Chapter 15: Transplantation and Rejection Phenomenon
TRANSPLANTATION AND REJECTION
Definition
- Transplantation is used to replace an organ that has undergone an irreversible pathological process, threatening the patient’s life or considerably hampers life quality.
- Transplantation is a biological object like hair, skin, kidney. and heart. The transplanted material is called a graft.
- This may be used cosmetically as a hair transplant and skin graft.
Indications
- The main indication is organ failure.
- The indications are different for the different organs.
Indications in various organs for the transplantation according to their demands:
| Organ needed according to their priorities |
Reason for the transplantation |
| Kidney | End-stage renal failure |
| Liver | Cirrhosis, biliary atresia, and cancer |
| Blood vessels | Coronary disease |
| Heart | Cardiac failure in the terminal stage |
| Lung | Cystic fibrosis, pulmonary hypertension |
| Bone marrow | Leukemia and immunodeficiency |
| Bone | In limb-sparing bone tumors |
| Pancreas or islet cells | Diabetes |
| Intestine | Cancer |
| Heart-lung | The diseases of heart and lung |
| Heart valve | Aortic and mitral valve defects |
| Skin | History of burn |
| Cornea | Keratitis, dystrophy, non-healing corneal ulcer |
History of the organ transplantation:
| Organ transplanted | When it was first transplanted |
| Intestine | 1987 |
| Lungs | 1983 |
| Heart and lung | 1981 |
| Heart | 1968 |
| Pancreas | 1968 |
| Liver | 1967 |
| Kidney | 1954 |
| Cornea | 1905 |
| Skin | 1870 |
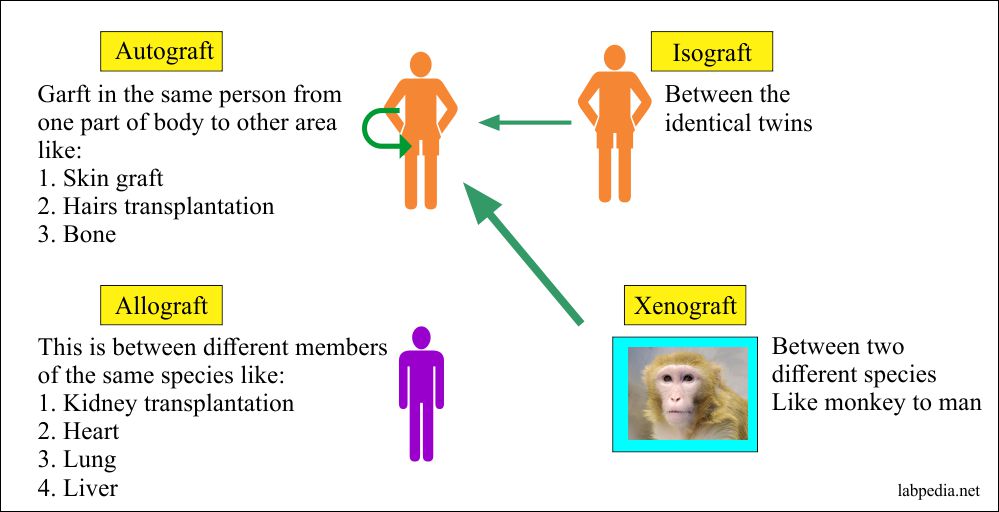
Types of Graft
- Autograft: These are 100% successful, with no chances for rejection.
- These are from self to self and from one place to another place in the same individual. The best example is the skin graft.
- Isograft Autograft: This is done in the same individual like skin graft or blood: This is between two genetically identical individuals or twins. This is also a successful graft. The genetic makeup of the donor and the recipient are identical.
- The above two grafts survive for an indefinite period of time.
- Allograft(Homograft): This is done between the same species mean man to man, which is the most common procedure, e.g., kidney, liver, and blood transfusion.
- The two individuals are not identical. The donor is alive or cadaver.
- Xenograft(Heterograft): This is done between two different species, like animals, to man. If we succeed in this category in the future, then various organs will be available commercially. We have to control the graft’s immunological problems, and then we can get organs from the animals.
- Still, we will have nonimmunological problems in xenograft like:
- Donor organ size.
- Physiological differences.
- Transmission of animal diseases.
- Ethics of the xenografting.
Transplantation of various organs and donors:
Graft types Genetic makeup Type of the tissue Type of the donor
Autograft No difference (same) Autologous (from the same individual) The donor is the same individual Isograft Identical Isologus The donor is identical twins or near-identical individual Allograft Not 100% identical Allogenic (from the same species) The donor is from the same species Xenograft Entirely different, xenogenic Heterologous (from different species) Tissue from the different species like a monkey to man
- Still, we will have nonimmunological problems in xenograft like:
Data of the tissue transplantation:
1997 = 158,000 medical patients have end-stage kidney.
1988 = 100,000 patients have organ transplantation.
Mid = 1989 >18000 were on the waiting list.
October 26, 1994, = Patients list was 36,000, out of this 26,895 were waiting for the kidney transplant, the liver was 3,815,
the heart transplant was 2,863.
Graft Survival in the USA
| Organ | Survival rate |
| Kidney | 80 to 90% out of 9736 patients |
| Cornea | 79% |
| Liver | 40 to 50% out of 3064 patients |
| Heart | 70% out of 2172 patients |
| Bone marrow | 80% |
| Lung | Low out of 535 patients |
Mechanism of Rejection
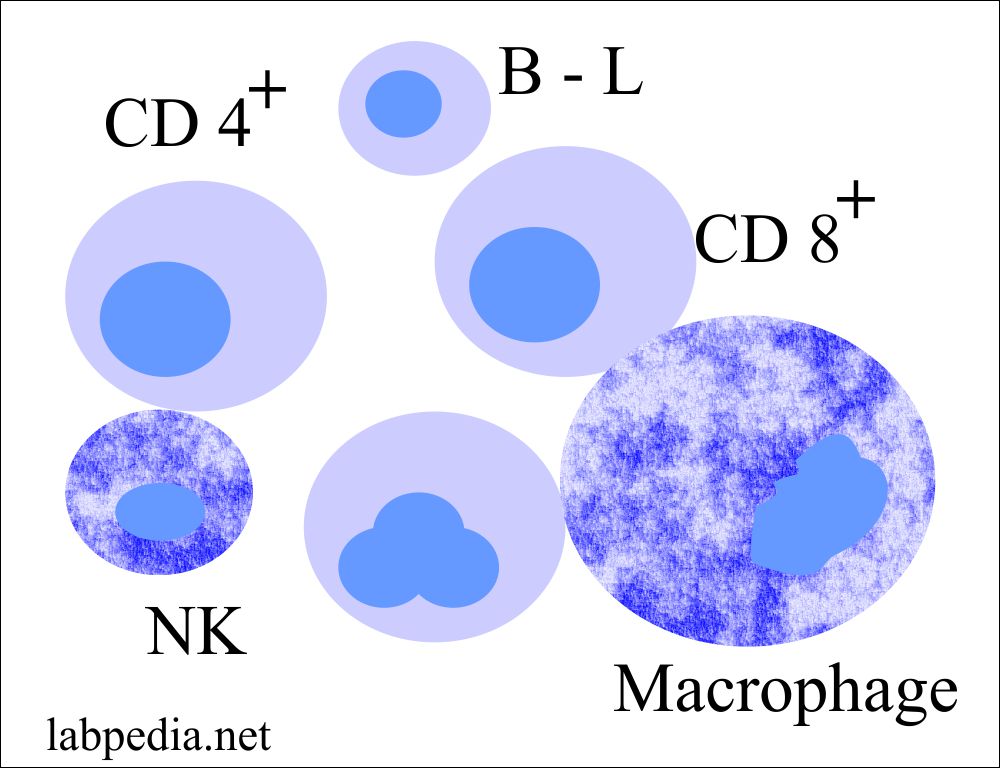
- Rejection is purely an immunologic reaction. The biopsy of the rejected organs invariably shows an inflammatory infiltrate. The analysis of such infiltrate by monoclonal antibodies shows the heterogeneous composition of the cellular infiltrates. CD4+ cells, CD8+ cells, macrophages, B-lymphocytes, and NK cells.
- Histocompatibility antigen (HLA) is present on the surface of white blood cells, platelets, and fixed tissue of the body.
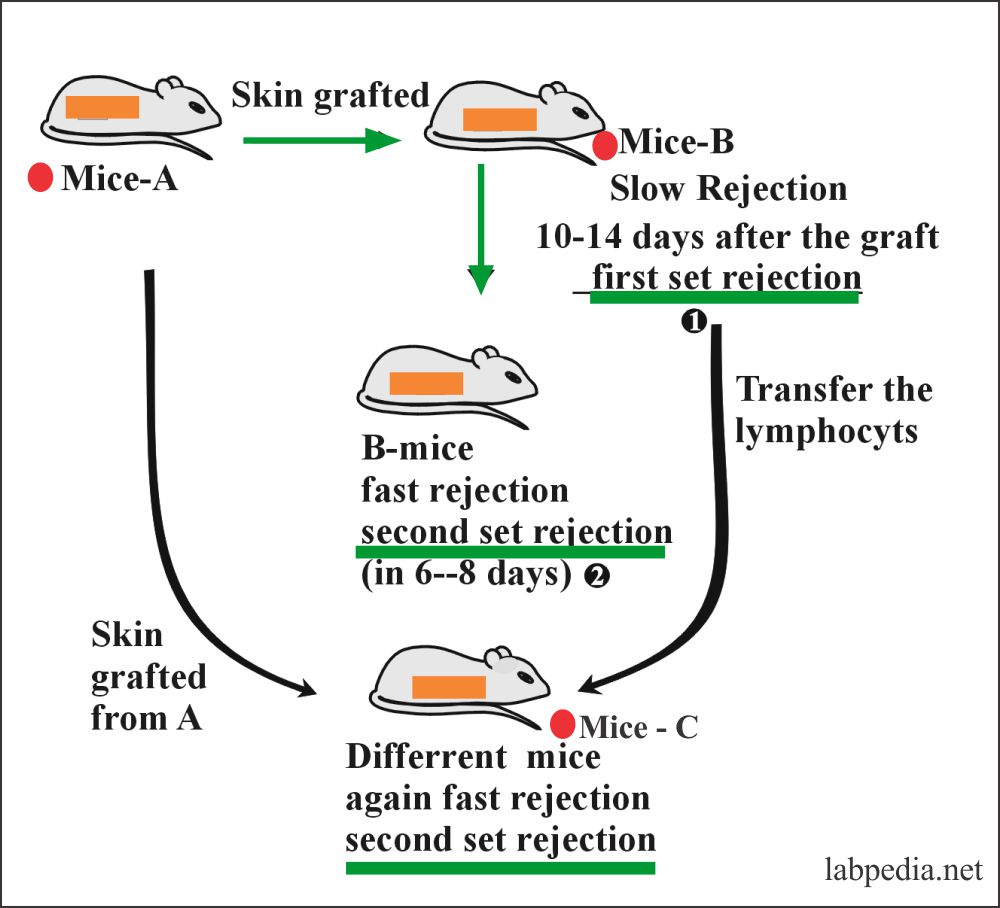
- Medawar, in world war II tried to attempt to skin graft in burn patients from their own bodies. These skin grafts were successful. At the same time, a skin graft from another person was rejected in about 4 weeks. He did an experiment on mice and described first set rejection and second set rejection.
There are three clinical observations for the rejection of transplantation:
-
- Medawar experiment and his skin grafting the burning soldier in world war II. He did the famous experiments on the mice described below.
- The second discovery was by Dausset, van Rood and Payne in 1958 found that sera of the multigravida women contained antibody, which agglutinated human leukocytes despite ABO compatibility. The production of antibodies in these mothers has occurred due to isoimmunization of pregnancy. White cells have entered the maternal circulation and stimulated the antibody’s production to the parental antigen on fetal white cells like RBcs isoimmunization. However, the disease in the newborn was rare.
- In 1965 Dausset gave a concept and postulated that the genetic basis for controlling 10 histocompatibility antigens has a major role in tissue transplantation. It provided the basis for tissue and white cell typing used in the RBCs typing. Now the transplantation is successful due to HLA typing.
Medawar experiment for the Rejection phenomenon:
- First, set rejection or slow rejection, which takes 10-14 days.
- The second set of rejection is fast or accelerated rejection.
First-set rejection: When mice B grafted first time from mice A, then graft is rejected slowly, 10-14 days and this is called first set rejection.
This example also shows that the immune system, which produces graft rejection, also displays memory and specificity.
Second-set rejection: When mice are regrafted from the same donor, then graft is rejected more rapidly (6-8 days) and is called Second set rejection.
Even if lymphocytes from Mice B, when transfused to mice C, show second set rejection. But when graft from mice A is put on Mice C again, there is First set rejection.
The basic principle involved in the transplantation:
The recognition of the foreignness of any substance, external or internal, gives rise to the same sequence of the reaction as we have seen in the immune response. So in tissue transplantation, both humoral and cellular mechanisms of immunity are activated.
The basic goal of the transplantation is the long survival of the graft. This will depend upon the donor’s similarities and the recipient’s genetic (antigenic similarity) structure.
The graft’s next survival depends upon the graft’s nature, whether nucleated (capable of survival) or non-nucleated (incapable of replication).
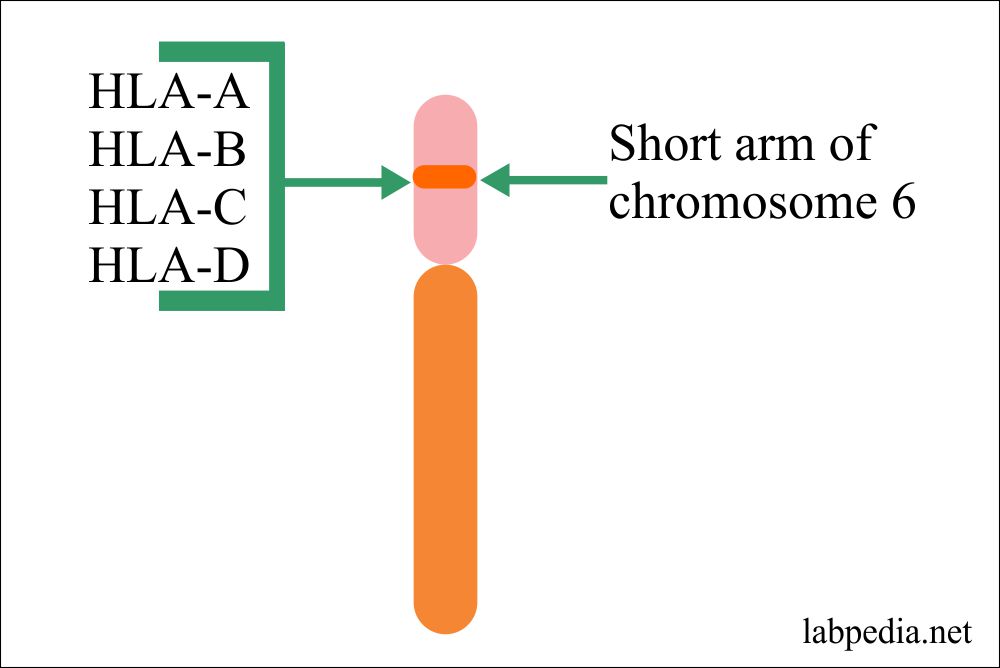
Histocompatibility antigens (HLA):
Antigens primarily responsible for the rejection of genetically different tissues, know as histocompatibility antigens, and the gene coding for these antigens is referred to as histocompatibility genes.
Some of these antigens provoke an immune response and are called major histocompatibility complex (MHC).
There are 30 histocompatibility gene loci (major histocompatibility complex, MHC), causing rejection at different rates.
In humans, MHC is called human leukocyte antigen (HLA). This is controlled by MHC or supergene, which includes several loci closely linked on the short arm of chromosome 6.
MHC is divided into four major regions:
- HLA-A.
- HLA-B.
- HLA-C.
- HLA-D.
- MHC is divided into 4 major regions and form molecules.
- A, B, C regions codes for the MHC-I molecule.
- These three principle loci A, B, C, and their antigens are numbered as 1, 2, 3, etc.
- These class I molecules consists of a single heavy chain and a light chain.
- D- region codes for MHC-II molecule. These are divided into three families:
- HLA-DR.
- HLA-DQ.
- HLA-DP.
- A, B, C regions codes for the MHC-I molecule.
- MHC-I = Present on most of the nucleated cells, RBCs, and platelets.
- MHC-II = These are restricted to antigen-presenting cells (APC, dendritic cells, and activated macrophages), B-lymphocytes, vascular endothelium, and some species, T-lymphocytes.
- IFN-γ and TNF are powerful inducers of the MHC expression.
The role of the HLA system in the transplantation:
In this case, the foreign MHC molecules can directly stimulate the T- lymphocytes. These T-lymphocytes respond against foreign proteins, which are process into peptides and presented on the surface of the recipient’s APC in association with MHC molecules.
Both MHC class, I and II molecules, are the T-L target that regulates the immune response.
- The MHC class I molecules regulate the interaction between cytolytic T-L and the target cells.
- The MHC class II molecule restricts regulatory T-L activity, including helper, suppressor, and amplifier subsets.
- MHC class II molecule regulate the interaction between helper T-L and antigen-presenting cells (APCs).
- Cytotoxic T-cells directed against class I antigens are inhibited by CD 8+ cells.
- Cytotoxic T-cells directed against MHC class II molecules are inhibited by CD 4+ cells.
- Class III molecules have no relation with class I and class II molecules, except their genetic linkage.
Distribution of the HLA- class I and II molecules on different cells of the body:
| HLA- class I molecule | Expressed on the surface of |
| Expressed | All body nucleated cells |
| variably expressed | Hepatocytes |
| weekly expressed | Parathyroid, pituitary, pancreatic islet cells, Myocardial muscles, skeletal muscles, thyroid (endocrine), gastric mucosa, and mature granulocytes |
| Not expressed | RBCs, corneal endothelium, exocrine pancreas, villus of trophoblast, some duodenal Brunner’s gland, and parotid acinar cell |
| HLA- class 2 molecule | |
| Expressed | B-L, activated T-L, renal glomeruli, and tubules, Langerhans cell, dendritic cells, deep epithelial cells of duodenum, ileum, and appendix, immature granulocytes, tonsils, epididymis |
| HLA-DR expressed | Monocytes, macrophages, and vascular endothelium |
| Not expressed | RBCs, hepatocytes, biliary epithelium, myocardial and skeletal muscles, smooth muscles, epithelial cells of the stomach, esophagus, and Brunner’ssd glands, spermatozoa, epithelium of prostate, urinary bladder, and ureter, platelets, neurons, mature granulocytes, and resting T-L |
The comparison of HLA, ABO blood group, and Rh-system needed in the transplantation:
| Characteristic feature | ABO blood group | Rh- blood group system | HLA system |
| Genetic locus | Single | Complex | Complex and linked genes |
| Polymorphism | Moderate | Extensive | Extensive |
| Distribution in the tissue | RBC, salivary gland, and many tissues | RBCs only | White blood cells and other many tissues |
| Importance in organ transplantation |
|
Hemolytic disease of the newborn |
|
| Diagnosis | By serological methods | By serological method |
|
| Treatment | No need | Specific anti-IgG antibody (Anti-RhoGAM) | Immunosuppressive therapy:
|
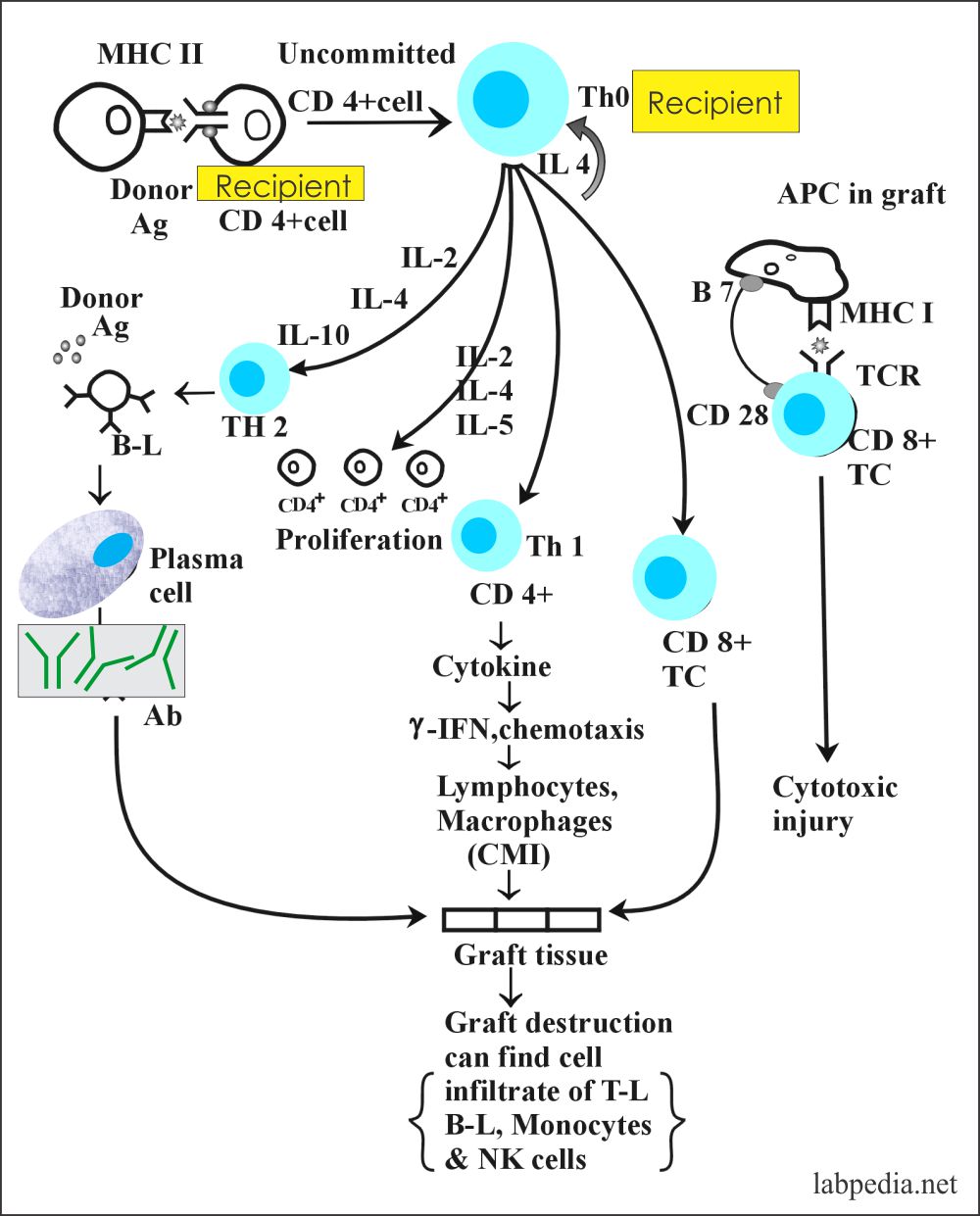
The role of T – lymphocytes in Rejection of the graft:
- Rejection reactions are induced by the recipient Th (CD4+) cells, which recognize donor MHC-I & II molecules.
- Donor Ag and cytokines IL-2 stimulate uncommitted recipient CD4+ cells, or IL-4 will differentiate CD4+ cells to Th1 or Th2 to initiate a series of immune responses.
- Th2 cells mainly secrete IL-4 and IL-10 and initiate Ab production by B-lymphocytes.
- Th1 cells secrete IL-2 and IFN-γ, which stimulates T-cytotoxic cell (CD8+), enhances class-I expression, and induces the class-II molecule’s expression donor tissue to activate macrophagic cells.
- Activated macrophagic cells release IL-1, TNF-α.
The role of the B – lymphocytes in rejection:
There is a main role of T-lymphocytes, but B-lymphocytes can also mediate rejection, and the possibilities are:
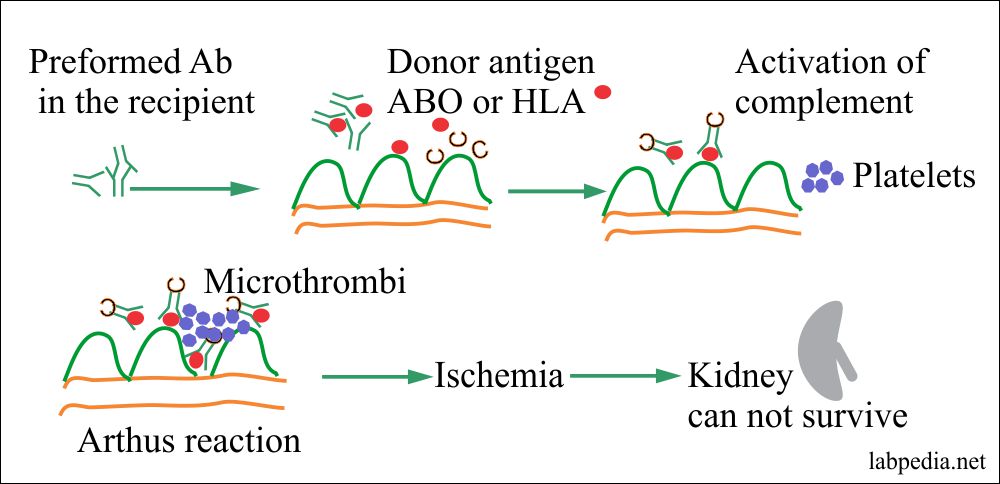
A. Presence of preformed Antibody:
- The recipient may have performed Ab, which may occur by giving multiple blood transfusions, pregnancy, and infections. Platelets and white blood cells are rich in HLA-Ag.
- These preformed Abs gives rise to hyperacute rejection, and this may be due to Arthus’ reaction.
- The cross-match can avoid the hyperacute rejection the cross-match by mixed lymphocytes reaction (MLR).
- Mixed lymphocyte reaction:
- Recipient serum + donor lymphocytes are mixed in the culture medium. This procedure is called a mixed lymphocyte reaction (MLR) and is the basis for the cross match.
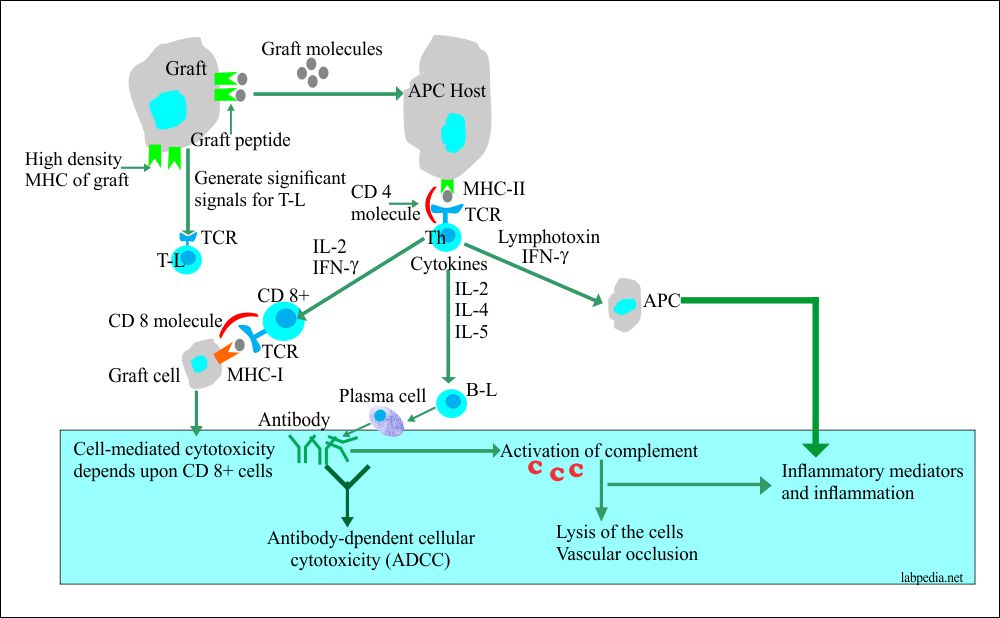
B. Formation of Antibody:
Exposure of HLA-I & II Ag of donors by the recipient give rise to Ab formation, and these may cause damage by:-
- Cytotoxic reaction, ADCC.
- Immune complex disease.
The initial target is graft vasculature, and some referred to this as rejection vasculitis.
Criteria for the success of Transplantation:
- The following criteria are the need for successful tissue transplantation:
- MHC -Major histocompatible (HLA-antigens) antigens called transplantation antigens.
- This can be checked by the mixed lymphocytic reaction and micro cytotoxicity test.
- Minor histocompatibility Ag is H antigens.
- ABO system – This is also very critical for the success of the graft.
- Immunosuppressive medication is also needed. The most commonly used are:
- Steroids are anti-inflammatory, suppress activated macrophages, decrease the APC functions, and reduce MHC expression.
- Cyclosporin interferes with lymphokine production.
- Azathioprine prevents the proliferation of immune activated cells.
- MHC -Major histocompatible (HLA-antigens) antigens called transplantation antigens.
Morphological Classification of the rejection:
- Hyperacute
- Acute:
- Acute cellular.
- Acute humoral (vasculitis)
- Subacute
- Chronic
Differentiating points of different type of rejection:
| Type | Time after Transplantation | Possible Mechanism |
| Hyperacute | Minutes to hours | Preformed anti donor antibodies and complement |
| Accelerated acute | 1-5 days (days) | T-Lymphocytes (reactivation of the sensitized T-L) |
| Acute | From 3rd week (days to weeks) | T-Lymphocytes (primary activation of T-L) |
| Chronic | Months to year |
Antibody and Complement (adhesion molecule) (causes are unclear, immune complexes, antibodies, slow cellular reaction) recurrence of the disease. |
Table XXII – Type of Rejections and differentiating points
Hyperacute Rejection
- Hyperacute rejection is due to the presence of preformed Ab in the recipient that is directed against Ag of the donor organs.
- The anti-HLA antibodies form from the previous blood transfusion, multiple pregnancies, or the rejection of the previous transplant.
- Antibodies against the ABO blood group system can also cause hyperacute rejection.
- Hyperacute rejection can also be mediated by Ab directed against donor HLA-I molecules. The origin of which can be traced to previous leukocytes containing blood transfusion.
- Mechanism:
- Preformed antibodies fix the complement, damage the endothelium of the blood vessels. This damage allows the leakage of cells and fluids, cause the aggregation of the platelets.
- These aggregates block the microvasculature, depriving the graft of blood supply.
- Classically there is an Arthus reaction.
Clinically
This rejection occurs within minutes to hours, so it is recognized by the surgeon at the table, particularly in a kidney transplant.
The kidney will be cyanotic, mottled, and flaccid.
Few drops of urine will form, and these may be bloody.
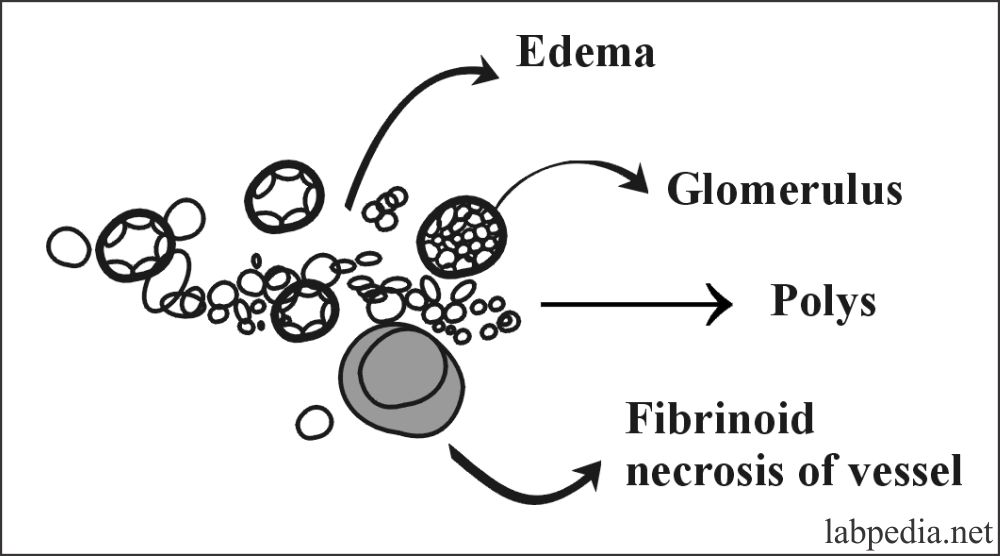
Microscopic Examination of graft tissue (kidney) shows:
- There is Interstitial edema.
- Infiltration by neutrophils around blood vessels, glomeruli, and peritubular capillaries.
- Intravenous fibrin- platelet thrombi may be seen.
- There is fibrinoid necrosis of arterioles.
End Result
The kidney cortex undergoes infarction, then necrosis, and the result is the non-functioning kidney.
Prevention:
- This can be prevented by blood group ABO matching and by cross-match.
- In this procedure, take the serum of the recipient for The detection of cytotoxic donor antibodies.
Acute Rejection
Acute Rejection can occur within a day or suddenly, in months or years, accompanied by renal failure signs and symptoms.
Mechanism:
- Acute Rejection may be due to :
- T-L (cell-mediated immunity).
- B-L (Humoral).
- Morphologically acute rejection is of two types:
-
- Humoral (Vasculitis).
- Cell-mediated (acute cellular).
-
- This acute rejection is due to the primary activation of T- lymphocytes.
- T-lymphocytes activation leads to the triggering of various effector mechanisms.
- There is accelerated cell-mediated rejection of the graft.
- In this case, CD4+ and CD8+ and humoral B- lymphocytes are involved.
- CD8+ cells may directly react to the graft and destroy the graft by their cytotoxicity.
- T-lymphocytes produce lymphokines to stimulate the monocytes.
- The monocytes cause delayed hypersensitivity reaction and destroy the graft.
- B-lymphocytes differentiate to plasma cells and form antibodies against the vessel wall antigens, causing graft rejection.
Signs and Symptoms
- The patient will have a fever and chills.
- There is oliguria.
- There is a swollen graft.
Acute rejection usually occurs after stopping immunosuppressive therapy.
A. Acute Cellular Rejection
This is cell-mediated due to T-L. It occurs in the initial months, and the patient develops abrupt signs/symptoms of renal failure.
Microscopic Examination
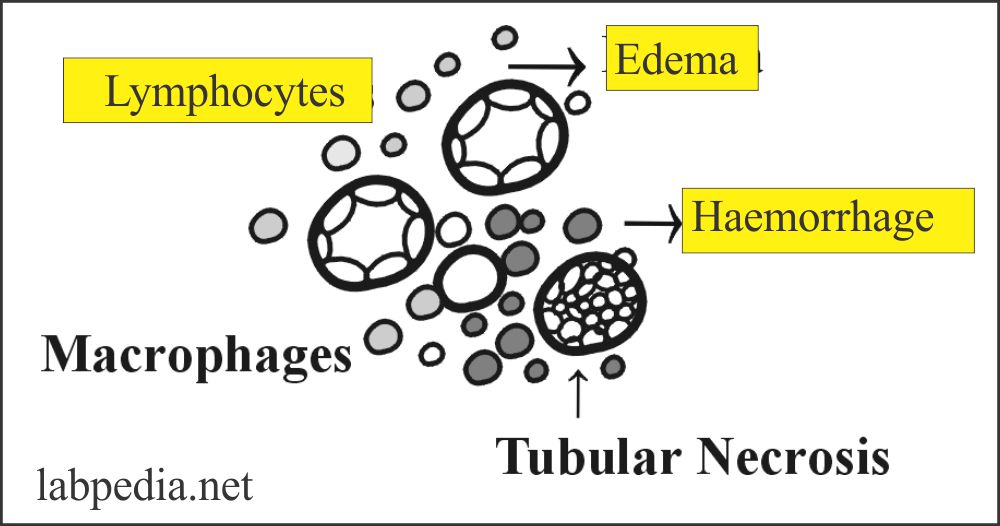
There is edema; mononuclear cellular infiltrates of T-L (CD4+, CD8+, and macrophages). There may be mild hemorrhage and focal tubular necrosis. But there is no evidence of vasculitis.
Treatment
This acute cellular rejection can be treated by giving cyclosporin, and there will be a prompt response.
B. Acute (Humoral) Vasculitis
This occurs in the first ten months or when immunosuppressive therapy is stopped.
Microscopic Examination
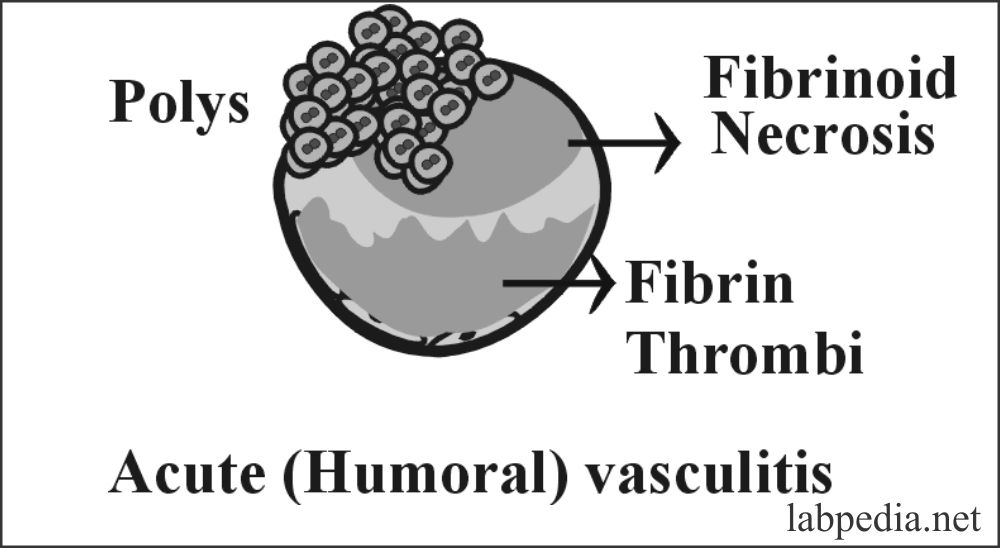
There is predominantly necrotizing vasculitis.
There is an infiltration of neutrophils and the formation of fibrin thrombi. There is necrosis of glomeruli and cortical arterial thrombosis. The presence of Immunoglobulin and complement can be demonstrated.
Treatment
There is no response to increasing doses of immunosuppressive therapy. This is the reason that on biopsy, this should be separated and diagnosed.
Subacute Rejection (Vasculitis)
This also occurs in the first few months, and this is a common condition.
Clinically
The patient will have altered renal function suggesting an episode of rejection.
Microscopically main changes are:
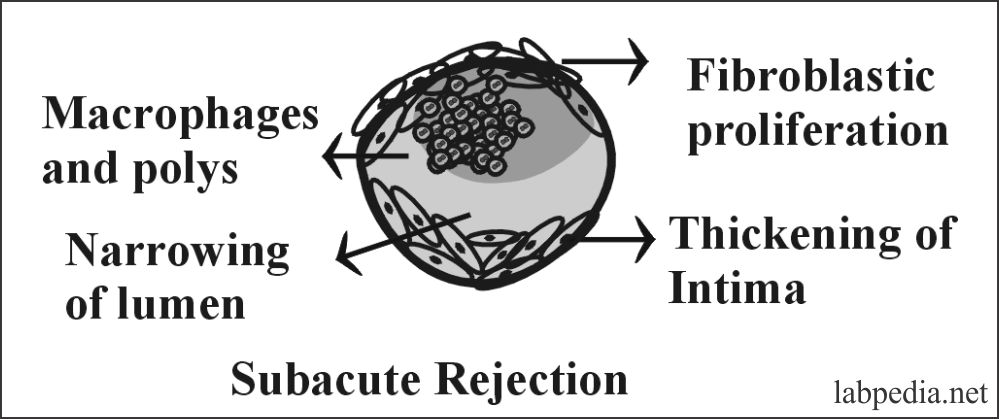
- These are mainly in the intima. There are proliferation and thickening of the intima.
- There is the proliferation of fibroblasts, myocytes, and foamy macrophages, leading to luminal narrowing.
- There may be infiltrating of neutrophils and mononuclear phagocytic cells.
- The walls of these arteries show the deposition of Ig and complement.
Chronic Rejection
- Chronic rejection occurs months to years post-transplantation.
- Chronic Rejection will be followed by a steadily increasing level of creatinine over a period of 4-6 months.
- Chronic rejection appears after months or years of successful transplantation. It is a major cause of long-term graft loss, but its pathophysiology is poorly understood.
- This process is controlled by the various growth factors, such as TGB-β, released due to immune or other injuries to the transplant.
Microscopically:
- In this case, both cell-mediated and humoral immunity are involved in the rejection of the graft.
- The cardinal feature is blood vessels luminal obstruction of the graft tissue.
- The changes are mainly vascular which, maybe early damage to the endothelium.
- There is diffuse intimal fibrosis (proliferation of the intimal smooth muscles), particularly in cortical arteries. This will lead to ischemia and changes in the glomeruli.
- There is a formation of scar tissue throughout the grafted tissue.
- There is tubular atrophy, and interstitial fibrosis further leads to a decrease in renal parenchyma.
- Cell infiltrate is not a major feature of chronic rejection, although macrophages play an important role through cytokine release (IL-1, IL-6, and TNF-a).
- There is the presence of mononuclear phagocytes, plasma cells, lymphocytes, and eosinophils.
Types of graft reaction, their duration, and etiology:
| Type of graft rejection | The time period for rejection | Mechanism of rejection | Pathological causes of rejection |
| Hyperacute rejection | Minutes to hours (may be seen at the table) | This is due to preformed antibodies (Humoral) |
|
| Acute | Days to weeks |
|
There is a reaction of T-L and B-L to graft tissue. |
| Chronic | Months to years |
|
|
Methods for Increasing Graft Survival:
- ABO blood group compatibility is the most important factor.
- HLA tissue typing:– Minimizing HLA disparity of donor and recipient leads to successful transplantation.
- When donor/recipient HLA types match, the successful survival is 70%, but when these are mismatched, then survival of the graft is low.
- Cadaveric kidney survival for 5 years is 33.50%, but this may be more in living relatives donated organs.
- Cross-matching of recipient serum with donor lymphocytes prevents hyperacute rejection due to preformed Abs.
Post Operative Therapy
- All transplanted recipients need immunosuppressive treatment except identical twins.
- Corticosteroids are given for maintenance therapy or bolus at the time of rejection. These are anti-inflammatory cells that decrease the number of circulating lymphocytes. These also interfere with lymphokines’ production; Down regulate the expression of cytokine genes like IL1, 2, 3,4,5,8, TNFa, and GM-CSF.
- Antimetabolites and Alkylating agents:- These control DNA & RNA functions and leads to the death of rapidly dividing lymphocytes, e.g., Azathioprine and Cyclophosphamide.
- Cyclosporin:- These are cyclic peptide antibiotics produced by fungi. These are varying effective in inhibiting T-L.
- Anti-Lymphocytes globulin and anti-thymocyte globulin can destroy T-Lymphocytes.
The complication of Post Operative Therapy
- These patients are prone to develop an infection, and 25% die due to sepsis in the kidney.
- 6% develop malignancy like skin cancers and 50% lymphoma or sarcomas.
Transplantation of the various organs:
Transplantation of Hemopoietic Cells (B M Transplantation)
Bone marrow transplantation is done in:
- Hematological malignancies like leukemia like acute myelocytic and acute lymphoblastic.
- In case lymphomatous malignancies like Hodgkin’s and non-Hodgkin’s lymphomas.
- Aplastic anemia.
- Certain immune deficiency status.
- Sickle cell anemia.
Procedure
Bone marrow transplant is the second most common transplantation.
The donor may be autograft or allograft. A donor is a living person, and the sample may be obtained by needle aspiration.
Before marrow is transplanted from the donor and the recipient is radiated with a lethal dose to destroy malignant cells or create an aplastic condition.
Major Problems
A major problem of Bone Marrow transplantation and occasionally in the liver are:
- Transplant rejection.
- Graft VS host disease (GVD).
Blood transfusion:
This is the most common type of transplantation. It helps to save the life of so many recipients daily.
The donor may be an autograft, in which blood is taken from the patient before the surgery and, if needed, can be given to the patient. These donors are always living.
Most donors are allografts. Blood from identical twins can also be used.
Indications for the blood transfusions are:
- Hemorrhage.
- Blood loss due to any cause.
- Patients with severe anemia.
The blood transfusion is always successful when a proper crossmatch is done.
Kidney transplantation:
A kidney transplant is the most common procedure.
In this case, the kidney can be gotten from the living donor, where one kidney will compensate for one kidney’s loss.
In this case, the graft is an allograft. The donor may be living or cadaveric.
These patients are put on the immunosuppressive therapy, and that will prolong the life.
Heart transplant:
The first successful transplant was done in South Africa in 1967. In the USA this was done in 1981.
The donors are allografts, and these are mostly cadaveric; these are the patient with brain dead.
Heart transplantation is indicated in:
- Idiopathic cardiomyopathy in children and adults.
- Congenital heart diseases in the children.
- Coronary disease in the adult.
These patients are treated with immunosuppressive therapy. Initial survival for one year was 20%. Now it has increased to 85 to 90%. At the same time, 5-year survival is 75 to 80%.
Herat valve transplant:
Xenogenic valve replacement is the standard procedure for aortic and mitral valve defects.
These valves’ source is bovine (cow) or porcine (pig); these valves are chemically or physically modified to reduce the antigenicity.
Patients who get these modified xenogenic valves do not get immunosuppressive therapy because the rejection is minimal or non-existent.
Skin graft / Transplanttion:
The source of the skin is autograft or allograft. But mostly, the donors are self (autograft). The donors are living source.
The skin allografts will show the rejection phenomenon because of the extremely high density of the MHC class I molecule antigens. These allografts are supported by immunosuppressive therapy.
This grafting or transplantation is done in burn cases. This is done to control the infection and get a normal skin look.
The graft from the self and identical twins is very successful. In the case of allograft, immunosuppressive therapy is needed.
Liver transplantation:
The donors are living where part of the liver is taken. The cadaveric liver can also be transplanted. This was very common in China, where the liver was provided by the criminals who were undergoing a death sentence.
Potential liver transplant patients should not have extrahepatic disease or infection.
Liver transplantation is done in:
- Congenital abnormalities.
- Malignancies of the liver.
- Metabolic disorders.
- In the case of cirrhosis. These patients are good candidates.
- Liver failure due to drugs.
- Alcoholic liver with cirrhosis.
- Liver diseases due to hepatotropic viruses like HBV and HCV.
- Autoimmune liver diseases.
- Diseases of the bile ducts in adults.
Liver cells can regenerate. So part of the liver can be transplanted, and the remaining liver will regenerate. The liver from one donor can be split and transplanted to two patients.
Immunosuppressive therapy is needed. Overall first-year survival is 60%.
This procedure’s major complication is biliary tract fistula or leak, which may be seen in 30% to 50% of the patients.
One of the liver transplantation complications is graft-versus-host disease.
Lungs transplantation:
The lung transplant is difficult because of technical and immunological problems. The donor and the recipient bronchi should be of the same caliber. Lungs are susceptible to ischemic damage.
Sometimes lungs and heart transplantation is done simultaneously; this combined procedure is less difficult
then only the lung.
This is usually done in patients with:
- Cystic fibrosis.
- Interstitial fibrosis.
- Emphysema.
The graft is allograft or from an identical twin. The donors are brain dead patients.
Lung infection and sepsis are widespread in donors.
Immunosuppressive therapy is needed. The lung transplant prolongs the life of the patient.
Many lung recipient patients died due to massive infection and sepsis.
Hair transplantation:
This usually by autograft of the living donor.
The hairs are taken from the lower back part of the head (occipital area).
This is advised in a bald area of the head. This is mostly a successful autograft.
Cornea transplant:
The corneal transplant was a common form of therapy for many years. The first corneal transplant was established in New York in 1944. The corneal transplant has a high success rate.
Cornea lake the blood vessels, so there is a reasonably low concentration of the MHC class I molecule (antigens). Almost nearly in the absence of MHC class II molecules (antigens), graft rejection is minimal. These grafts are made small and avoid making contact with the vascular area.
This is also known as keratoplasty. This is allograft or graft from the identical twins.
Mostly the cornea is taken from the cadaver.
The indication for the cornea transplant are:
- Scarring of the eye due to infections.
- Eye injury due to chemical burn.
- Non-healing corneal ulcers.
- Corneal edema.
- Thining and distortion of the cornea leading to keratoconus.
- Vision loss due to Fuchs dystrophy.
Immunosuppressive therapy is not needed. There is a complete visual recovery because the cornea is an avascular structure. Only in 20% of the cases rejection is seen.
Pancreas transplant:
There may be full pancreatic tissue or only islet cell transplantation.
The pancreas as a whole transplant is not successful. While islet cells transplant into retroperitoneal tissue has a success rate.
Graft-versus-host disease (GVHD):
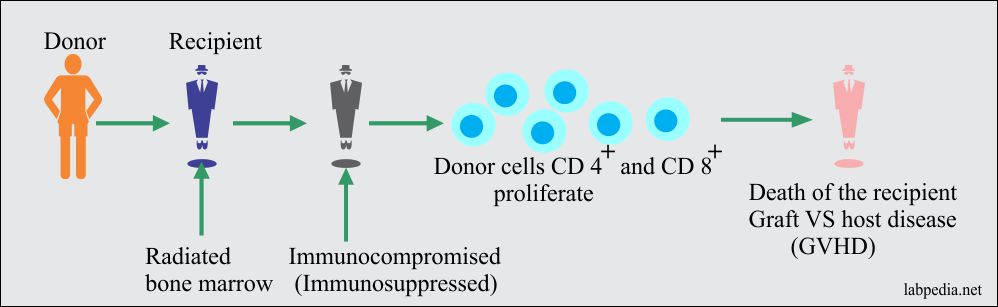
GVHD may be due to blood transfusion or transplantation in severely immunocompromised or immunosuppressed patients.
The degree of immunodeficiency in the host, the number of transfused immunocompetent lymphocytes determine whether or not GVHD will occur.
Mechanism of Graft VS Host Disease (GVHD):
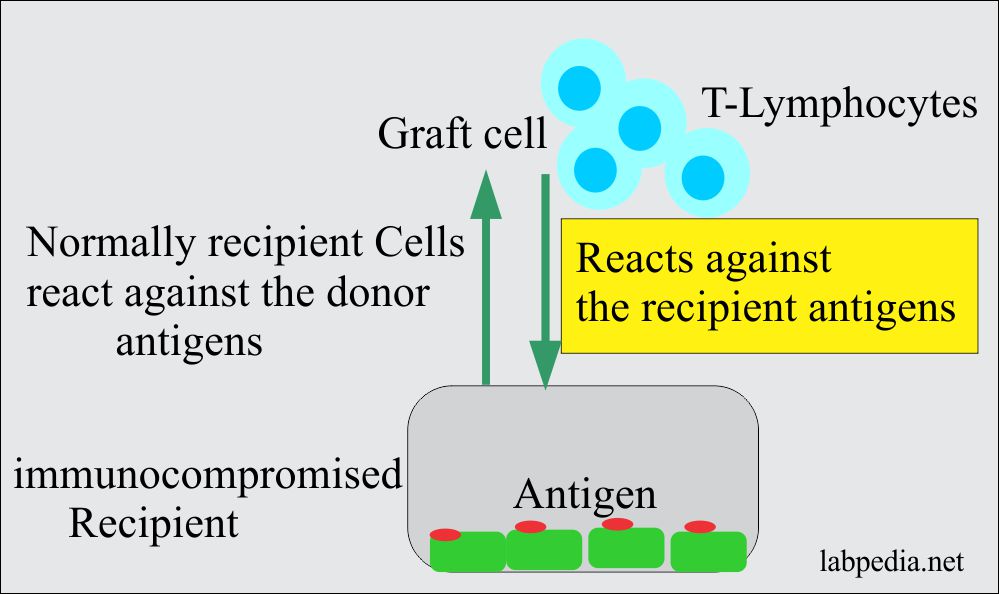
This immunological condition arises when a graft contains immunocompetent cells are engrafted into an immunologically incompetent recipient. Immuno-competent cells of the graft recognize Ag (alloantigen) of the recipient and are activated.
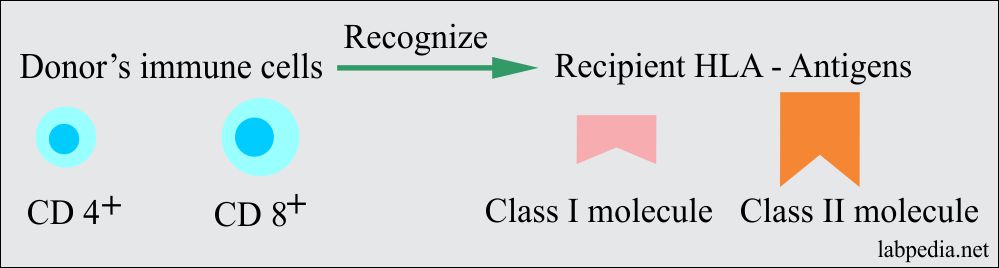
When GVH becomes symptomatic, the term graft versus host disease (GVHD) is a more appropriate name. Donors (immune cells) recognize recipient HLA – Antigen as foreign and reacts against them with sensitization, and anti-recipient CD4+ and anti-recipient CD8+ are generated. Normally recipient cells react against the donor antigens.
Donors CD4+ and CD8+ are Activated against recipient HLA Ag (Class-I Molecule and Class-II Molecule).
In this case, the recipient can not reject the transfused lymphocytes; the grafted lymphocytes may destroy the host tissues and eventually death. The greater the antigenic difference, the more severe reaction will be seen.
GVHD is seen in:
- Immunodeficient.
- Immunosuppressed with severe lymphocytopenia and bone marrow depression.
- Instead of chemotherapy at the time of bone marrow transplantation, 20% to 50% of the patient will develop Acute GVHD.
- 20% to 40% of these patients will die of GVHD or infection.
Classification of the graft versus host disease (GVHD):
Graft versus Host disease is of two types:
- Acute disease (Acute GVHD).
- Chronic disease (Chronic GVHD).
Acute Graft VS host disease (GVHD):
It occurs in the first 1-2 months after transplantation (first 100 days).
Any organ may be involved, and the main problem is the immune system’s involvement and epithelium of skin, liver, and intestine.
Infections are prevalent.
Signs and Symptoms
- GVHD causes an inflammatory response. Post transfusion symptoms start within 3 to 30 days after the transfusion.
- Skin shows generalized rashes.
- Liver: – There is bile duct destruction, and the patient develops jaundice.
- Intestine: – There is mucosal ulceration of the gut, and patients may develop bloody diarrhea.
Chronic graft versus host disease (GVHD):
It appears after at least 2-3 months after transplantation.
This may follow acute or insidious onset.
Signs and Symptoms
- The chronic form looks like collagen vascular disease with skin changes such as erythema and cutaneous ulcers.
- There is extensive cutaneous injury and maybe fibrosis in the dermis. There is desquamation and blister formation.
- The liver shows chronic liver disease like cholestatic jaundice, and alkaline phosphates level is raised. This is due to bile duct degeneration and cholestasis.
- Gastrointestinal tract:- The patient may have abdominal pain and diarrhea with life-threatening electrolytes imbalance. There may be esophageal stricture.
- Recurrent infections are also common.
Treatment
- Immunosuppressive therapy: The most effective treatment to prevent acute GVHD is a combination of methotrexate and cyclosporin. While treatment of established GVHD is with methylprednisolone, cyclosporin, and or anti-thymocyte globulin.
- Careful HLA typing is needed.
- Removal of the mature T – lymphocytes from the graft.
Important
If donor T lymphocytes from bone marrow are depleted, then GVHD will be prevented.