Cerebrospinal Fluid Analysis:- Part 3 – CSF Culture, Special stains, and Electrophoresis, D/D of Meningitis
CSF Culture, and Special stains
What sample is needed for Cerebrospinal Fluid Analysis?
- The analysis is done in the CSF fluid.
- CSF is collected in three tubes:
- The second tube is recommended for culture, and the third tube is recommended for both culture and special studies.
- Never use the first tube for the culture.
- Transport the CSF immediately to the laboratory; culture should be performed as soon as the sample arrives at the lab.
How will you define Meningitis?
- Meningitis is the inflammatory process involving the protective layers surrounding the brain and spinal cord, the meninges.
- Symptoms include fever, stiff neck, severe headache, nausea, vomiting, and sensitivity to light.
How will you perform the Cerebrospinal Fluid (CSF) culture?
- The diagnosis of acute bacterial meningitis depends on the isolation of the organism.
- In infants under the age of 1 to 2 months, group B-streptococci are most common. This is followed by Escherichia coli.
- The third common organism is Listeria monocytogenes.
- The other organisms are Enteric gram-negative bacteria.
- For children from age 3 months to 5 or 6 years, the most common organism is H. influenzae.
- The second common organism is Meningococci.
- This is followed by the Pneumococci.
- For older children and adults, the most common is Meningococci.
- It is followed by Pneumococci.
- In Adults, the most common are Meninogococci and Pneumococci.
- In old people, pneumococci are more common than meningococci.
- The gram-negative bacilli follow these.
- Staphylococci are reported in 4% to 7% of the cases, and most are associated with brain surgery, septicemia, or endocarditis.
- Any organism, even fungi, can infect the brain.
How will you find the organism in the Cerebrospinal Fluid?
- Gram stain.
- Acid-fast stain.
- Fluorescent antibody stain.
- India Ink preparation.
- Latex agglutination.
- Enzyme-linked immunoabsorbent assay (ELISA).
- The Limulus lysate test is useful for diagnosing meningitis caused by Gram-negative bacteria.
- Serologic tests are done to identify the microorganism.
- CSF serological tests can diagnose neurosyphilis.
How will you prepare the sediment for stains from Cerebrospinal Fluid (CSF)?
- CSF can be centrifuged, and the sediment is stained for Gram stain
- Centrifuge CSF at 1500 g for 15 minutes, and prepare the slides from the sediments.
- The cytocentrifuge will provide a highly concentrated sample.
- The most common stain used is the Gram stain..
- Even with the concentrated CSF, 10% of the cases of Gram stain and culture are negative.
- Take blood culture and CSF culture because causative bacteria will also be present in the blood.
- Screening of the Gram stain of CSF is very difficult and may have false-negative results.
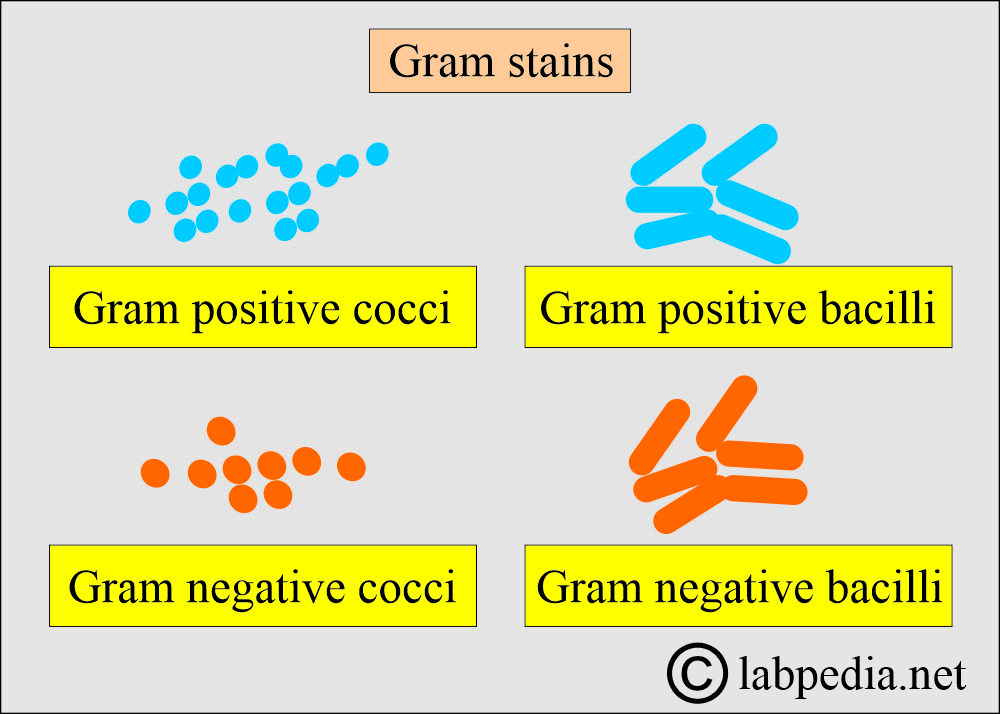
What do you know about the Gram stain of Cerebrospinal Fluid (CSF)?
- It gives a preliminary diagnosis.
- Gram stain yield is 70% of the suspected cases.
- A negative Gram stain does not rule out bacterial meningitis.
- Gram stain will differentiate:
- Bacterial meningitis is characterized by the presence of bacteria, whether they are cocci or bacilli, and whether they are gram-positive or gram-negative.
- Viral meningitis will be negative.
- The most common causative agents are H. Influenzae in children and Neisseria and Streptococcus in adults.
- The most common organisms are:
- Streptococcus pneumonia (gram-positive cocci).
- Hemophilus influenza (gram-negative rods, pleomorphic).
- Escherichia coli (gram-negative rods).
- Neisseria meningitidis (gram-negative cocci).
- Listeria monocytogenes (gram-positive rods, common in newborns).
- Streptococcus agalactiae (gram-positive cocci, common in newborns).
- Tuberculous meningitis (advise Acid-fast stain or fluorescent antibody stain).
- The fungi are Gram-stain positive or require India Ink preparation.
How will you interpret the culture and Sensitivity of Cerebrospinal Fluid?
- Culture can identify the organism, and the most common organisms found are:
- Bacteria.
- Fungi.
- T.Bacilli.
- Culture needs 24 to 48 hours to get a result. This may take up to 72 hours to get sensitivity.
- Culture can identify around 85% of the bacteria in cases of suspected bacterial meningitis.
- Meningococci grow best in a high CO2 atmosphere.
- TB culture needs 4 to 6 weeks.
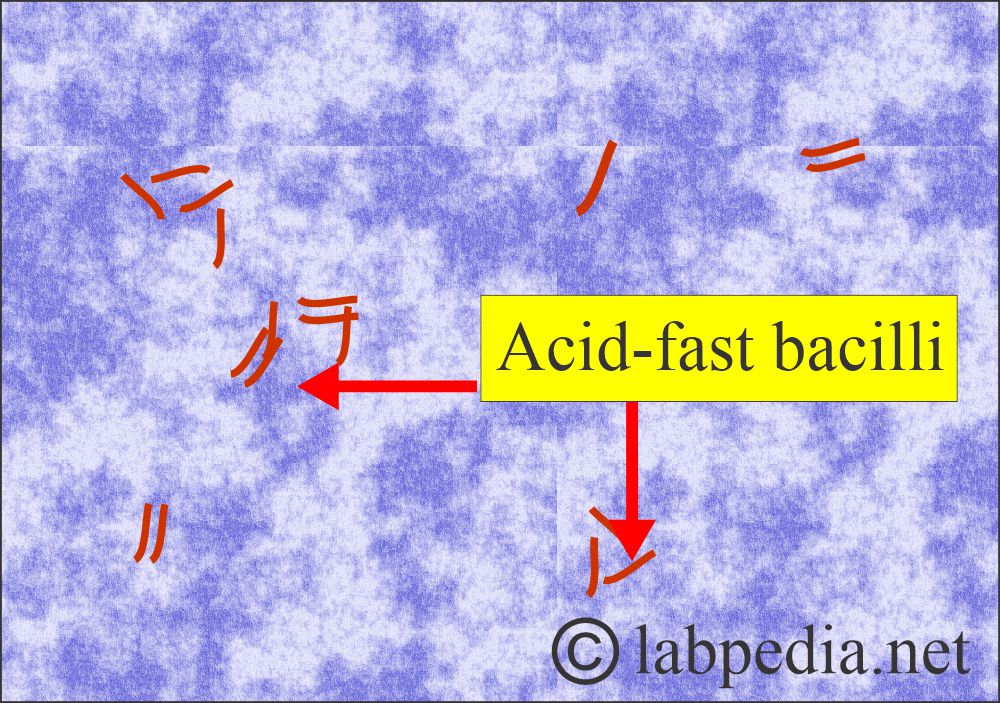
How will you identify Tuberculous bacilli in Cerebrospinal Fluid?
- CSF and sputum smears are stained for Acid-fast bacilli.
- These are red, rod-shaped bacteria.
- The conventional culture of T. bacilli requires 4 to 6 weeks of incubation.
- The BACTEC method is a culture technique in which the growth medium for culturing M. tuberculosis contains a substrate labeled with radioactive carbon. (14C).
- The bacteria utilize this substrate and produce radioactive carbon dioxide (14CO2) from it.
- This 14CO2 is detected and quantified.
- This will give quick identification of mycobacteria.
- The polymerase chain reaction (PCR) method has also been developed.
- This allows the amplification of genomes, which the genetic DNA probe can detect.
- Mycobacterium is detected in 36 to 48 hours.
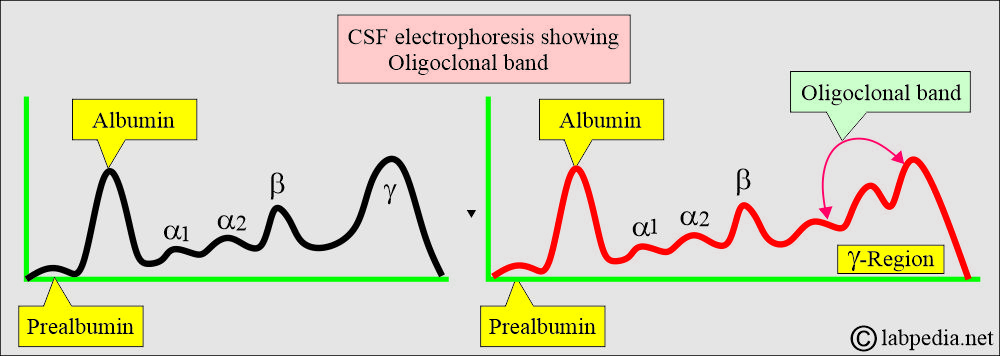
How will you perform the Cerebrospinal Fluid (CSF) protein electrophoresis?
What are the indications for CSF electrophoresis?
- Electrophoresis is used to detect any abnormalities in proteins and immunoglobulins.
- This helps to diagnose:
- Multiple sclerosis.
- Neurosyphilis.
- Autoimmune diseases.
What will you see in Multiple Sclerosis (MS) in Cerebrospinal Fluid?
- It is a chronic demyelinating disease characterized by relapses, a remitting course, and episodes separated in time and anatomic location within the central nervous system.
- Recurrent illness of unpredictable length and severity.
- A multifocal demyelinating process in the cerebral hemisphere.
- The involvement of white matter results in various combinations of weakness, ataxia, vision problems, and paresthesia and frequently ends in paralysis.
- In Multiple sclerosis, typical findings are:
- In the early stages, routine CSF examination changes are nonspecific.
- Later on, changes are similar to aseptic meningitis.
- Increased total proteins, and this is mainly gamma globulin.
- There is increased IgG production.
- There is an increased IgG in 60% to 80% of the cases.
- Increased IgG: albumin ratio:
- The normal ratio is <25%.
- Approximately 70% of MS patients have an elevated IgG/albumin ratio.
- This IgG/albumin ratio is more specific than the IgG alone.
- The gamma region has a discrete, sharp band called the oligoclonal band.
- The presence of an oligoclonal band is a significant laboratory finding.
- Without an oligoclonal band, if IgG is raised, it has no significance.
- Total protein levels are mildly elevated in 25% to 50% of cases.
- If the total protein level is greater than 100 mg/dL, the diagnosis of MS is less likely.
- The oligoclonal band may be seen in HIV.
- Electrophoresis differentiates CSF from serum, as there is an additional band of transferrin in CSF that is not present in serum.
How will you summarize various types of meningitis?
| Disease | Pressure | Gross | Glucose mg/dL | Protein mg/dL | TLC count/cmm | Type of Cells |
|---|---|---|---|---|---|---|
|
70-200 | Clear(C.L) | 45 to 85 | 10 to 45 | 0 to 8 | MN |
|
Increased | Turbid | 0 to 25 mg/dL | 50 to 500 | 1000 to 2000+ | Polys |
|
Normal | <100 mg/dL | 5 to 300 | Lymphocytes | ||
|
Increased | clear/cobweb | 15 to 45 (Decreased) | 50 to 100 | 100 to 300 | Lympho |
|
Increased | Normal to Decreased | 50 to 300 | 40 to 400 | Lymph0 + monocytes | |
|
Increased | clear | Normal | 50 to 200 | 50 to 250 | poly/lympho |
|
Increased | bloody | Normal | 50 to 100 | normal | RBCs |
MN = Mononuclear cells.
TLC = Total leucocytic count.
Mening. = Meningitis.
Lympho = Lymphocytes.
Haem = Haemorrhage.
How will you differentiate various types of meningitis?
| Type of CSF | Appearance | Glucose | Protein | WBCs/cmm | Serology/other tests |
|
|
|
|
|
|
|
|
|
Normal or increased | 10 to 1000, mostly lymphocytes |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Normal |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Serology = positive |
|
|
|
|
|
|
|
|
|
|
Oligoclonal band = Positive | |
|
|
|
|
|
CSF glucose = Increased |
Questions and answers:
Question 1: How can you confirm the diagnosis of multiple sclerosis?
Question 2: What will you see in subarachnoid hemorrhage in CSF?