine is the transmitter substance that is released at the motor neuron end-plate by an electrical impulse traveling down the nerve toward a muscle.
- The function of the neurotransmitter is to propagate an electrical impulse from one neuron to another neuron.
- Acetylcholinesterase exists in RBCs and at nerve endings.
- Two enzymes can hydrolyze acetylcholine.
How will you discuss the Pathophysiology of Cholinesterase?
- Acetylcholine diffuses from the nerve endings to the muscles, causing electrical depolarization of the muscle cells and subsequent muscle contraction.
- Acetylcholine is rapidly broken down to acetate and choline by the enzyme acetylcholinesterase at the post-synaptic site to finish the process.
- Failure to inactivate acetylcholine results in muscular paralysis.
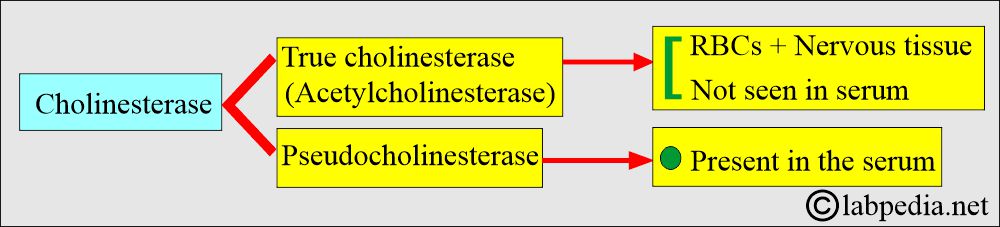
- Cholinesterase is primarily not found in the serum, while pseudocholinesterase is found in the serum.
- Serum cholinesterase is a test that looks at blood levels of enzymes like Acetylcholinesterase and pseudocholinesterase.
- Cholinesterase is an enzyme of the hydrolase group.
- It can catalyze the breakdown of an acyl group from various choline esters and acetylcholine.
- Cholinesterase is of two types:
- Acetylcholinesterase:
- This is also known as true cholinesterase.
- Pseudocholinesterase in the serum is derived from the liver.
- It is the first noticeable neurotransmitter and is formed in presynaptic cholinergic neurons from acetyl-CoA derived from lipid metabolism.
- Pseudocholinesterase.
- Acetylcholinesterase:
What are the enzyme inhibitors?
- The alkaloids prostigmine and physostigmine inhibit both acetylcholinesterase and butyrylcholinesterase.
- Certain organic phosphorus compounds, such as diisopropyl fluorophosphate, irreversibly inhibit both enzymes.
- Many compounds, such as morphine, tertiary amines, quinine, phenothiazines, pyrophosphate, citrate, bile salts, borate, and fluoride, also inhibit both enzymes.
What is the Cholinesterase enzyme distribution and functions?
- The cholinesterase enzyme breaks down acetylcholine.
- Acetylcholinesterase is found in nerve tissue, red blood cells, and the lungs and spleen.
- It is present in the grey matter of the brain.
- Pseudocholinesterase is found primarily in the liver.
- It is also present in the pancreas, heart, white matter of the brain, and serum.
- These enzymes help the nervous system to work correctly.
- Acetylcholinesterase and pseudocholinesterase are needed to send signals through nerves.
- Acetylcholinesterase in RBCs is known as RBC cholinesterase.
- Pseudocholinesterase, known as butyrylcholinesterase or plasma cholinesterase, helps break down a chemical that nerves need to send signals.
- The difference between the two types of cholinesterase depends on their respective preferences for substrates.
- Acetylcholinesterase hydrolyzes acetylcholine more quickly.
- Pseudocholinesterase hydrolyzes butyrylcholine more quickly.
- The half-life of pseudocholinesterase is approximately 8 to 16 hours.
- Pseudocholinesterase levels may be reduced in patients with advanced liver disease.
- The decrease must be greater than 75% before significant prolongation of neuromuscular blockade occurs with succinylcholine.
- Elevation of plasma pseudocholinesterase was observed in 90.5% of cases of acute myocardial infarction.
- Acetylcholinesterase can confirm several common types of birth defects, including abdominal wall and neural tube defects.
What are the signs and symptoms of a deficiency of Cholinesterase?
- A 40% drop in serum enzyme activity occurs before the first symptoms are noted.
- A drop of 80% is needed before the neuromuscular signs are noted.
- Near 0% enzyme activity requires emergency treatment of the patient with enzymes, such as pyridine-2-aldoxime.
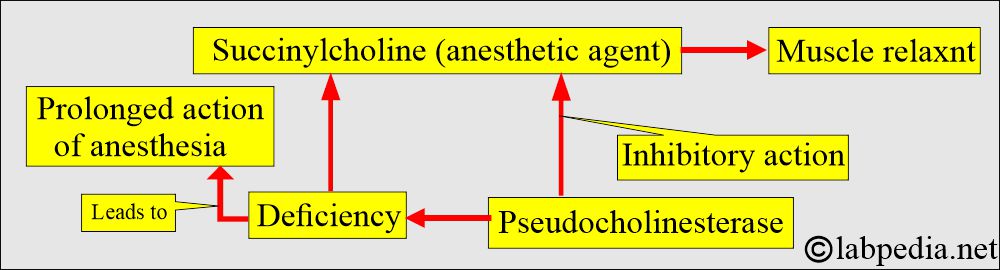
- Pseudocholinesterase deficiency is present in a patient, and if these patients are given anesthesia drugs, they will not break down and leading to prolonged action.
- As a result, the muscles are relaxed, and the patient has difficulty breathing and moving.
What is the normal Cholinesterase?
Source 1
- Serum cholinesterase = 8 to 18 units/mL (8 to 18 units/L).
- RBC cholinesterase = 5 to 10 units/mL (30 to 40 units/g of the hemoglobin).
- Typically, normal pseudocholinesterase values range between 8 and 18 units/mL.
- The values are low at birth and in the first 6 months of life.
- Reference values have not been established for patients who are <18 years of age.
Source 2
- 4.9 to 11.9 U/mL
- Values are low at birth and during the first 6 months of life, increasing to 30% to 50% above adult values by 5 years, then gradually decreasing to adult values by puberty.
- (Values vary according to the type of methodology used.)
What are the causes of an increased serum level of Cholinesterase?
- Nephrosis.
- Diabetes mellitus.
- Hyperlipidemia.
What are the causes of a decreased serum level of Cholinesterase?
- Poisoning with organophosphate insecticide.
- Liver diseases like hepatitis.
- Cirrhosis with ascites or jaundice.
- Metastatic carcinoma.
- Obstructive jaundice.
- Congestive heart failure.
- Before you receive anesthesia with succinylcholine, which may be given before certain procedures or treatments, including electroconvulsive therapy (ECT).
- In conditions with low serum albumins, such as malnutrition, anemia, infections, Dermatomyositis, Acute MI, and liver diseases.
What are the causes of a smaller decrease in cholinesterase?
- Pregnancy.
- Use of birth control pills.
What are the causes of increased RBC-Cholinesterase level?
- Reticulocytosis.
- Sickle cell anemia.
What are the causes of decreased RBC-Cholinesterase level?
- Poisoning is due to insecticides like organophosphorus.
- Congenital cholinesterase deficiency.
- What is the Critical value of the Cholinesterase level?
- The persistently low level in liver disease indicates a poor prognosis.
Questions and answers:
Question 1: What is the transmitter substance for nerve conduction?
Question 2: What is the end product of acetylcholine?