Chapter 17: Autoimmune Diseases:- Systemic Lupus erythematosus (SLE)
SYSTEMIC LUPUS ERYTHEMATOSUS (SLE)
Definition
SLE is a chronic inflammatory autoimmune disease of unknown etiology.
This is the prototype of autoimmune diseases. It is a systemic rheumatic disorder. SLE is a multisystem disease, and it includes:
- Joint involvement.
- Involvement of the connective tissues.
- There is the involvement of the collagen vascular system.
Osler described SLE in detail in 1895.
Epidemiology
- It is estimated 50 to 70 cases per million per year of the population.
- American blacks, Native Americans, Puerto Ricans, and Asian (especially Chinese) have increased the frequency of the SLE.
- SLE was roughly 8 times more common in females than males.
- The prevalence rate is 1 in 700 for females during the age of 20 to 64 years.
- While in black women between the ages of 20 to 64 years is 1 in 245.
- Survival is estimated to be more than 90% at 10 years after the diagnosis.
- High mortality is seen in patients where there is renal and brain involvement.
- The most common cause of death is an infection and renal failure.
Typical features of SLE: These are mostly:
- Young females (childbearing age).
- There are butterfly rashes.
- The patient will have a fever.
- These patients have pain in the joints.
- There is photosensitivity.
- Sometimes the sign and symptoms are puzzling, and the patient may come with only fever and proteinuria.
The salient features of SLE:
- Onset:
- Acute or insidious
- Chronic
- Major Immunologic Features:
- The lupus erythematosus cell phenomenon is positive.
- Increase concentration (titer) of Antinuclear Antibody (ANA), seen in >95% of the patients.
- Positive anti-DNA Ab, particularly double-stranded DNA (dsDNA).
- The complement level is low.
- The deposition of immune complexes (Ag + Ab) can be demonstrated.
- Detection of other autoantibodies.
- Age:- This may occur at any age, but the peak is second to the third decade. This may be seen in children.
- Sex:- It is most common in females with a male: female ratio of 1:9 (another source says female: male =5:1)
One out of 700 white females develops SLE, while black females are 1:245.
One out of 2500 females may have SLE during their lifetime.
- HLA:- DR3 in Caucasians and DR2 in orientals has susceptibility to SLE. Monozygotic twin Caucasians have a higher incidence.
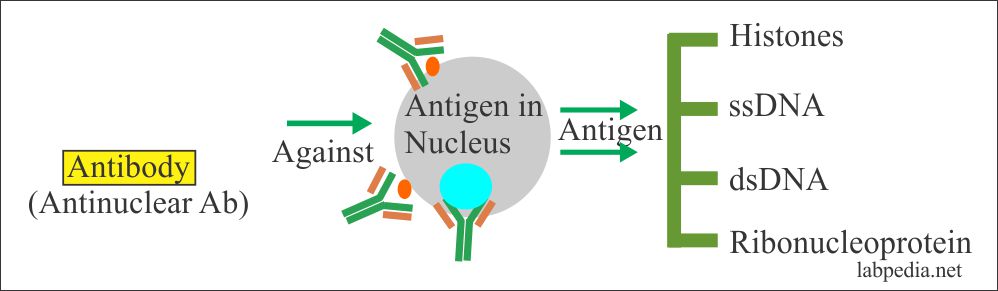
Types of Autoantibodies
- Anti-nuclear antibodies.
- Anti -DNA
- Single-stranded.
- Double-stranded.
- Against RNA.
- Against RNA-associated proteins.
- Against Histones.
- Against the nuclear antigen.
- Antinuclear antibodies (ANA) are virtually positive in all patients. But these are not specific. When ANA is negative, then doubt about the diagnosis.
- DNA and anti-DNA make the immune-complexes and leads to pathological lesions.
- Autoantibodies against formed elements of blood:- RBC, platelets, and neutrophils.
- Smith antigen(sm):- Anti-smith antibody is strongly suggestive of the disease.
- Anti-cardiolipin antibodies are present and are nonspecific.
Etiology of SLE (Pathogenesis)
The cause of SLE is unknown. the primary defect in the regulation of the immune system is considered important in the pathogenesis of SLE.
SLE may be due to the following factors, or these are the hypotheses favoring this disease’s emergence:
1. Genetic Factors
- This disease is 60% in monozygotic twins than dizygotic twins, where it is only 3%.
- There is an increased familial risk, and even normal family members show autoantibodies in 20% of them.
- 60% have inherited low complement (particularly C2 and C4).
- There is an increased incidence of SLE in DR2 and DR3. Also more common in HLA-A1 and B8.
- HLA-DR, and HLA-DQ (class II molecules), have a role in the pathogenesis of SLE.
- SLE patients have an increased frequency of HLA-B8, HLA-DRw2, HLA- DRw3 antigens.
2. Nongenetic Factors (or Environmental Factors)
- There is a history of a man associated animal like a dog that shows dsDNA and his master has SLE.
- Viruses: -It is disputed, but viral particles are positive in affected tissue.
- Drugs: – Some of the drugs are also blamed for this disease, like hydralazine, procainamide, and D-penicillamine.
- Other drugs are chlorpromazine hydrochloride, anticonvulsant drugs, birth control pills, and isoniazid.
- Drug-induced SLE is milder in form than idiopathic SLE.
- Drug procainamide hydrochloride and hydralazine hydrochloride are potent inducers of antinuclear antibodies (ANA) against RBCs and lymphocytes.
- Sex-hormones: – Certain pieces of evidence suggest the role of sex hormones, particularly female hormones. e.g., during reproductive life, the incidence of the disease is 10 times more common. This disease is also more common in pregnancy and during the normal menstrual period.
- This disease is seen between puberty and menopause.
- S/S are worsening during pregnancy and immediately after postpartum.
- When estrogens are given in the postmenopausal period, then SLE incidence increases.
- Estrogen:- It is found that estrogen increases antibodies formation. So female hormones accelerate the disease while male hormones suppress the disease.
- U-V-light: – This can stimulate keratinocytes, and the stimulated cells produce IL-1, which stimulates the B-lymphocytes and T-L.
- UV-light may cause DNA to form thymine dimers. This will change the antigenicity of DNA and may result in the formation of anti-DNA antibodies.
3. Immunologic Factors
This disease is definitely due to a defect in the immune system.
- Some believe that defect is in both B-L and T-L. But this has a lot of controversies.
- B-lymphocytes defect is accepted because there is an increased concentration of immunoglobulins. Also, there is 8-10 times more B-L proliferation, and these B-Lymphocytes react with self and non-self-antigens.
- Hyperactivity of B-L:- This hyperactivity may be due to an inherited defect, and these cells are refractory to immune regulation.
- There is an overactivity of T-helper cells.
- There may be a decreased activity of T-suppressor cells.
- Infectious agents may give rise to polyclonal activation.
Mechanism of Injury in SLE
The injury to various organs and cells may be due to:
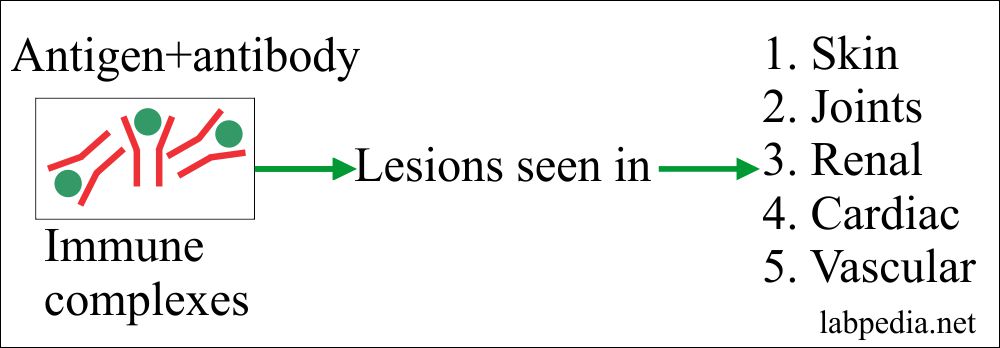
- Type III: – Immune complex disease that may involve almost all organs and common sites are blood vessels, kidneys, and skin.
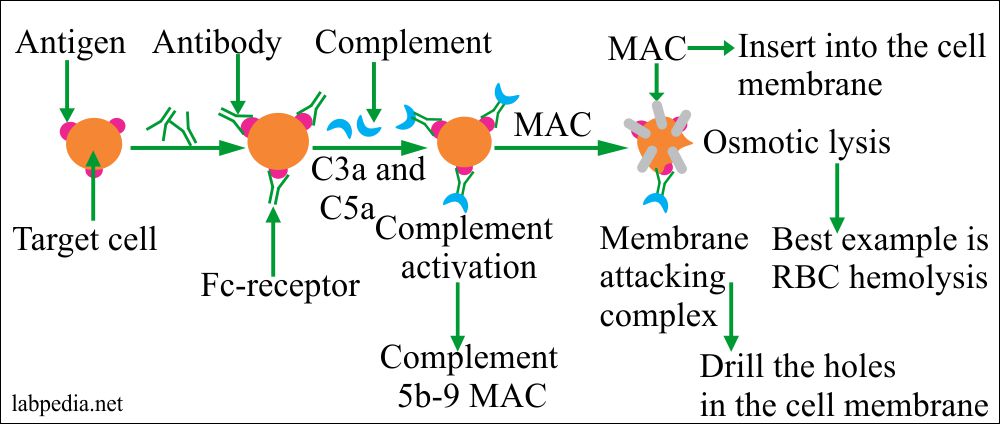
- Type II: – Cytotoxic reaction, which will destroy RBC, platelets, neutrophils, lymphocytes, etc.
- Various self-antigen and autoantibodies with their clinical outcome:
Self-antigen Mechanism Clinical outcome
Red blood cells (RBCs) Antibody to RBCs Hemolytic anemia (Coomb’s positive) Platelets Antibody against platelets Thrombocytopenia White blood cells (WBCs) Antibody against WBCs Leukopenia Clotting factors Antibody against clotting factors Bleeding and prolonged clotting time Blood vessels Antigen-antibody complex Vasculitis Glomerulus antigen Anti-glomerulus antibody Glomerulonephritis (Nephritis) Synovial membrane Antibody against synovium Arthritis Immunoglobulins (Ig) Anti-globulin antibodies Hypergammaglobulinemia Nuclear antigen Antibody against the nuclear proteins Damage to the cells (vascular injury) Nuclear DNA Anti-DNA antibodies Damage to the cells (vascular injury) Nuclear RNA Anti-RNA antibodies Damage to the cells (vascular injury)
American Rheumatism Association Criteria
American Association of rheumatism gave certain criteria for the diagnosis of SLE. These were revised in 1982. When four or more of the following signs and symptoms present, they can label as a case of SLE.
- Malar Rash: – There are butterfly rashes, and these are flat or may be raised. These are present in 1/3 of the cases.
- Discoid Rash: – These are erythematous raised patches. There are keratotic scaling and follicular plugging and, in severe cases, may see atrophic scarring.
- Photosensitivity: – There is an appearance of skin rashes when exposed to sunlight.
- Oral ulcers: – There are painless ulcers in the oral cavity or nasopharynx.
- There is non-erosive arthritis involving 2 or more peripheral joints. These are tender, edematous, and may see effusion.
- Serositis: – There is pleuritis with rub and pain. There may be pericarditis with rub or effusion.
- Renal disorder: – There is proteinuria more than 0.5G / 24 hours or 3+. There are cellular casts like RBC, hemoglobin, or granular casts.
- Neurological disorders:- These patients may have seizures. It has to exclude abscess, drugs, or metabolic disorders, or electrolyte imbalance. Sometimes these patients come with psychosis.
- Hematological disorders:- These patients may have:
- Autoimmune hemolytic Anaemia with increased reticulocytes.
- Leucopenia.
- Lymphopenia.
- There is no evidence of offending drugs.
- Immunologic disorders: These patients may show:
- The L-E cell phenomenon is positive.
- dsDNA-Ab presence.
- Anti-smith-Ab presence.
- False test positive for syphilis.
- ANA: There is an increased titer of ANA.
If 4 of the above criteria present at any time during the course of the disease, a diagnosis of SLE can be made with 90% specificity and 97% sensitivity.
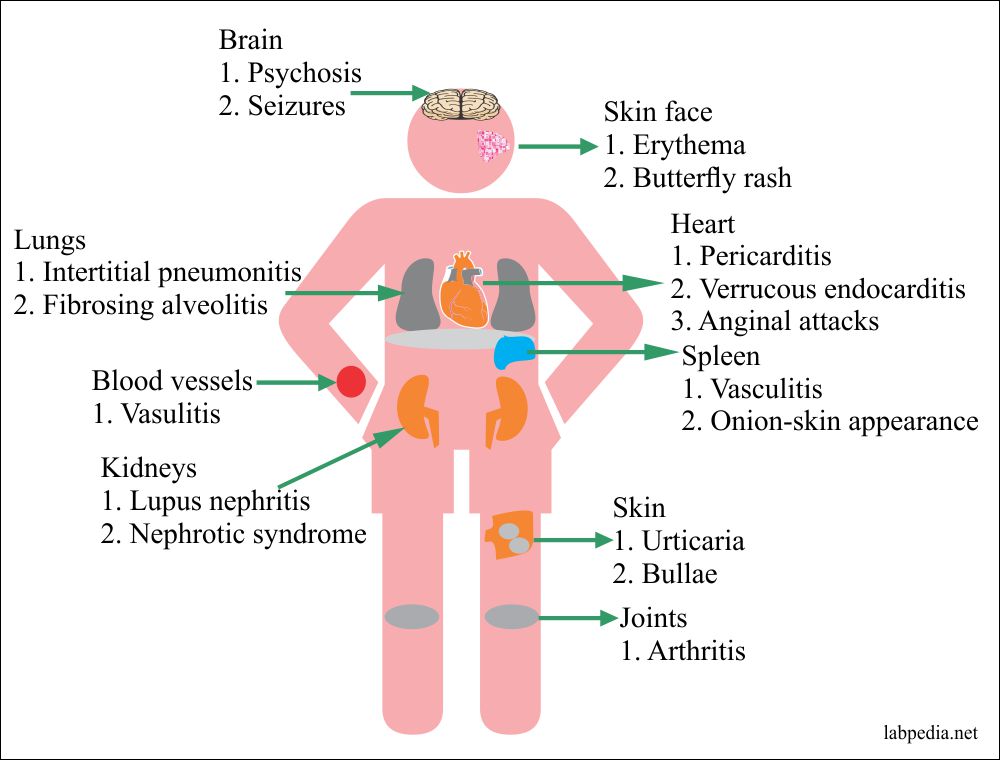
Target Organs
In SLE, almost all the organs are involved. The most common organs are:-
| Disease | % occurrence of the disease |
| Skin | 80 to 90 |
| Joints | 80 to 90 |
| Kidneys | 70 |
| Lymphadenopathy | 60 |
| GIT | 30 |
| Heart | 50 |
| Liver | 20 |
| Spleen | 20 |
| CNS | 20 |
| Lungs | 10 to 20 |
| Eyes | 20 |
| Serosal membranes | 4 |
The characteristic lesions of Systemic Lupus erythematosus are seen in:
- Blood vessels.
- Kidneys
- Connective tissue.
- Skin
Signs and Symptoms of Systemic Lupus erythematosus
1. SLE may be acute or chronic inflammation.
- There may be typical mild illnesses limited to photosensitivity, facial rash, and diffuse arthritis to life-threatening involvement of the kidneys, heart, lungs, or the brain.
- In the early stages, it is difficult to differentiate from:
-
- Polymyositis.
- Progressive systemic sclerosis.
- Sjogren’s syndrome.
- Raynaud’s phenomenon.
- Rheumatoid arthritis.
2. Lymphadenopathy
-
- There is peripheral and axial lymphadenopathy. Also, there is splenomegaly.
- Patients with SLE may develop lymphoma in comparison to the general population.
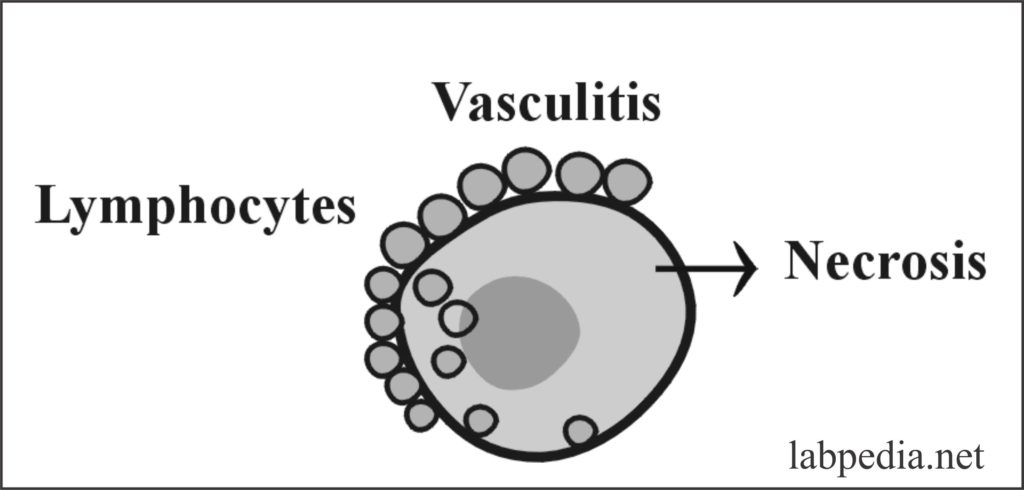
3. Blood Vessels
- There is necrotizing vasculitis with the presence of fibrinoid necrosis and accompanied by perivascular lymphocytic infiltrate.
- The chronic stage is followed by fibrosis. These affected blood vessels can show the presence of Ig, C3, and DNA.
4. Kidneys
- 60-70% show no changes in the light microscope, while 100% show E/M and immunofluorescence evidence.
- This involvement of the kidney may be monitored by:-
-
-
- Abnormal urine analysis.
- Increase the concentration of dsDNA antibodies.
- Low complement level, especially C4.
-
WHO has given the classification of Systemic lupus erythematosus nephritis as follows:
Class – I: Biochemical evidence:
- This is a rare condition where on light microcopy, E/M and immunofluorescence are normal where there will be biochemical evidence of the renal involvement.
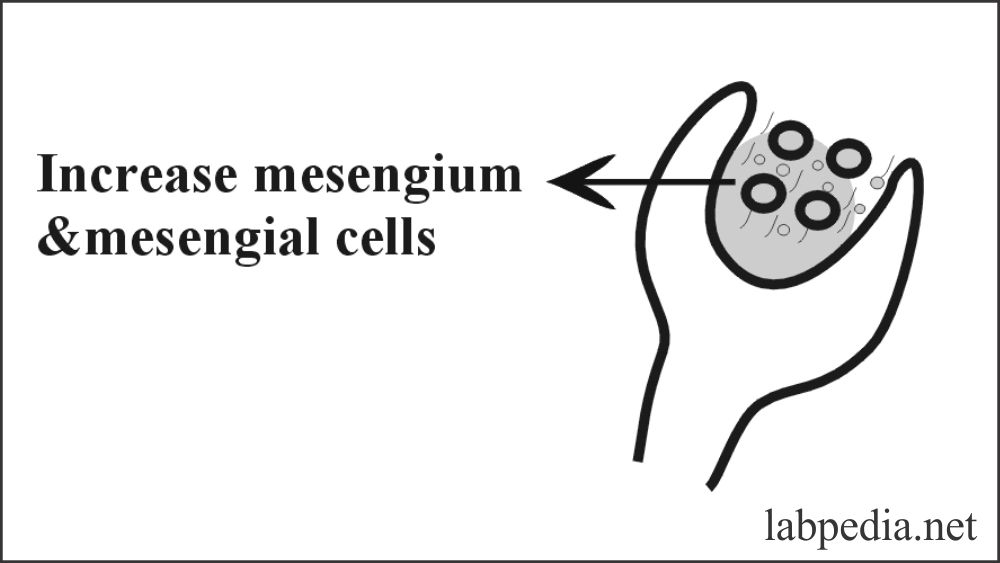
Class-II – Mesengial lupus glomerulonephritis:
- This is seen in 25% of the cases and is the mildest form with minimal S/S. There are mild haematuria and proteinuria.
- Microscopically there is an increase in mesengium, increased mesengial cells. Granular deposits of Ig and complement can be demonstrated.
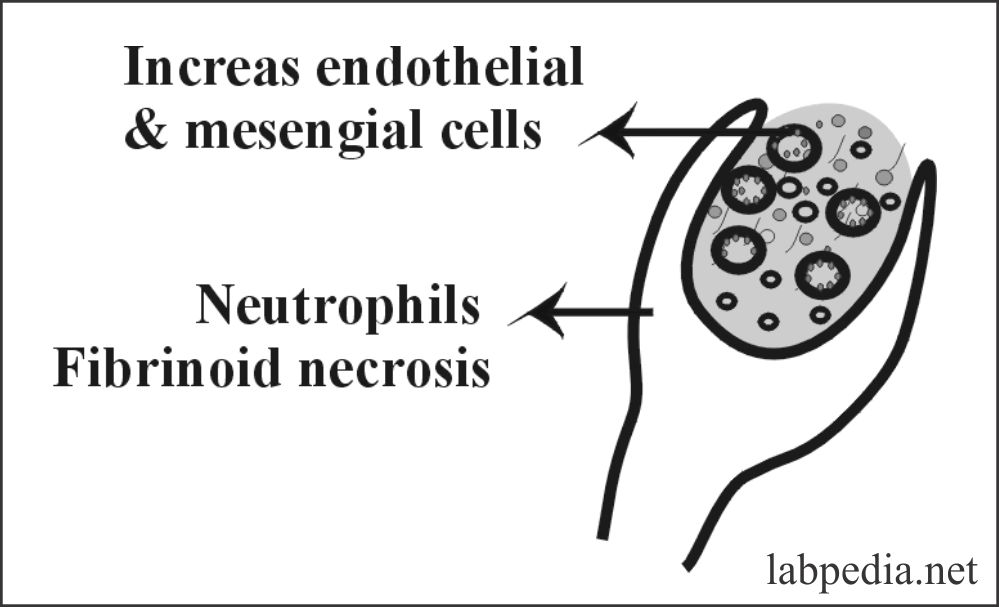
Class III – Focal proliferative glomerulonephritis
- This is seen in 20% of the cases. There is 50% involvement of the glomeruli, and also there is partly involvement of the glomeruli. The patient will have proteinuria and haematuria.
- Microscopically there is partly involvement of glomeruli, increased endothelial and mesengial cells. There is a neutrophil infiltration. Sometimes fibrinoid necrosis and thrombosis may be seen.
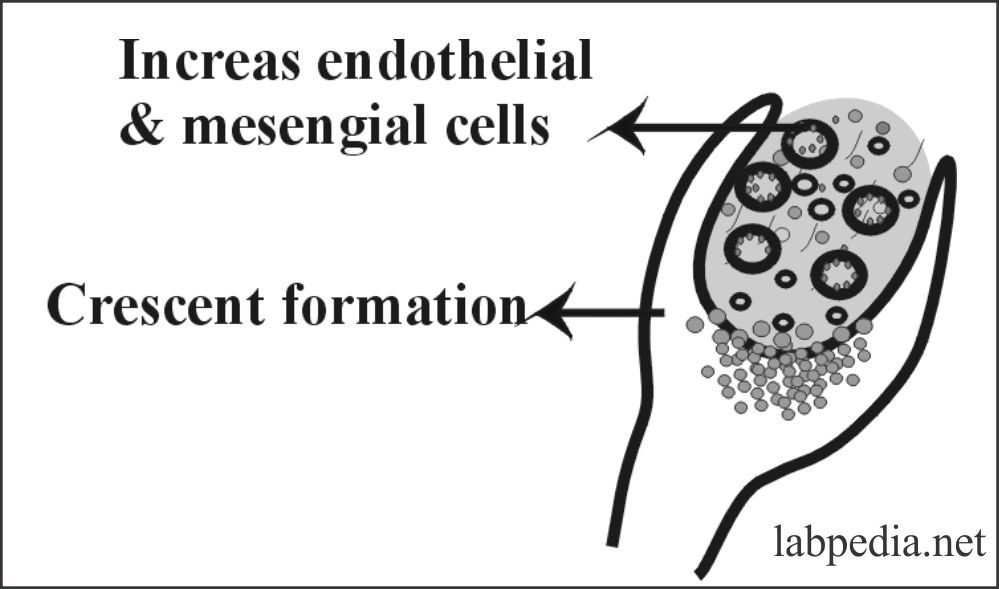
Class IV – Diffuse proliferative glomerulonephritis
- This is seen in 35-40% of the case. This is the most serious condition. Patients show gross haematuria and proteinuria. 50% have hypertension, and these patients develop nephrotic syndrome.
- Microscopically there is diffuse involvement of the glomeruli with an increase in endothelial cells, mesengial cells, and sometimes epithelial cells leading to the crescent formation. There may be fibrinoid necrosis and thrombosis.
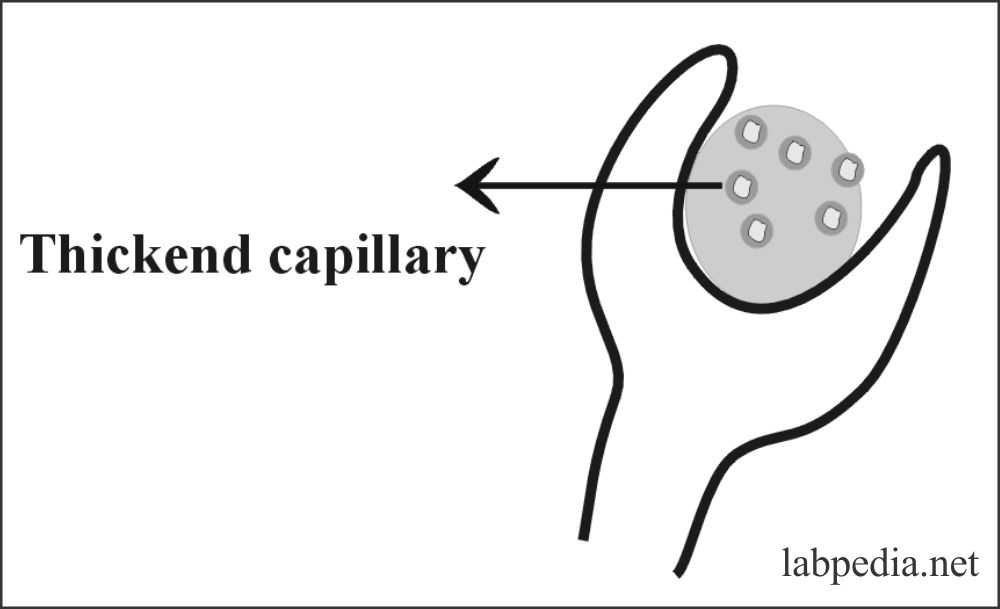
Class V- Membranous glomerulonephritis
- This is seen in 15% of the cases. Patients have severe proteinuria and become nephrotic.
- Microscopically there is a widespread thickening of capillary walls.
Mechanism of injury in the kidneys in SLE:
- The kidney is mainly a typed III immune complex disease, and the complexes are (DNA + Anti-DNA).
WHO classification of the renal involvement:
| The histological type of nephritis | Class of Glomerulonephritis | Frequency % | Clinical findings (Diagnosis) |
| Normal | I | <5 | Only biochemical evidence |
| Mesengial GN | II | 15 | Mild hematuria and proteinuria |
| Focal proliferative GN | III | 20 | Hematuria and proteinuria |
| Diffuse proliferative GN | IV | 50 | Hematuria and proteinuria, and hypertension |
| Membranous GN | V | 15 | Hematuria and nephrotic syndrome |
5. Cardiovascular System
- Inflammation of the myocardium in SLE patients can produce persistent tachycardia and, occasionally, intractable congestive heart failure.
- Ischemic disease or, more commonly, atherosclerosis of the coronary blood vessels are seen.
- These patients may have pericarditis. Another common lesion is non-bacterial verrucous endocarditis, which shows vegetations of 1-4mm in diameter.
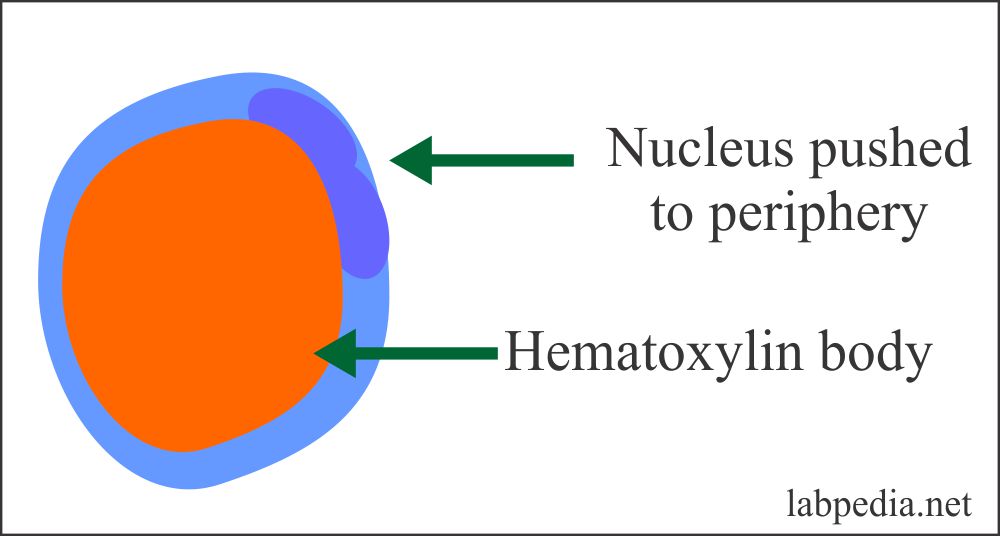
- These vegetations microscopically show fibrinoid necrosis, neutrophil infiltration, and fibroblastic proliferation. There is hematoxylin bodies presence (Bacterial vegetations are larger, measuring 0.5-2 cm in diameter).
- These patients may have anginal attacks due to coronary thickening.
6. Joints and musculoskeletal system
- There is the involvement of the peripheral joints, characterized by tenderness, swelling, or effusion.
- Both small and large joints are involved. Chronic arthritis may result in disability and deformity seen in SLE.
- Osteonecrosis develops in one-fourth of the patients.
- Microscopically there is non-erosive synovitis with little deformity. There are fibrinous exudates and mainly neutrophil infiltrates. If the joint fluid is aspirated, it will show mainly neutrophils.
7. Skin
- There is erythema, butterfly rashes (on nose and cheek)—extremities, and trunk show urticaria and bullae. There are hypopigmented areas without the presence of a scar called sub-acute lupus.
- Microscopically there is basal cell degeneration, and perivascular mononuclear infiltrate. Dermis shows fibrosis. Ig can be demonstrated at the dermo-epidermal junction.
8. Lungs
- There are interstitial pneumonitis and diffuse fibrosing alveolitis. This may be acute or chronic or subacute. There is pleuritis, and in 50% of the cases, there is pleural effusion.
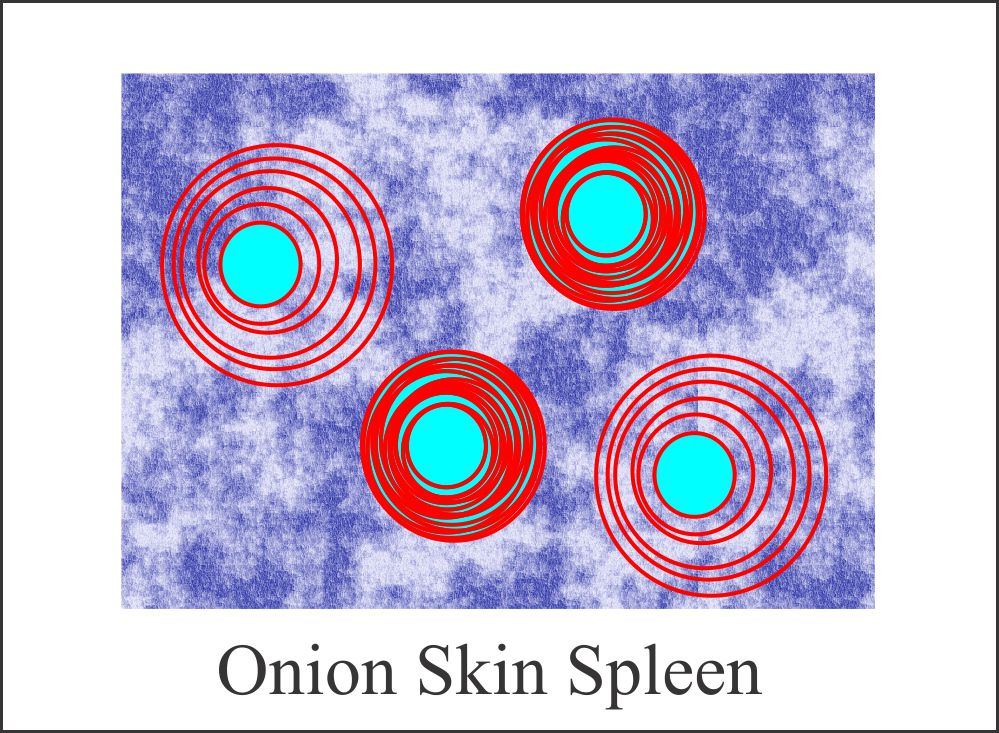
9. Spleen
- There are increased capillary thickening and follicular hyperplasia. The infiltration by plasma cells increases.
- There may be massive hemoptysis due to alveolar hemorrhage.
- Microscopically there is perivascular fibrosis, and it gives an “onion skin” appearance.
10. Central Nervous System:
- The patient may have psychiatric or neurologic symptoms. There may be a presentation of psychosis and seizures. 25% of signs are related to acute vasculitis, which leads to infarct and hemorrhage.
- The most common abnormalities are mental function disturbances, ranging from mild confusion, memory deficiency, and impairment of orientation and perception to psychiatric disturbances such as hypomania, delirium, and schizophrenia. Some patients may have epilepsy and severe headache.
11. Gastrointestinal system:
- There are nonspecific symptoms due to GIT involvement in SLE. Acute crises due to vasculitis are less common.
- Acute and chronic pancreatitis may be seen.
12. Chronic Discoid Lupus Erythematosus:
- There is only skin manifestation.
13. Effects of the pregnancy:
- In SLE patients, premature delivery and spontaneous abortion are increased during pregnancy. Mother and fetus are at increased risk of various complications during and after the pregnancy.
- Pregnant ladies are at an increased risk of a flare-up of the disease.
- Passive transfer of the antibodies across the placenta to the fetus may produce abnormalities like hepatosplenomegaly, cytopenia, and photosensitivity in the newborn.
Signs and symptoms summary SLE:
| Clinical involvement of organs | Clinical presentation |
| Systemic | Fever, Fatigue, and weight loss |
| Musculoskeletal system | Arthritis |
| Cutaneous | Malar rash, photosensitivity, and alopecia |
| Hematological | Anemia, leucopenia, and thrombocytopenia |
| Renal | Glomerulonephritis |
| Lungs | Pleuritis and pneumonitis |
| Heart | Pericarditis and valvular dysfunction |
| Central nervous system | Psychosis, stroke, and seizures |
The course of the disease: – This is unpredictable.
- The patient may go into remission.
- 90% of survival is seen for one year.
- 80% of survival is seen for 5 years.
- 76% of survival is seen for 10 years.
The life-threatening complications are:
- Renal diseases.
- Involvement of the CNS.
- Low platelet and white cell count.
- Autoimmune hemolytic anemia.
The most common cause of death is Renal Failure, followed by:-
- Intercurrent infection.
- Cardiac failure.
- Pulmonary diseases.
- Involvement of CNS.
- The cause of death in renal failure:
Renal disease grade Death due to uremia Overall death in renal failure Mesengial GN II 0% 18% Focal proliferative GN III 11% 30% Diffuse proliferative GN IV 36% 58% Membranous GN V 6% 38%
Diagnosis
- Blood examination:
- Blood shows normochromic and normocytic anemia.
- Occasionally Coomb’s test is positive and indicates hemolytic anemia.
- There are lymphopenia and thrombocytopenia.
- Complement C3 and C4 are decreased (low level).
- Serum immunoglobulins are raised.
- Urine analysis shows haematuria and proteinuria with the presence of renal cast.
- Typically ESR is raised while CRP will be negative.
- ANA:- Antinuclear antibodies are positive in 99% of the cases. If these are negative, then SLE diagnosis is in doubt.
- ANA may be positive in other diseases like:
- Sjogren syndrome = 68%.
- Scleroderma = 60-70%.
- Rheumatoid arthritis = 20-40%
- ANA may be positive in other diseases like:
- Immunofluorescence techniques on the frozen section:
- Four patterns are seen, and specific for SLE is RIM formation.
- Anti-dsDNA antibodies are specific for SLE diagnosis, and these are positive in 50% to 70% of the cases.
- Anti-Smith antibodies are diagnostic but positive in 30% of the cases.
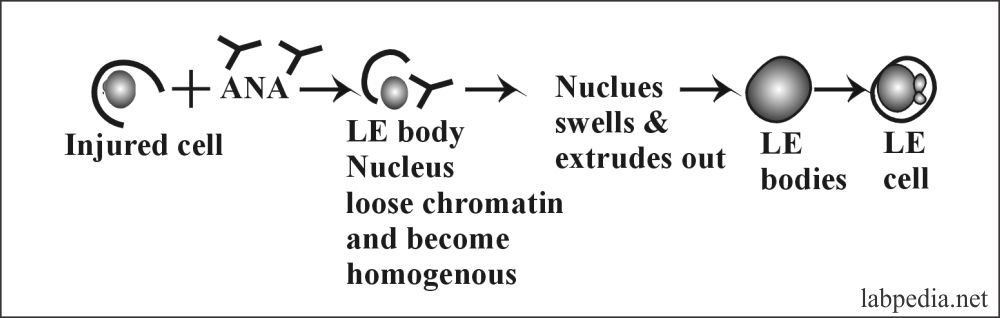
- Lupus-Erythematous cell phenomenon (LE Cell).
Hargreave described this in 1948. The patients’ blood shows hematoxylin bodies in the monocytes/neutrophils pushing the nucleus to the periphery.
Procedure and Mechanism of LE cell phenomenon:
- Procedure:
Take the blood of patients 5-10ml. - It is traumatized by glass beads or glass rods to expose the nucleus to antinuclear antibodies in patients’ serum.
- Complement is activated, and it causes the death of the nucleus, and it becomes a homogenous hematoxylin color body, and the nucleus is pushed to the periphery.
Treatment
-
- Patients are treated according to the manifestation of the disease.
- For arthritis, Nonsteroidal anti-inflammatory drugs and aspirin may be used.
- For cutaneous manifestation, anti-malarial (Hydrochloroquin) can be used.
- Corticosteroids alone or in combination with cytotoxic drugs like cyclophosphamide and azathioprine may be used in case of life-threatening manifestation.