Blood Urea Nitrogen (BUN), and Interpretations
Blood Urea Nitrogen (BUN)
What sample is needed for Blood Urea Nitrogen (BUN)?
- It is performed on the patient’s serum.
- No special preparation is needed.
- This test can be done on a random sample.
What are the indications for blood urea nitrogen (BUN)?
- To assess renal function.
- As a routine test for a patient with dialysis.
- To assess liver function.
- This may be part of the routine test.
- In patients:
- Has nonspecific symptoms.
- During the hospital stay.
- Before some drug therapy.
- Acutely ill patients are admitted to the emergency department.
- BUN is an unreliable and less specific indicator of the kidneys’ function.
What are the precautions for Blood Urea Nitrogen (BUN)?
- If there is Fluoride, that will inhibit the Urease reaction.
- Avoid hemolysis.
- Protein intake will affect BUN. A low-protein diet will result in a low BUN.
- A high-protein diet or the use of nasogastric tubing can increase BUN.
- Remember that muscle mass is higher in males than in females and in children.
- Overhydrated patients will dilute the BUN, resulting in a lower value.
- The dehydrated patient will have concentrated BUN and give a high value.
- GI bleeding can cause an increase in BUN levels.
- Advanced pregnancy may increase the BUN level.
- Drugs increasing the BUN level are cephalosporin, indomethacin, gentamicin, polymyxin B, rifampicin, bacitracin, neomycin, tetracycline, thiazide diuretics, and aspirin.
- Some drugs that decrease the BUN level are streptomycin and chloramphenicol.
How will you define Blood urea nitrogen (BUN)?
- It is the nitrogen part of the urea.
- BUN measures the nitrogen part of the urea.
- Urea nitrogen is synthesized mainly in the liver. It is mostly the end product of protein metabolism.
- Urea in the blood is reported as blood urea nitrogen (BUN).
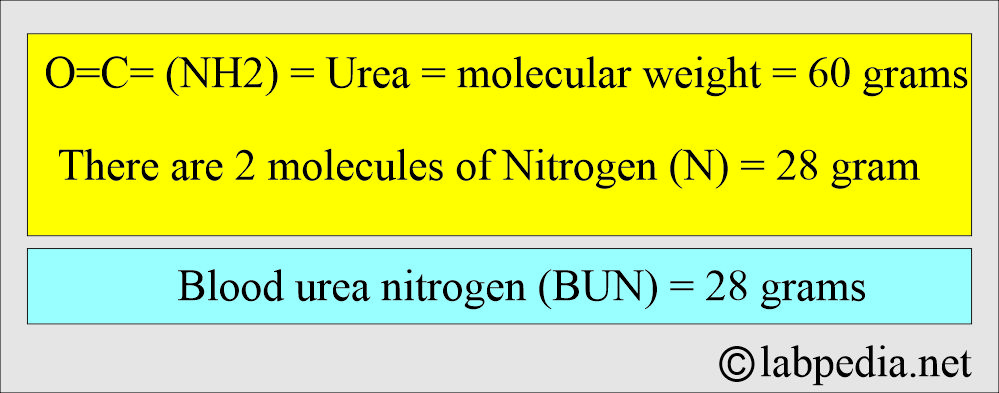
How will you calculate blood urea nitrogen (BUN)?
- To calculate BUN from the total blood urea = 60/28 = 2.1
- Now the value of blood urea nitrogen (BUN) will be = suppose Blood urea = 100 mg/dL = 100/2.1 = 47.6 mg/dL
How will you discuss the pathophysiology of blood urea nitrogen (BUN) and blood urea?
- Blood urea molecule: O = C = ( NH2 )2.
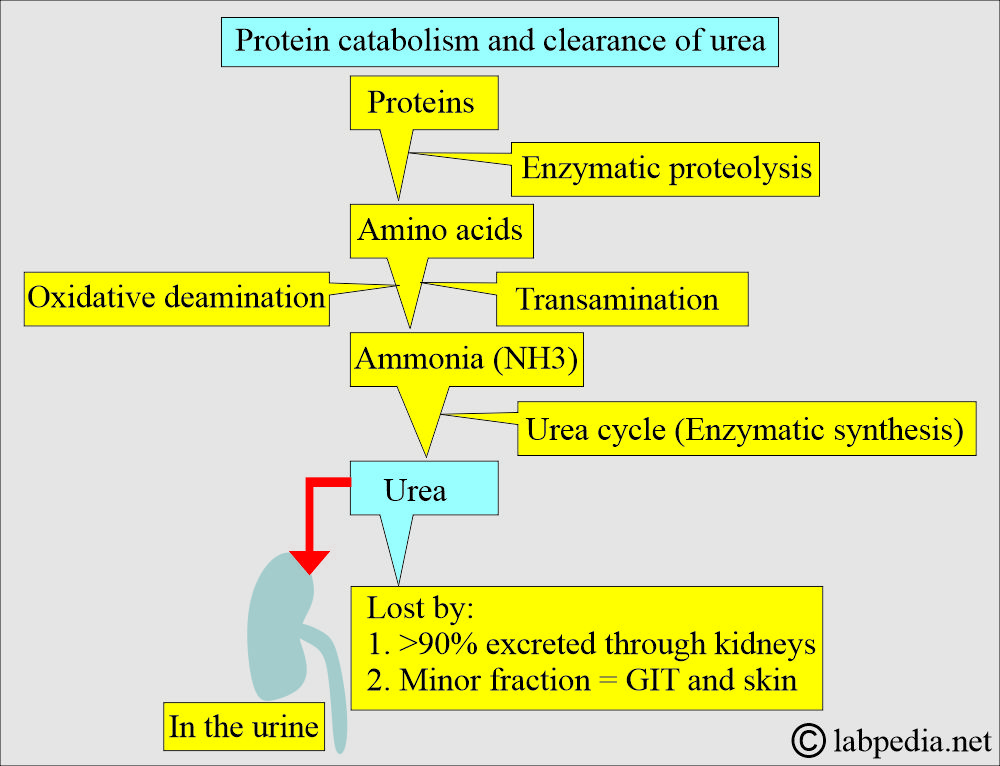
- Urea production and BUN increase when more amino acids are metabolized in the liver.
- This occurs with a high-protein diet, tissue breakdown, and or decreased protein synthesis.
- While urea and BUN production are reduced in the case of low protein intake and severe liver disease.
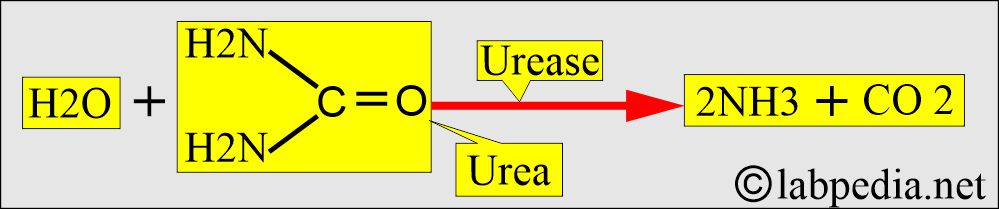
- The urease enzyme can split urea into ammonia and carbon dioxide.
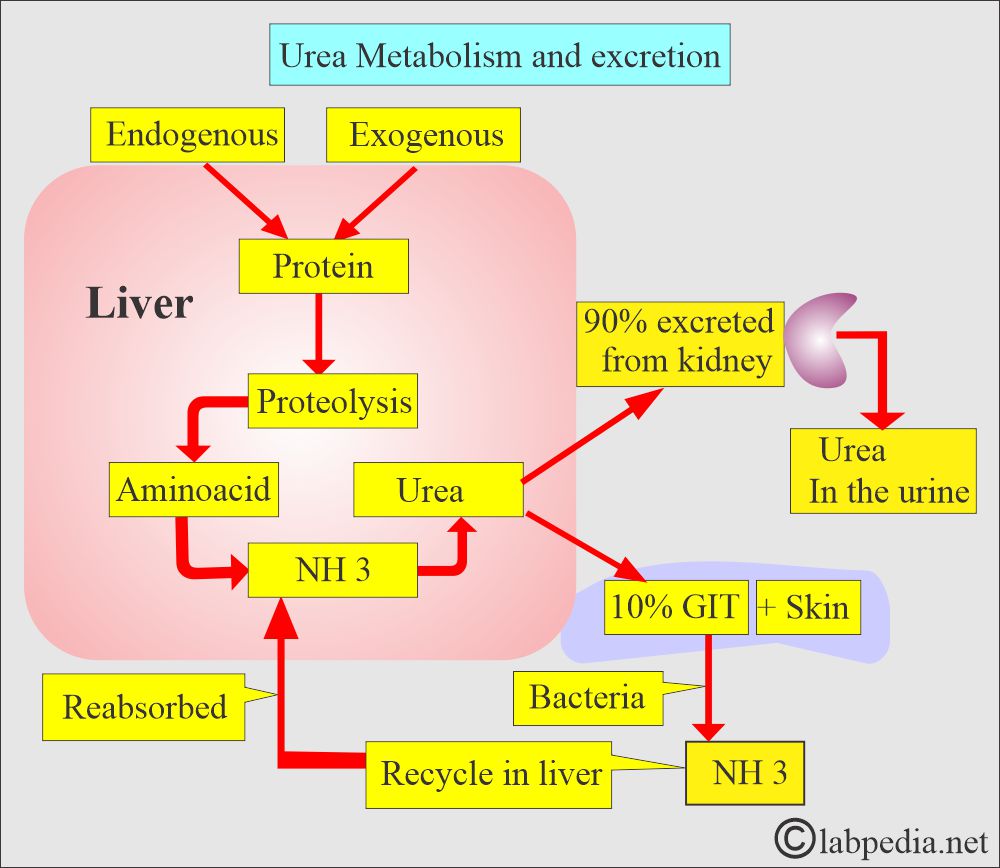
- >90% of the urea is excreted through the kidneys, the rest through the GIT and skin.
- Urea is freely filtered from the glomeruli.
- 40% to 70% of the urea is highly diffusible and moves passively out of the renal tubule into the interstitium and ultimately enters the blood.
- The molecular weight of urea = 60 grams
- Each molecule contains 2 nitrogen atoms = 28 grams. It is called blood urea nitrogen (BUN).
- While in the SI unit, this is meaningless because it is reported as mmol/L.
- The serum concentration of 28 mg/dL of urea-nitrogen (BUN) is equivalent to 60 mg/dL of blood urea or 10 mmol/L of urea or urea-nitrogen in SI units.
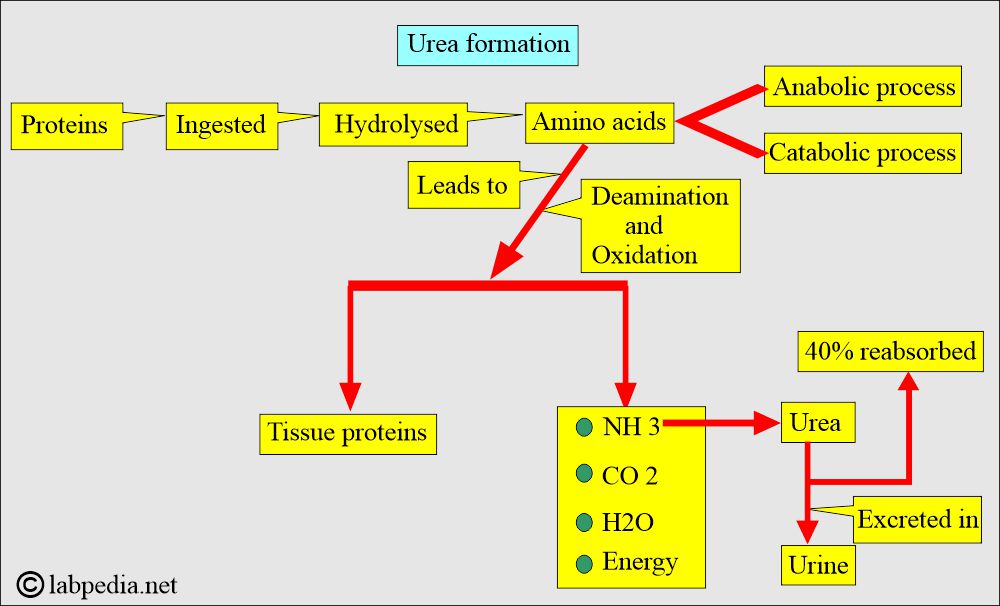
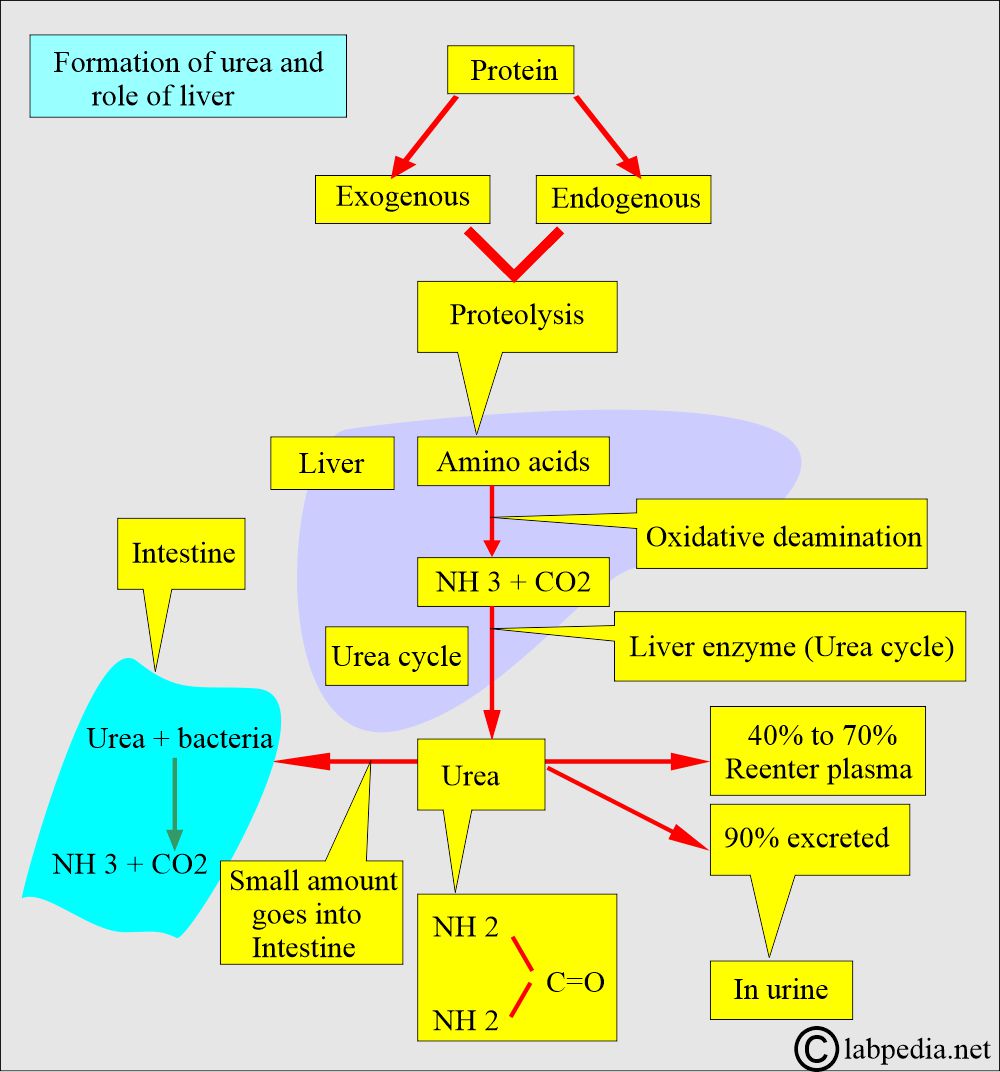
How will you discuss protein metabolism and the formation of urea?
- Proteins cannot be stored in the body. Surplus amino acids are catabolized for energy when they are in excess.
- The breakdown of the proteins and nucleic acids gives rise to a non-protein nitrogenous compound (NPN) in the blood:
- Urea. This is present in high concentrations in the blood. (45% of total NPN).
- Amino acids.
- Uric acid and Urates.
- Ammonia.
- Creatinine.
- Creatine
- Ammonia (NH3)
- Amino acids are converted into ammonia (NH3), CO2, H2O, and energy.
- NH3, before it reaches a toxic level, is prevented by the conversion of NH3 to urea.
- Urea is synthesized in the liver from carbon dioxide (CO2) and ammonia (NH3).
- CO2 and ammonia (NH3) are produced from the deamination of the amino acids in the urea cycle.
- While ammonia (NH3) forms urea, which is excreted into the urine. The conversion of NH3 to urea occurs in the liver.
- Urea is a water-soluble waste product that is excreted in the urine.
- Urea concentration in the glomerular filtrate is the same as in the plasma.
- Under normal conditions, 40% of the urea filtered is reabsorbed in the tubules.
What is the mechanism of urea clearance?
- Blood urea nitrogen is the main waste product of protein metabolism.
- Urea forms in the liver with CO2 and is the final product of protein metabolism.
- Urea is cleared by the kidneys.
- Urea is freely filtered and then partially absorbed by the nephron.
- 40% to 50% of filtered urea is reabsorbed by the proximal tubules.
- The BUN is used as an index of glomerular function in urea production and excretion.
- Urea reabsorption is increased in hypovolemia, so that BUN will underestimate the Glomerular filtration rate (GFR) and more in hypovolemia.
What is the role of the kidneys and liver in Blood urea/Blood urea nitrogen (BUN)?
- The toxic level of NH3 is prevented by converting the NH3 into urea, which occurs in the liver.
- Urea production and BUN increase when the liver has increased amino acid metabolism.
- It can occur by increased protein intake, tissue breakdown, or decreased protein synthesis.
- Urea levels decrease in cases of severe liver disease and low protein intake.
- Urea is degraded in the intestine to ammonium ions by the intestinal bacteria.
- This BUN, or urea, is excreted through the kidneys in the urine.
- The measurement of urea nitrogen indicates the ratio between urea excretion and production.
- Kidneys: Urea is filtered at the glomerulus, and approximately 40% to 50% is reabsorbed in the proximal tubules by passive back-diffusion.
- In normal conditions, urea clearance values parallel the glomerular filtration rate (GFR) at approximately 60% of its value.
- At a low level, when urine output is <2 mL/minute, the values are very inaccurate, even with the application of correction formulas.
- Urea, carried by the blood, is excreted in the urine by the kidneys.
- In the liver, amino acids are catabolized, producing free ammonia.
- Ammonia molecules combine to form urea.
- So, BUN depends upon the liver’s metabolic function and the kidneys’ excretory function.
- BUNis directly related to the liver’s metabolic function and the kidneys’ excretory function.
- In chronic renal diseases, the BUN level correlates better with the signs and symptoms of the patient than creatinine.
- As the synthesis of BUN depends upon life, patients with severe primary liver disease will have decreased BUN.
- In combined liver and renal disease, as in hepatorenal syndrome, the BUN may be normal due to poor liver function, which results in decreased urea formation.
- Overall, the BUN is less accurate than creatinine for renal diseases.
- In chronic renal diseases, BUN correlates more closely with symptoms than creatinine.
What is the relation between BUN level and the degree of azotemia?
| BUN level | Clinical implication |
|
|
|
|
|
|
|
|
|
|
|
|
- A high-protein diet may increase the BUN, while a low-protein intake may decrease its level.
- The blood urea nitrogen and creatinine ratio also helps explain renal, pre-renal, or post-renal diseases.
| Clinical condition | BUN |
|
Decreased |
|
Normal |
|
Increased |
|
Decreased |
How will you interpret BUN for renal function?
| BUN level | Clinical interpretations |
|
|
|
|
|
|
What is the clinical presentation of renal dysfunction (S/S of renal disease)?
- The patient may have edema around the eyes, legs, abdomen, and wrists.
- There is a history of fatigue, poor appetite, lack of concentration, and disturbed sleep.
- There may be flank pain in the kidney area.
- There may be burning urination, abnormal discharge, and increased frequency.
- There is a decrease in the amount of urine.
- The urine is bloody or coffee-colored and foamy.
- There may be hypertension.
What are the normal BUN and Urea levels?
Source 2
- Urea
- 20 to 40 mg/dl
- BUN
- Blood urea nitrogen (BUN) = 10 to 20 mg /dl
- Children (BUN) = 5 to 18 mg/dl
- Infants = 5 to 18 mg/dL
- Newborn = 3 to 12 mg/dL
- Cord blood = 21 to 40 mg/dL
- Older people may have a higher level than adults.
Source 1
| Age | Urea nitrogen mg/dL |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Source 3
Blood urea nitrogen (BUN)
- Adult = 10 to 20 mg/dL
- Older people have a higher value
- Cord blood = 21 to 40 mg/dL
- Newborn = 3 to 12 mg/dL
- Infants = 5 to 18 mg/dL
- Child = 5 to 18 mg/dL
A level above 100 mg/dL is the critical value indicating severe renal dysfunction.
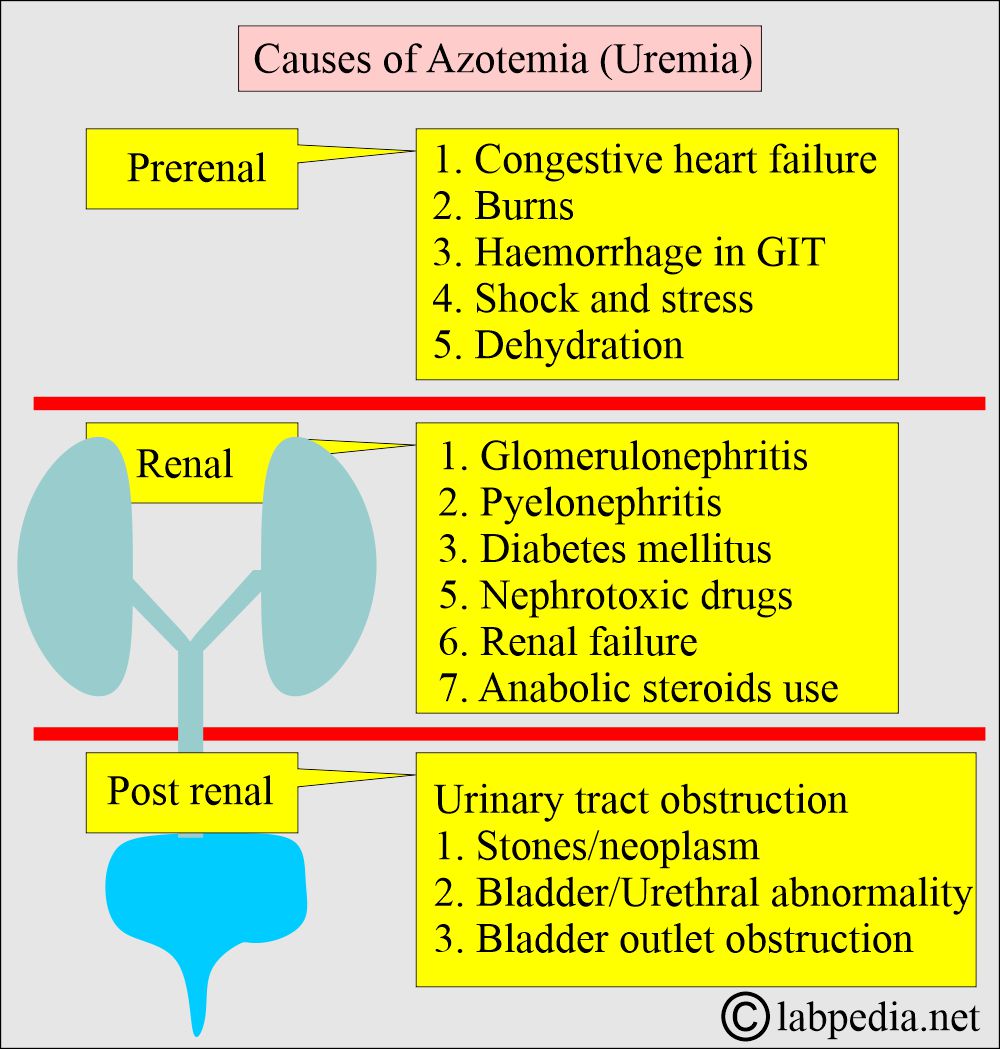
What are the causes of increased Urea (BUN), Azotemia?
A. Impaired renal function:
- Prerenal causes:
- These are mostly due to decreased blood flow to the kidneys.
- Congestive heart failure and Myocardial infarction (CHF).
- Salt and water depletion.
- Shock.
- Stress.
- Acute MI.
- Hemorrhage in the GI tract.
- Dehydration.
- Excessive protein catabolism.
- Burn.
B. Chronic renal diseases:
- Renal causes:
- Any urinary tract obstruction also increases the BUN/creatinine ratio. In the case of protein catabolism, the serum creatinine is normal.
- Glomerulonephritis (GN).
- Pyelonephritis (PN).
- Acute tubular necrosis.
- Renal failure.
- Diabetes mellitus with ketoacidosis.
- Anabolic steroid use.
- Nephrotoxic drugs.
C. Urinary tract obstruction:
- Postrenal causes
- Ureteral obstruction from stones, tumors, or congenital abnormalities.
- Bladder outlet obstruction from prostatic hypertrophy or cancer.
- Bladder/urethral congenital abnormality.
What are the common causes of uremia?
| Type of uremia | Etiology | Causes |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What are the causes of decreased Urea/BUN?
- Severe liver diseases (liver failure).
- Malnutrition and a low-protein diet.
- Impaired absorption in Celiac disease.
- Syndrome of inappropriate antidiuretic hormone secretion.
- Increased utilization of protein for synthesis:
- Late pregnancy.
- Acromegaly.
- Infants.
- Anabolic hormones.
- Malnutrition.
- Overhydration.
- Nephrotic syndrome.
What is the effect of drugs and other conditions on a BUN?
- Some drugs that may cause a decrease in BUN include Dextrose infusion, Phenothiazine, and Thymol.
- Increased BUN levels may be observed in late pregnancy and infancy due to the increased utilization of proteins.
Questions and answers:
Question 1: What is the difference between blood urea and blood urea nitrogen (BUN)?
Question 2: What are the causes of decreased BUN in late pregnancy?