Cerebrospinal Fluid Analysis:- Part 3 – CSF Culture, Special stains, and Electrophoresis, D/D of Meningitis
CSF Culture, Special stains
Sample for Cerebrospinal Fluid Analysis
- The analysis is done in the CSF fluid.
- CSF is collected in three tubes:
- The second tube is recommended for the culture, and the third tube for culture and special studies.
- Never use the first tube for the culture.
- Transport the CSF immediately to the lab; culture should be done as the sample reaches the lab.
Definition of Meningitis
- Meningitis is the inflammatory process involving protective layers surrounding the brain and spinal cord meninges.
- Symptoms include fever, stiff neck, severe headache, nausea, vomiting, and light sensitivity.
Cerebrospinal Fluid Analysis (CSF) for culture:
- The diagnosis of acute bacterial meningitis depends upon the organisms’ isolation.
- In infants under the age of 1 to 2 months, group B-streptococci are most common. This is followed by Escherichia coli.
- The third common organism is Listeria monocytogenes.
- The other organisms are Enteric gram-negative bacteria.
- For children from age 3 months to 5 or 6 years, the most common organism is H. influenzae.
- The second common organism is Meningococci.
- This is followed by the Pneumococci.
- For older children and adults, the most common is Meningococci.
- It is followed by Pneumococci.
- In Adults, the most common are Meninogococci and Pneumococci.
- In old people, pneumococci are more common than meningococci.
- These are followed by the gram-negative bacilli.
- Staphylococci are reported in 4% to 7% of the cases, and most are associated with brain surgery, septicemia, or endocarditis.
- The brain can be infected by any organism, even fungi.
Lab diagnosis of Cerebrospinal Fluid Analysis (CSF) causative organism:
- Gram stain.
- Acid-fast stain.
- Fluorescent antibody stain.
- India Ink preparation.
- Latex agglutination.
- Enzyme-linked immunoabsorbent assay (ELISA).
- The Limulus lysate test is useful to diagnose meningitis caused by gram-negative bacteria.
- Serologic tests are done to identify the microorganism.
- CSF serological tests can diagnose neurosyphilis.
Procedure to prepare the sediment for stains from Cerebrospinal Fluid (CSF):
- The most common stain used is the Gram stain.
- CSF can be centrifuged, and the sediment is stained for gram stains.
- Centrifuge CSF at 1500 g for 15 minutes, and prepare the slides from the sediments.
- Cytocentrifuge will provide a highly concentrated sample.
- Even with the concentrated CSF, 10% of the cases of gram stain and culture are negative.
- Take blood culture and CSF culture because causative bacteria will also be present in the blood.
- Screening of the gram stain of CSF is very difficult and may have false-negative results.
Gram stain of Cerebrospinal Fluid (CSF):
- It gives a preliminary diagnosis.
- Gram stain yield is 70% of the suspected cases.
- A negative gram stain does not rule out bacterial meningitis.
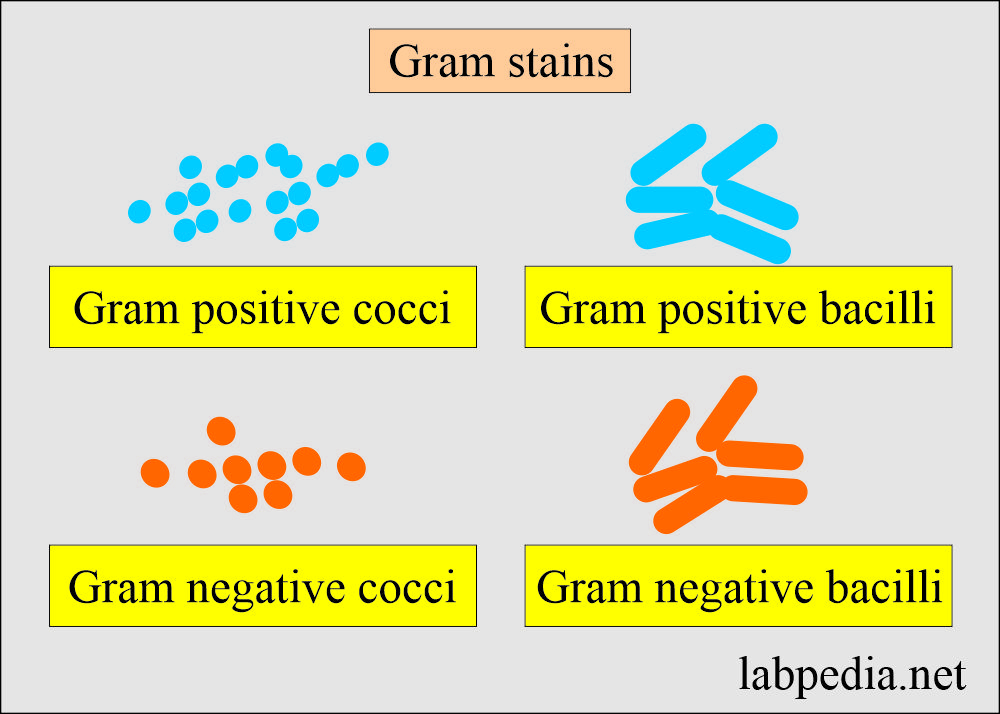
- Gram stain will differentiate:
- Bacterial meningitis with the presence of bacteria, whether it is cocci or bacilli, and as gram-positive or negative.
- Viral meningitis will be negative.
- The most common causative agents are H. Influenzae in children and Neisseria and Streptococcus in adults.
- The most common organisms are:
- Streptococcus pneumonia (gram-positive cocci).
- Hemophilus influenza (gram-negative rods, pleomorphic).
- Escherichia coli (gram-negative rods).
- Neisseria meningitidis (gram-negative cocci).
- Listeria monocytogenes (gram-positive rods, common in newborns).
- Streptococcus agalactiae (gram-positive cocci, common newborns).
- Tuberculous meningitis (advise Acid-fast stain or fluorescent antibody stain).
- The fungi are gram stain positive or advise India Ink preparation.
Culture and Sensitivity of Cerebrospinal Fluid Analysis:
- Culture can identify the organism, and the most common organisms found are:
- Bacteria.
- Fungi.
- T.Bacilli.
- Culture needs 24 to 48 hours to get a result. This may take up to 72 hours to get sensitivity.
- Culture can recognize around 85% of the bacteria in case of suspected bacterial meningitis.
- Meningococci grow best in a high CO2 atmosphere.
Identification of Tuberculous bacilli in Cerebrospinal Fluid Analysis (CSF):
- CSF and sputum smears are stained for the Acid-fast bacilli.
- These are red, rod-shaped bacteria.
- The conventional culture of the T bacilli takes 4 to 6 weeks of incubation.
- BACTEC method is a culture technique in which the growth medium for the culture of M. tuberculosis has added a substrate labeled with radioactive carbon. (14C).
- This substrate is used by the bacteria and produces radioactive carbon dioxide (14CO2), from the substrate.
- This 14CO2 is detected and quantitated.
- This will give quick identification of mycobacteria.
- The polymerase chain reaction (PCR) method is also developed.
- This allows the amplification of genomes, which can be detected by the genetic DNA probe.
- Mycobacterium is detected in 36 to 48 hours.
Cerebrospinal Fluid Analysis (CSF) protein electrophoresis
Indication for CSF electrophoresis:
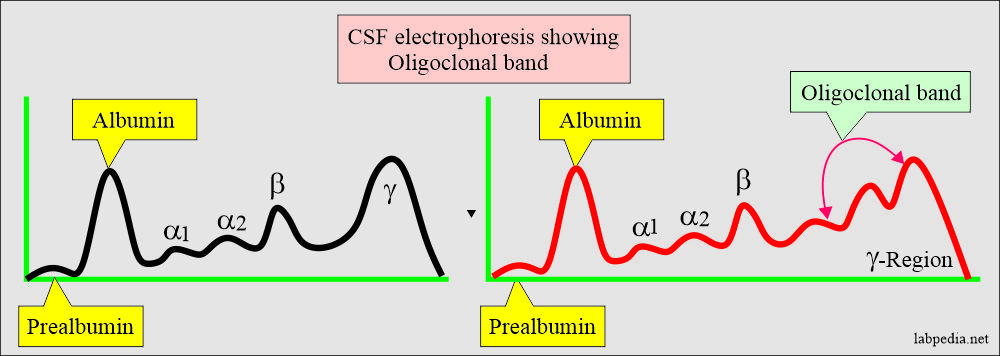
- Electrophoresis is done to find any abnormality of the proteins and immunoglobulins.
- This helps diagnose:
- Multiple sclerosis.
- Neurosyphilis.
- Autoimmune diseases.
Multiple sclerosis (MS) finding in Cerebrospinal Fluid Analysis:
- It is a chronic demyelinating disease characterized by relapses, remitting course with the central nervous system episodes separated in time and anatomic location.
- Recurrent illness of unpredictable length and severity of the disease.
- A multifocal demyelinating process in the cerebral hemisphere.
- The involvement of white matter results in various combinations of weakness, ataxia, vision problems, and paresthesias and frequently ends in paralysis.
- In Multiple sclerosis, typical findings are:
- In the early stages, routine CSF examination changes are nonspecific.
- Later on, changes are similar to aseptic meningitis.
- Increased total proteins and this is mainly gamma globulin.
- There is increased IgG production.
- There is an increased IgG in 60% to 80% of the cases.
- Increased IgG: albumin ratio.
- The normal ratio is <25%.
- Around 70% of MS patients have raised IgG/albumin ratio.
- This IgG/albumin ratio is more specific than only IgG.
- The gamma region has a discrete sharp band called the oligoclonal band.
- The presence of the oligoclonal band is an important lab. finding.
- Without an oligoclonal band, if IgG is raised, it has no significance.
- Total proteins are mildly elevated in 25% to 50% of the cases.
- If the total protein is >100 mg/dL, then the diagnosis of MS is less likely.
- The oligoclonal band may be seen in HIV.
- Electrophoresis differentiates CSF from serum, where there is an extra band of transferrin in CSF and not in the serum.
Differential diagnosis of meningitis:
| Disease | Pressure | Gross | Glucose mg/dL | Protein mg/dL | TLC count/cmm | Type of Cells |
|---|---|---|---|---|---|---|
| Normal | 70-200 | Clear(C.L) | 45-85 | 10-45 | 0-8 | MN |
| Bact. Meningitis | Increased | Turbid | 0-25 mg/dL | 50-500 | 1000-2000+ | Polys |
| Viral meningitis | Normal | <100 mg/dL | 5 to 300 | Lymphocytes | ||
| Tub. Meningitis | Increased | clear/cobweb | 15-45 (Decreased) | 50-100 | 100-300 | Lympho |
| Fungal meningitis | Increased | Normal to Decreased | 50 to 300 | 40 to 400 | Lymph0 + monocytes | |
| Poliomyelitis | Increased | clear | normal | 50-200 | 50-250 | poly/lympho |
| Subarachnoid Hemorrhage | increased | bloody | normal | 50-100 | normal | RBCs |
MN = Mononuclear cells.
TLC = Total leucocytic count.
Mening. = Meningitis.
Lympho = Lymphocytes.
Haem = Haemorrhage.
Differential diagnosis of various types of meningitis:
| Type of CSF | Appearance | Glucose | Protein | WBCs/cmm | Serology/other tests |
|
|
|
|
|
|
|
Usually clear | Normal | Normal or increased | 10 to 1000, mostly lymphocytes |
|
|
|
Mostly 0 to 45 mg/dL |
|
|
|
|
|
|
|
|
|
|
|
Normal | 20 to 200 mg/dL |
|
|
|
Normal | Normal | 50 to 100 mg/dL | <300/cmm |
|
|
Normal | Normal then decreases | Increased |
|
|
|
Normal |
|
|
|
|
|
Xanthochromasia | Normal | <2000 mg/dL |
|
|
|
|
Normal | 20 to 125 mg/dL | 0 to >2000/cmm |
|
|
|
Normal | Slightly increased | <500/cmm | Serology = positive |
|
Normal | Normal | Increased |
|
|
|
Normal | Normal | Always >50/cmm | Oligoclonal band = Positive | |
|
Normal | Increased | Normal | Mostly normal | CSF glucose = Increased |
Questions and answers:
Question 1: How you can confirm the diagnosis of multiple sclerosis?
Question 2: What you will see in subarachnoid hemorrhage in CSF?