Ceruloplasmin, Copper Toxicity and Wilson’s Disease
Ceruloplasmin
What sample is needed for Ceruloplasmin?
- Venous blood is needed to prepare the serum.
- Fresh serum is preferred.
- It can be stored at 4 °C for 3 days.
- It can be stored at -20 °C for up to 4 weeks.
What are the precautions for Ceruloplasmin?
- Avoid lipemic and hemolyzed samples.
What are the Indications for Ceruloplasmin?
- This is an acute-phase protein.
- This test is done to diagnose Wilson’s disease.
How will you define Ceruloplasmin?
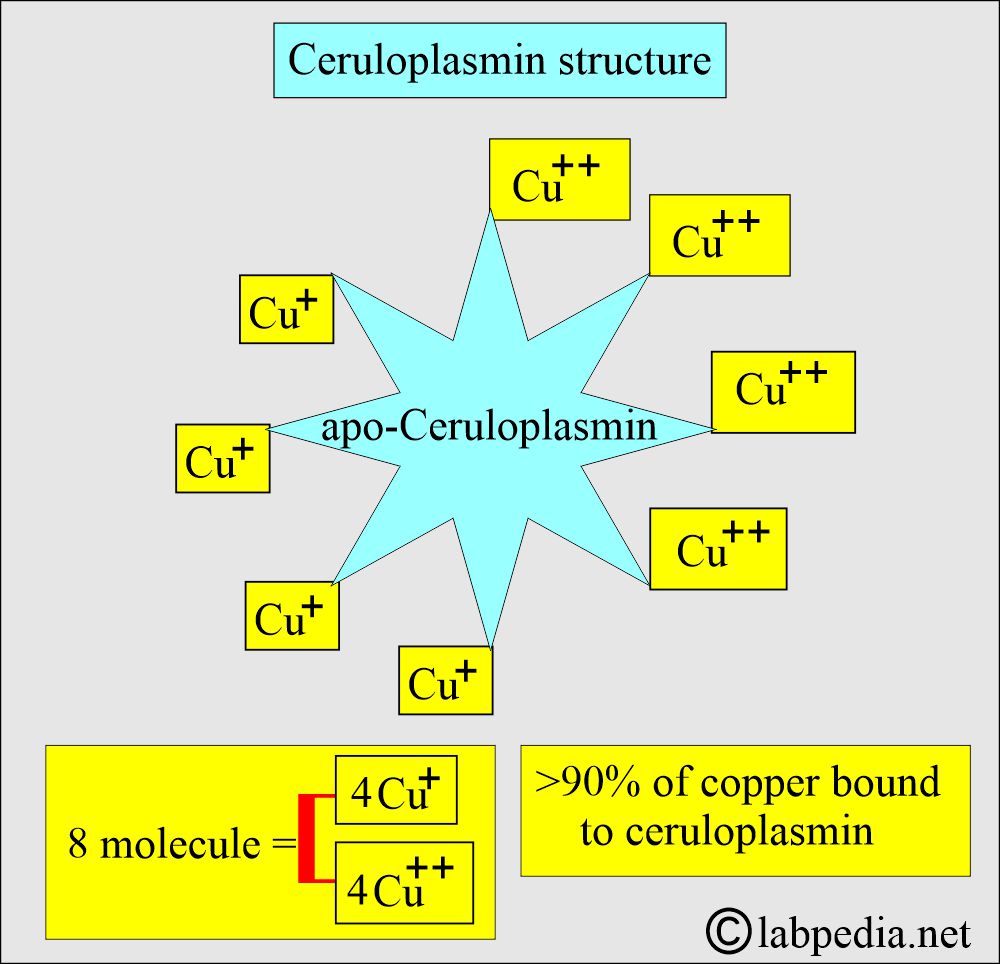
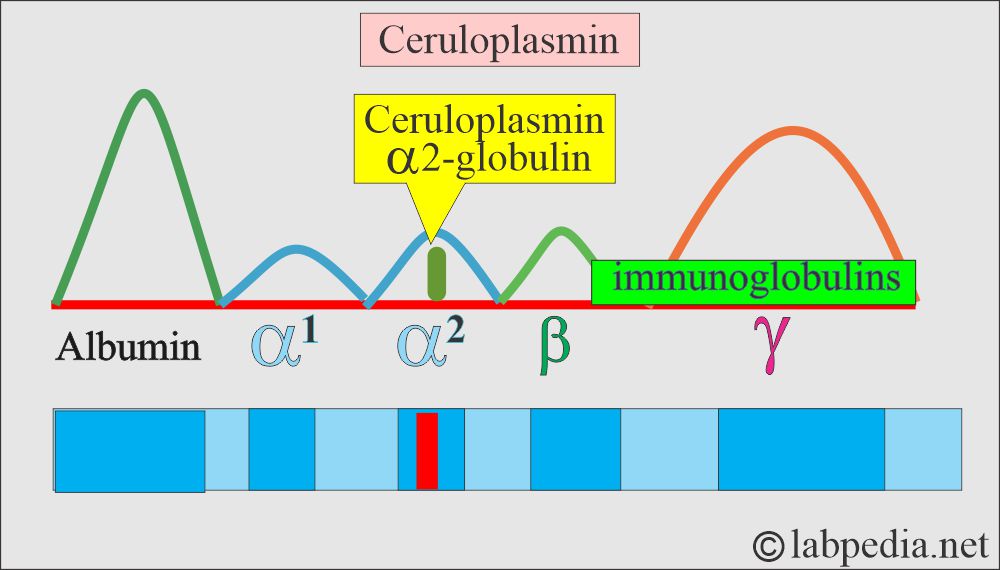
- Ceruloplasmin is a copper-containing, α2-glycoprotein with enzymatic activities like copper oxidase, histaminase, and ferrous oxidase.
- It is synthesized in the liver, where 6 to 8 atoms of copper, half as Cu+ and half as Cu++ ions, are attached to an apo-ceruloplasmin.
How will you discuss the pathophysiology of Ceruloplasmin?
- Ceruloplasmin is an alpha-2 globulin.
- The concentration at birth gradually increases to the adult level and continues to rise slowly with age.
- Adult females have higher levels than males.
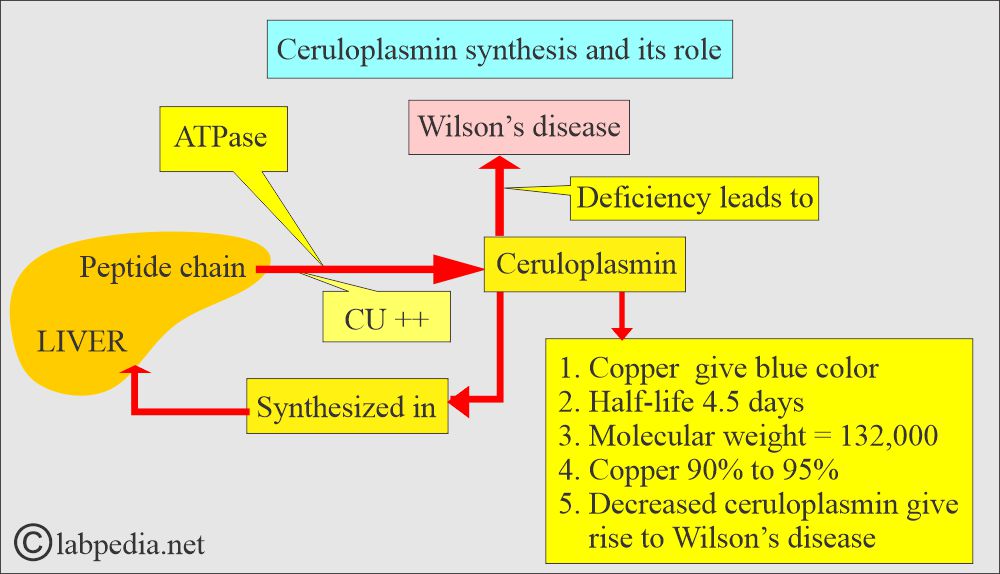
- Its half-life is 4.5 days, and its molecular weight is 132,000 daltons.
- It contains 90% to 95% of serum copper, giving it a blue color.
- In the case of increased Ceruloplasmin, the plasma has a greenish tint.
- Its primary role is oxidation and reduction in the plasma.
- Ceruloplasmin will bind copper for transport in the blood.
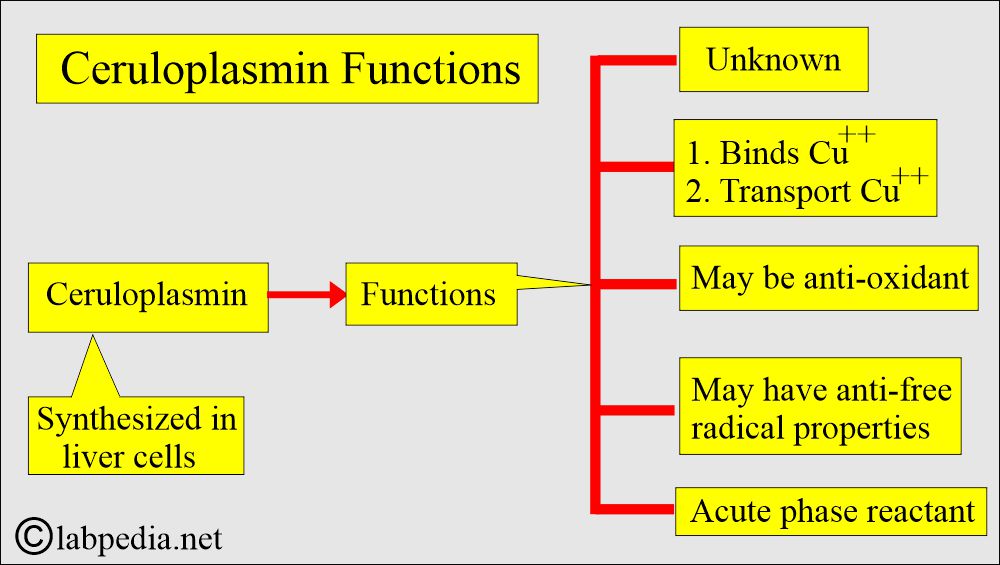
- Ceruloplasmin is synthesized in the liver.
- Wilson’s disease is an inherited disorder characterized by a decreased level of ceruloplasmin.
- In low Ceruloplasmin, increased unbound copper is toxic to tissues.
What are the functions of Ceruloplasmin?
- Ceruloplasmin’s physiological role is reduction and oxidation (Redox).
- This may be an oxidant or antioxidant, depending upon the factor, such as the presence of free Ferric (Fe+++) ions and ferritin-binding sites.
- Ceruloplasmin is essential for maintaining the ionic state of iron, specifically by oxidizing Fe++ to Fe+++ and preventing the formation of toxic iron compounds.
How will you discuss the Copper metabolism?
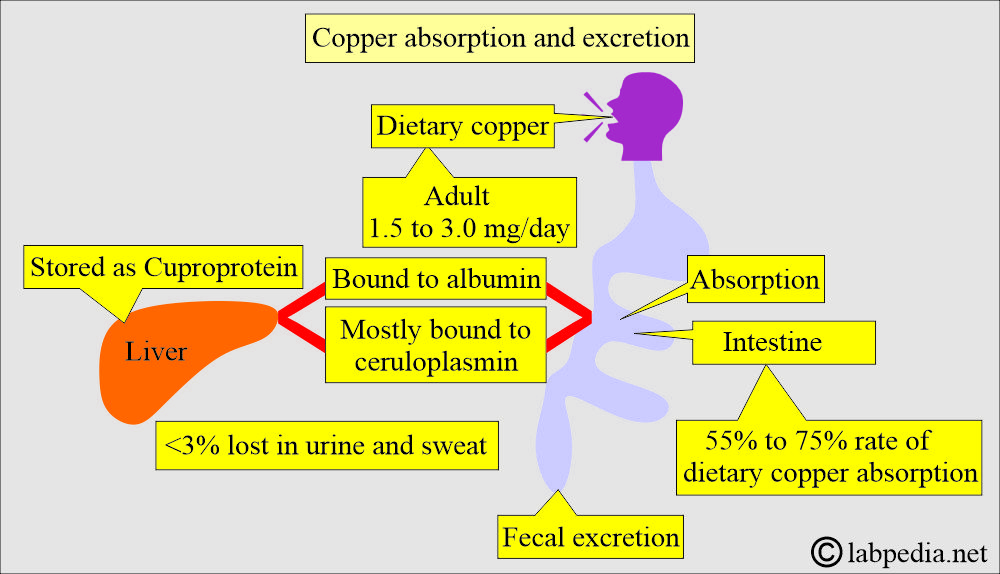
- Copper is absorbed from the gastrointestinal system in food.
- 1.5 to 3 mg/day of dietary copper is safe and adequate for the body.
- Excess copper is excreted into the bile by Ceruloplasmin, which is produced by the liver.
- In the case of a deficiency of Ceruloplasmin, copper accumulates in the body.
- Ceruloplasmin is a copper-containing protein that accounts for more than 95% of the copper found in the plasma.
- Copper is bound to Ceruloplasmin (α-2 globulin) with ferroxidase activity.
- Copper is also transported in plasma loosely bound to albumin.
- A small fraction of the copper is complexed with amino acids.
- Excretion of copper occurs mainly in the bile and a small fraction in the urine (<40 µg/day).
- Plasma copper is not a reliable indicator of blood copper level.
- Factors that will give a raised level of copper are:
- Oral contraceptives.
- Pregnancy.
- Inflammation or infectious process.
- Sources of copper:
- Liver.
- Kidneys.
- Eggs.
- Shellfish.
- Legumes.
Discuss the Copper absorption and excretion?
- The dietary copper requirement is 1.5 to 3.0 mg/day.
- It is absorbed in the intestine, and a small amount of blood binds to albumin and mostly to Ceruloplasmin.
- It is excreted in the feces.
- <3% is lost in the urine and copper.
What are the Copper functions?
- It is involved in the development of:
- Nerves.
- Bones. Copper maintains healthy bones. It prevents osteoporosis.
- Skin pigments.
- Collagen.
- It helps the immune system.
- It contributes to iron absorption.
- It prevents cardiovascular diseases.
- It prevents osteoporosis.
- Copper is a metal component of various enzymes:
- Cytochrome oxidase.
- Superoxide dismutase.
- Tyrosinase.
What are the sites where Copper can deposit?
- Eye.
- Liver.
- Brain.
- Kidneys.
- Hemolysis, necrosis, and other cellular changes may be caused by lipid peroxidation, a known toxic effect of copper.
- Copper is essential for the normal folding of the polypeptide chain.
What are the effects of Copper deficiency?
- Heart diseases.
- Bone and joint osteoarthritis,
- Osteoporosis.
- Demineralization is also associated with copper deficiency.
- Microcytic and hypochromic anemia.
- There is neutropenia.
- There may be hypothermia.
- There is hypercholesterolemia.
- There is decreased protection of the antioxidants.
- Copper deficiency is also associated with cerebellar and cerebral degeneration.
- There may be a subdural hematoma.
- There may be thrombosis of the arteries in the brain.
- Urinary copper excretion is increased.
What is the normal level of Ceruloplasmin?
Source 1
- Adult = 23 to 50 mg/dL (230 to 500 mg/L).
- Neonates = 2 to 13 mg/dL (20 to 130 mg/L).
- >7 years = 20 to 54 mg/dL
Source 2
| Age | Level mg/dL |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
- For conversion to SI unit x 10 = mg /L
- Copper serum = 70 to 140 µg/dL
- Urinary copper = 15 to 60 µg/24 hours (0.2 to 1.0 µmol/24 hours)
Wilson’s disease (Hepatolenticular degeneration):
How will you discuss the pathophysiology of Wilson’s disease?
- Wilson’s disease is a familial disorder of copper metabolism, and it is transmitted as an autosomal recessive trait.
- It is inherited as an autosomal recessive trait.
- This is also known as hepatolenticular degeneration and progressive lenticular degeneration.
- Worldwide, it is 1 in 30,000 people.
- Age: Most people diagnosed are between the ages of 5 to 35 years (another reference is 8 to 30 years) but may be seen in younger and older people (another source = This disease occurs from 6 to 40 years).
- The symptoms do not appear before the age of 6 years.
- This is a rare genetic disease with an accumulation of copper (copper toxicity).
- The patient inherits one defective gene from one of the parents.
- Excessive accumulation of copper in the liver, brain, kidneys, and cornea.
- There is a decrease in copper-containing Ceruloplasmin in the liver.
- There is an impairment of the excretion of copper from the liver.
- Copper begins to accumulate in the brain and liver.
- Ceruloplasmin level may be as low as <20 mg/dL. These levels are typically low at 10 mg/dL.
- Albumin-bound and free copper levels are increased, but total serum copper is low because of low Ceruloplasmin.
- It can be controlled if diagnosed before the deposition of copper in tissue.
- There is an accumulation of copper in the liver, kidney, brain, and cornea.
- Wilson’s disease is characterized by the inability of the liver to make a normal quantity of Ceruloplasmin.
- Ceruloplasmin is an α-2 globulin that transports copper.
What is the etiology of Wilson’s disease?
- The etiology is unknown; however, there is excessive deposition of copper in various tissues, which ultimately results in damage to the basal ganglia of the brain and liver tissue.
- Kidneys may also be affected, leading to the production of amino aciduria.
- Copper is also deposited in the cornea, producing a zone of discoloration called the Kayser-Fleischer ring.
What will be the clinical presentation of Wilson’s disease?
- The triad of the S/S and diagnostic of Wilson’s disease is:
- Typical basal ganglia symptoms.
- Kayser-Fleischer ring.
- Hepatic cirrhosis.
- The patient has symptoms of:
- About 30% to 50% of the patients develop liver symptoms.
- Approximately 30% to 40% of individuals develop neurological symptoms.
- About 20% to 30% develop psychiatric abnormalities like schizophrenia.
- Few patients develop Coombs-negative hemolytic anemia.
- Children are usually seen with liver symptoms. Mostly, there is chronic hepatitis.
- Macronodular cirrhosis develops later and is usually found in the late-age patient group.
- Some patients present with minimal active or inactive cirrhosis.
- Neurological symptoms start from the basal ganglia area (lentiform nucleus) of the brain, and they consist of:
- Varying degrees of incoordination.
- Tremors.
- Spasticity.
- Rigidity.
- Dysarthria (speech problems)
- There may be flapping tremors.
- There is fatigue, a lack of appetite, and abdominal pain.
- Hepatitis.
- Cirrhosis.
- Recurrent neuromuscular incoordination:
- Uncontrolled movements or muscle stiffness.
- Swallowing problems.
- Green-brown discoloration in the cornea due to the deposition of copper (Kayser-Fleischer rings).
- It is grossly visible but sometimes needs slit-lamp examination.
- Approximately 20% of patients may not exhibit Kayser-Fleischer rings at the time of diagnosis.
- Urinary copper excretion is increased.
- Early detection is the key to controlling the disease.
- Ceruloplasmin is an acute-phase protein that will be raised in infections, stress, and pregnancy.
How will you diagnose Wilson’s disease?
Clinical diagnostic features are:
- Kayser-Fleischer ring. It may be apparent to the naked eye or sometimes require a slit-lamp examination.
- Liver cirrhosis.
- Neurological features.
Laboratory findings:
- There is increased urinary excretion of copper, >40 µg/24 hours, and usually it is >100 µg/24 hours.
- Advise serum or plasma copper levels.
- Hepatic copper is raised >210 to 250 µg (dry liver).
- The total serum copper level is decreased, but the direct react fraction is elevated.
- Urinary excretion of copper is increased.
- Ceruloplasmin level. This is low, <20 mg/dL.
- <5 mg/dL is diagnostic.
- Hemolytic anemia is Coombs-negative.
- Measuring superoxide dismutase and cytochrome oxidase in platelets or leukocytes helps assess copper status.
How will you treat Wilson’s disease?
- This disease is treated with a copper chelating agent (penicillamine) or zinc acetate.
What are the complications of Wilson’s disease?
- Scarring of the liver (cirrhosis).
- Liver failure.
- Persistent neurological disease.
- Kidney diseases.
- Psychological problems.
- Blood problems like anemia and jaundice.
What are the causes of increased levels of Ceruloplasmin?
- Acute inflammatory diseases.
- Pregnancy.
- Thyrotoxicosis.
- Malignancies.
- Autoimmune diseases (Rheumatoid arthritis).
- Copper intoxication.
- Biliary Cirrhosis.
What are the causes of decreased levels of Ceruloplasmin?
- Wilson’s disease.
- In early infancy, the age before six months.
- Sprue.
- Kwashiorkor.
- Nephrotic syndrome.
- Starvation.
- The inherited defect of the production of alpha 2 globulin.
Questions and answers:
Question 1: What will be the finding in Wilson's disease in urine?
Question 2: How is Kayser-Fleischer ring seen in the eye?