Candidiasis, Candida albicans and Diagnosis
Candida albicans
How will you take a sample for Candida albicans?
- Scrapings from the affected area.
- Gram stain of the smear.
- The culture of the material.
- The patient’s serum is needed for an antibody test.
- The serum or body fluid is needed for the presence of the antigens.
How will you define Candida albicans?
- Candida organisms may be present as normal flora of the nasopharyngeal area or gastrointestinal tract (20% to 40%).
- Positive culture of the vaginal secretions in asymptomatic women (10% to 15%)
- Superficial infection is seen in the oral cavity or vagina.
- It can be seen as a deep or disseminated infection.
- The most common opportunistic infections are caused by:
- Candida.
- Aspergillosis.
- Mucormycosis.
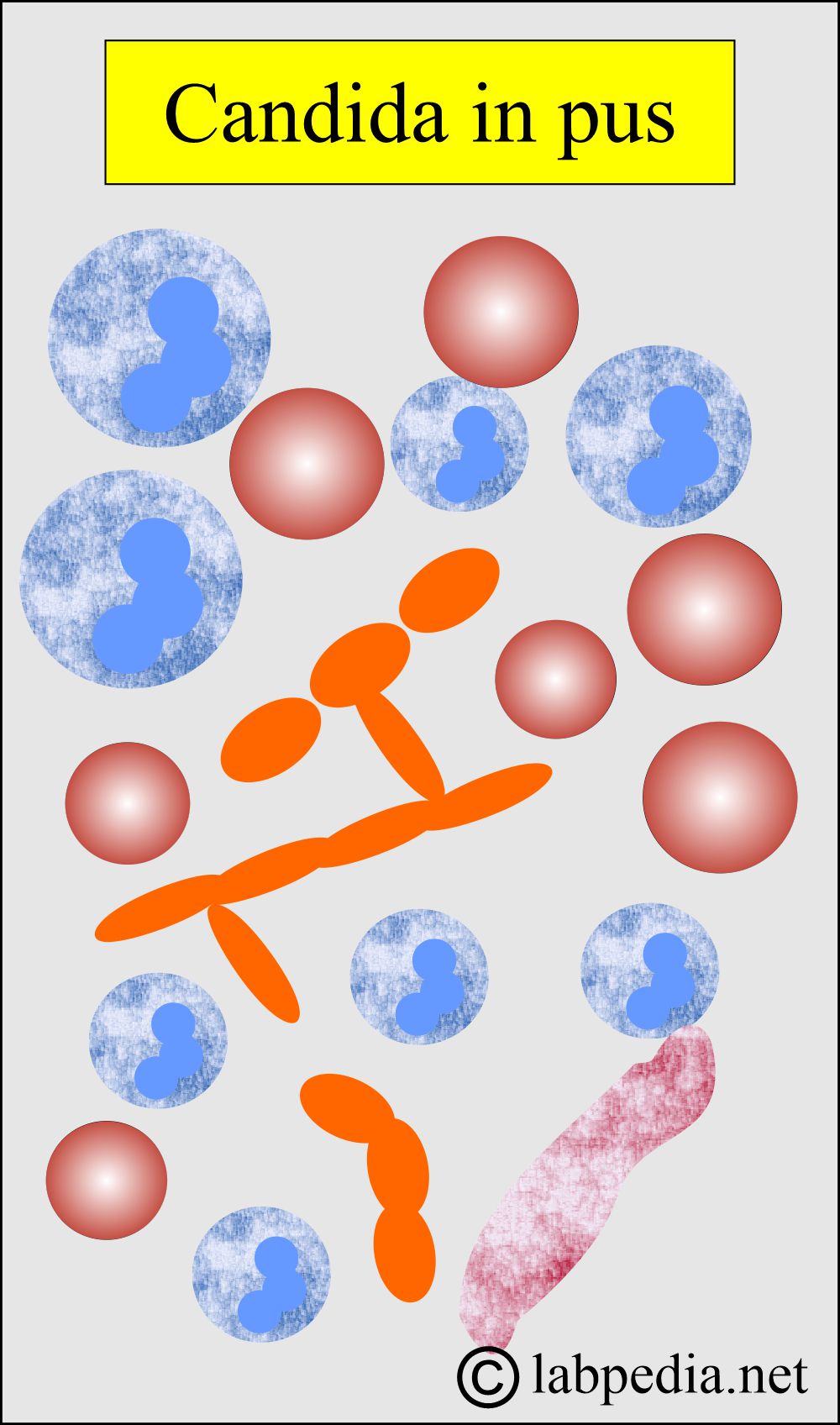
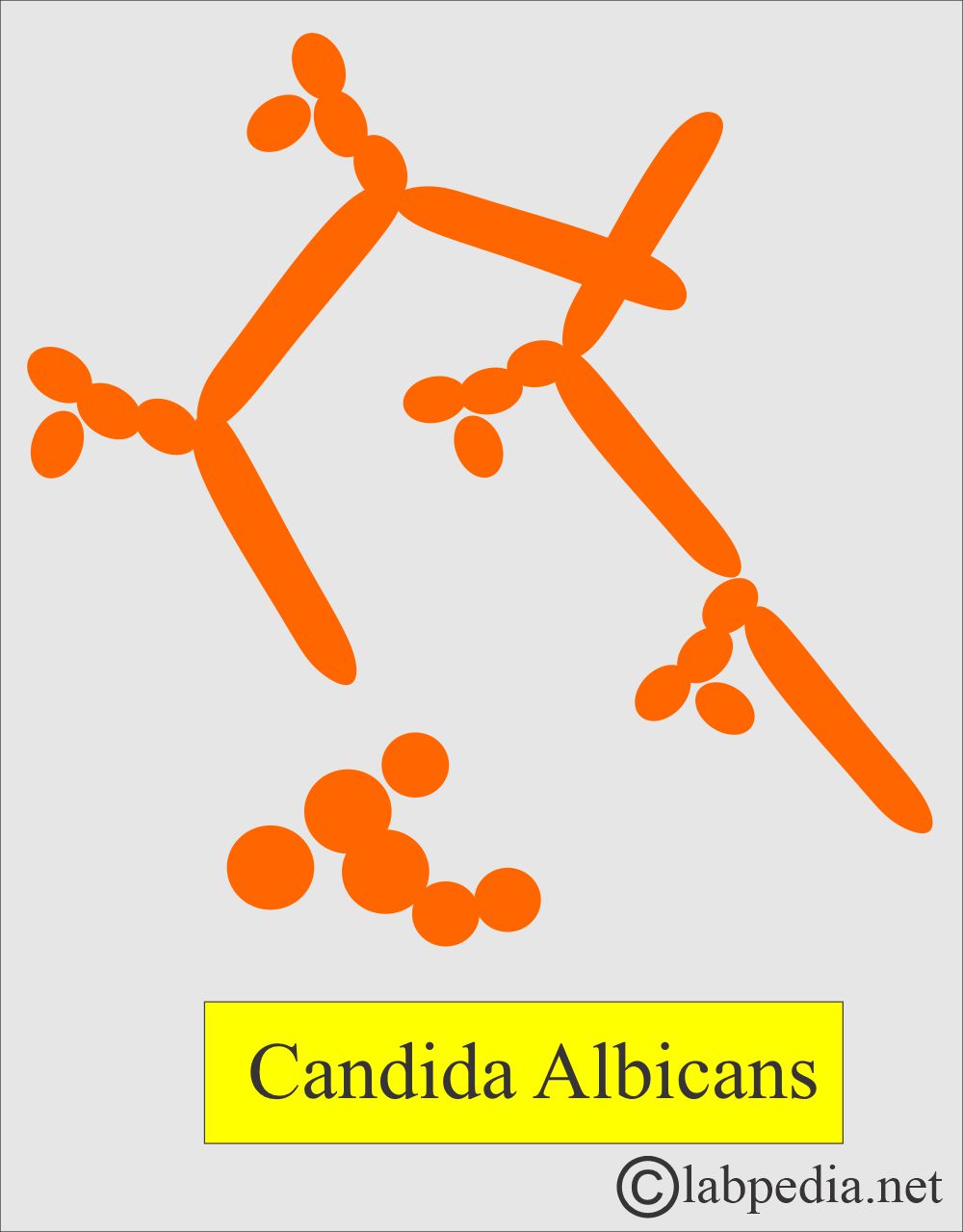
How will you discuss the microbiology of Candida albicans?
- The most common Candida infection in humans is caused by Candida albicans (90%), followed by Candida tropicalis.
- These are oval budding yeast measuring 3 x 6 μm.
- These are gram-positive.
- Elongated filament cells joined end to end are called pseudohyphae in vivo.
- Candida albicans is the only species to produce hyphae and pseudohyphae in vivo.
- Spherical to budding oval cells (3 to 5 x 5 to 10 μm).
- Yeast is Y-form.
- Other types are:
- C. stellatoidea (subtype is C.albicans).
- C. tropicalis.
- C. krusei.
- C. guilliermondii.
- C. parapsilosis.
- Candida is also known as moniliasis.
What are the characteristic features of Candida albicans?
- Candida is a normal flora of the upper respiratory tract (nasopharyngeal area), gastrointestinal tract, and female genital tract (20% to 40%).
How will you culture Candida albicans?
- These are aerobic and easy to cultivate.
- Sabouraud’s medium may be made selective by adding the antibiotic (chloramphenicol) and is helpful for primary isolation when incubated at 37 °C for 48 hours.
- Other media, such as blood agar, show colonies around the antibiotic disc, indicating that bacterial growth has been inhibited.
- Colonies are cream to white, flat or hemispherical, and have a waxy appearance.
What is the pathogenicity of Candida albicans?
- The most common areas affected are:
- Mucous membranes.
- Nails.
- Skin.
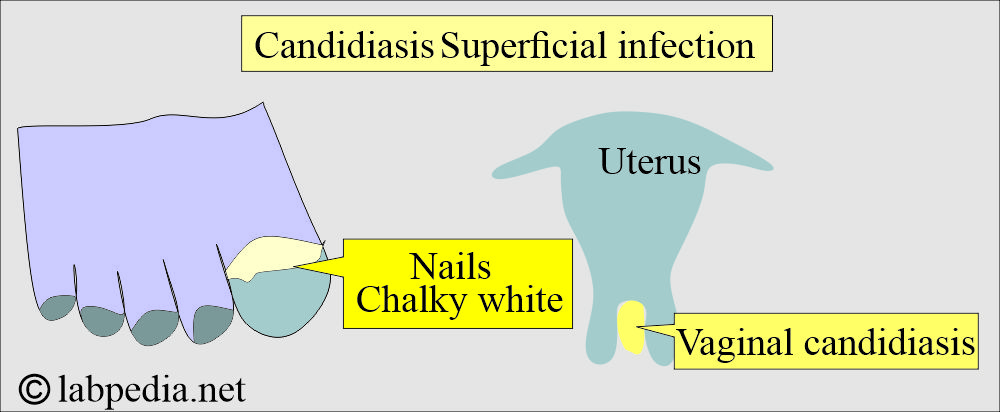
- Candidiasis may be Superficial, where it involves:
- Mucocutaneous thrush.
- Skin in the form of red weeping areas, particularly in obese people.
- In chronic mucocutaneous lesions, involvement is typically seen in the face and scalp.
- Candidiasis may be deep, where it involves:
- Lower respiratory system.
- Urinary tract.
- The eyes, meninges, bones, and kidneys are involved in septicemia.
- It is a yeast-like fungus and is usually present in vaginal secretions.
- Candida albicans is present in the upper respiratory, female genital tract, and gastrointestinal tract.
- Candida albicans is the causative agent in 90% of the cases.
- The rapid growth of Candida occurs in:
- The patients are on long-term antibiotic therapy.
- The patients with diabetes mellitus.
- The patients are on corticosteroid therapy.
- The female during pregnancy.
- The ladies on oral contraceptives.
- Candida growth occurs in areas that are not well-ventilated, such as undergarments, and in infants, particularly in the diaper area.
- Candida infection has occurred in immune-compromised patients mainly due to T-lymphocyte depression and AIDS.
- It may be seen in premature babies.
- It is identified in malignancies like leukemia and lymphoma.
- It is seen in extensive surgery.
What are the clinical manifestations of Candida albicans?
- The predisposing factors are:
- Aged.
- Cachectic or debilitated persons.
- People with diseases like AIDS or leukemia.
- Drugs are impairing the immune system.
- Oral antibiotic therapy.
- Clinically, there may be mucosal candida infection characterized by laryngitis and esophagitis.
- Female Patients may have vaginitis, cystitis, and thrush.
- In the case of acute disease, it may involve the eyes, skin, and muscles when it spreads through the blood.
- Chronic cases have been seen in a patient with neutropenia.
- Clinically, one can see candidiasis as follows:
- Thrush.
- Diaper rash.
- Genital candidiasis.
- Candida albicans lesions are:
- Superficial like thrush.
- The skin shows a red, weeping lesion.
- Chronic mucocutaneous candidiasis affects the face and scalp.
- Deep lesions are involved in both the respiratory and urinary systems.
- Septicemia shows eye, endocardium, meninges, kidneys, and bone lesions.
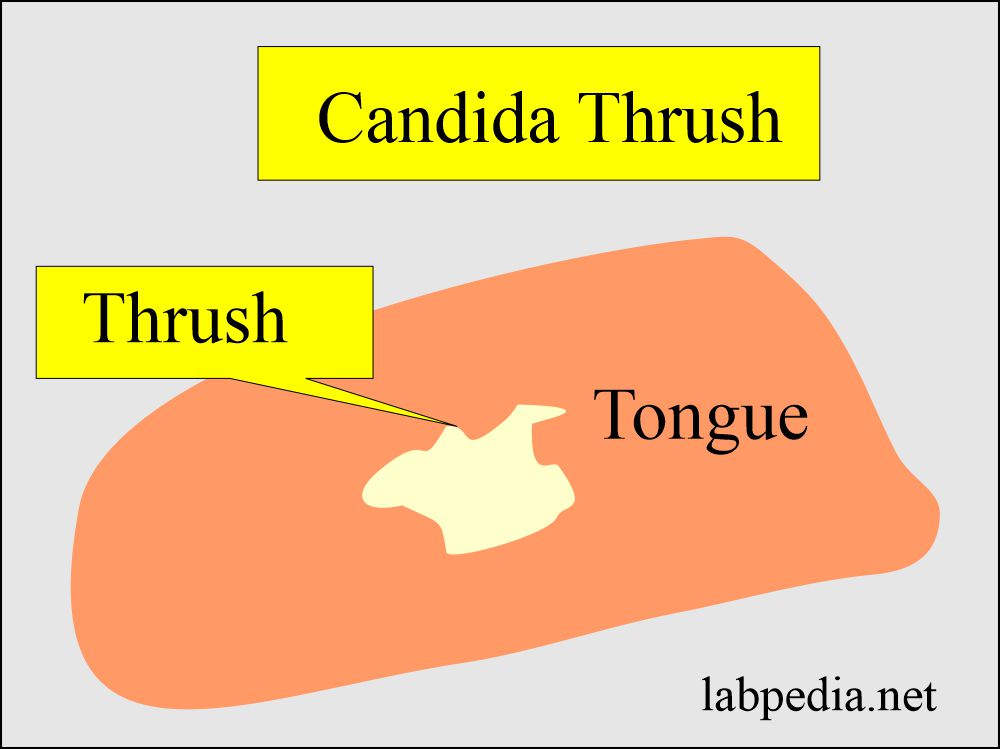
Thrush:
- This condition is a very common finding.
- It is oropharyngeal candidiasis.
- There are white or yellow patches on the tongue or oral cavity with a reddish base covering the mucous membranes.
- There is a red area that may involve the throat.
- It is difficult to scrape off.
Diaper rash:
- It is seen in infants.
- It occurs when a wet diaper is left for an extended period.
- It is seen in the warm, moist areas under diapers and in adults between skin folds (under the breast in females).
Genitalcandidiasis:
- It is more common in females than in men. It involves the vagina (monilia).
- In females, it leads to candida vaginitis and is common during:
- Antibiotic therapy.
- Oral contraceptives.
- During menses.
- During pregnancy.
What are the S/S of vaginitis?
- There is severe itching in the vagina.
- There is vaginal discharge, thick, copious secretion, wetting the undergarments.
- On examination, the vagina is inflamed.
- Cottage cheese patches appear in white clumps attached to the vaginal wall.
- Imidazole suppository helps to treat the disease.
How will you discuss the Invasive candidiasis?
- It occurs through the I/V or catheter when it is left in the body.
- It can enter the brain, heart, and eyes.
- It may involve nails and look like onychomycosis.
- Candida albicans and Candida tropicalis are also seen in conditions like:
- Bone marrow transplantation.
- Leukemias.
- Lymphomas.
What is the mode of the spread of Candida albicans?
- It is usually endogenous, but cross-infection may occur, such as from a mother to a baby or a baby in the nursery.
- Infections are more common in premature babies.
- Infection is also more common in debilitated patients and patients with diabetes mellitus.
- Infection is more common in immunocompromised patients with AIDS, malignancy, leukemia, and lymphoma.
- It is commonly observed in patients undergoing long-term treatment with antibiotics, immunosuppressive drugs, or cytotoxic agents.
How will you diagnose Candida albicans?
- Wet film from the affected area can be Gram-stained.
- Culture is diagnostic, and the culture media used are:
- Sabouraud’s medium.
- Incubation is done at 37 °C for 48 hours.
- Agar and blood agar.
- An indirect hemagglutination test may be helpful, but these tests lack sensitivity and specificity.
- Antigen tests like EIA are available.
- A titer greater than 1:8 indicates systemic infection.
- A positive test may be observed in mucocutaneous candidiasis or in severe vaginal infections.
- The skin test based on type VI sensitivity is a good diagnostic indicator.
- Scrapings with KOH preparation may show Candida.
- It will detect around 60% to 70%of vaginal secretion smears.
What are the diagnostic features of Candida albicans?
- Germ tubes are observed when grown in serum for 3 hours at 37 °C and then made into a wet film.
- There are filamentous outgrowths, such as germ tubes.
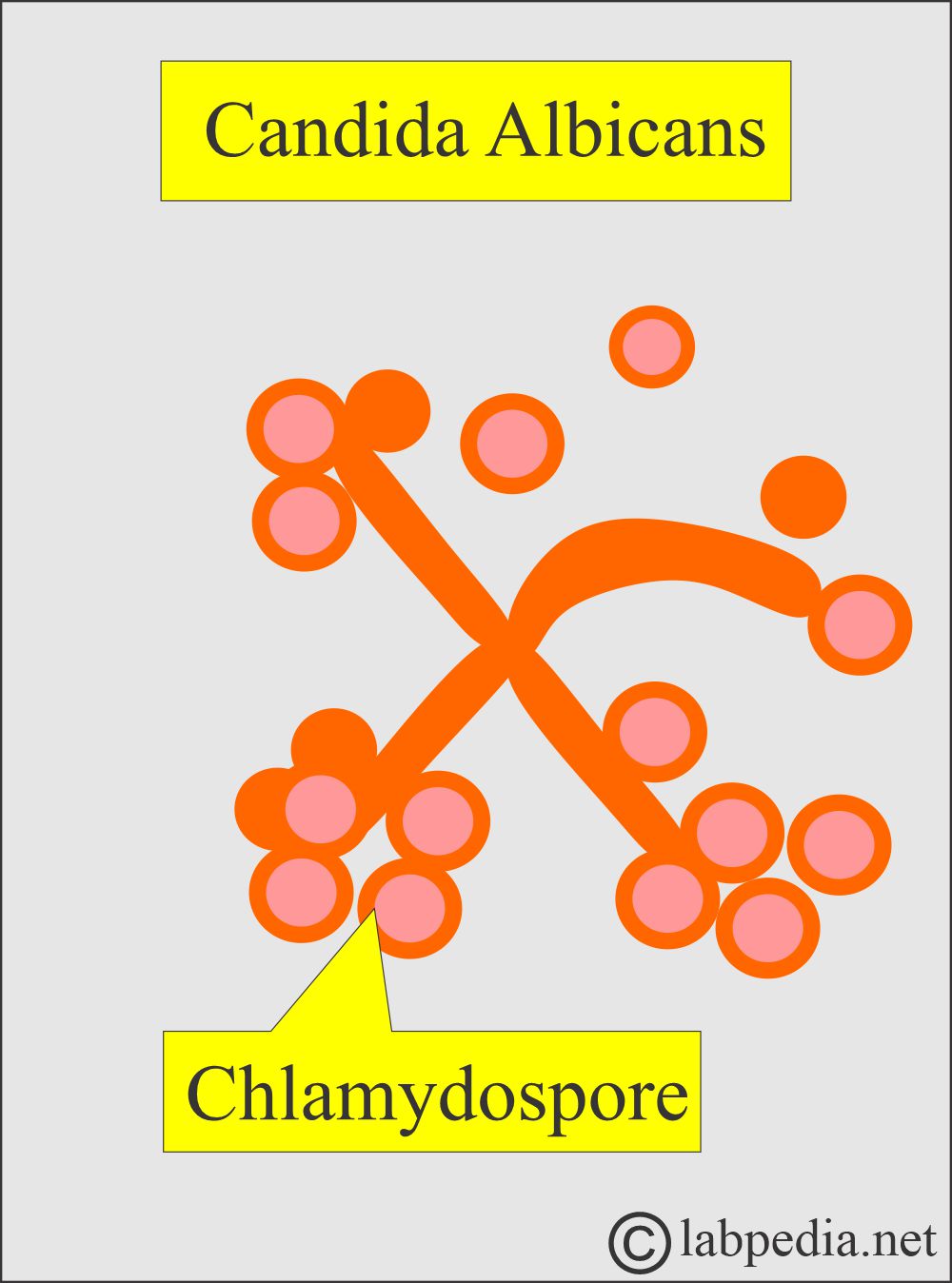
- Chlamydospores are seen when grown on a nutrient-poor medium (cornmeal agar) for 24 hours at 28 °C.
- There are round, thick-walled resting structures – chlamydospores, usually found at the ends of pseudohyphae deep in the agar.
- Biochemical activity is a result of fermentation.
- Antigenic structure: This falls into two groups:
- Serotype A.
- Serotype B.
- Antibodies are detected in most of the human sera.
- A positive skin test is common due to a delayed hypersensitivity (type IV) reaction. This is almost universal in normal adults.
- How will you summarize the diagnosis of Candida infection?
- Wet-mount or stained slide preparation.
- KOH (potassium hydroxide) can diagnose in 60% to 70% of the cases.
- The use of fluorescent stain (Calcofluor white) increases the detection possibility.
- Papanicolaou-stained slides are positive in 45% to 50% of the cases.
- Culture.
- The isolation of Candida from blood and urine is suggestive of disseminated candidiasis.
- Serologic tests.
- Latex agglutination tests are available. These are easy to perform.
- IgG EIA procedure is positive in about 82% of the cases for sensitivity.
How will you treat Candida infection?
- Candida is resistant to all antibacterial drugs because it is an eukaryotic microorganism.
- Amphotericin B is the drug of choice.
- For topical use, Imidazole (miconazole, clotrimazole) can be used.
- Thrush is treated with nystatin, amphotericin B, and miconazole.
- Systemic lesion needs I/V amphotericin B, either given alone or with 5-fluorocytosine.
Questions and answers:
Question 1: How will you make the Candida wet slide method?
Question 2: What is thrush?