Summary of Routine Important Blood Tests
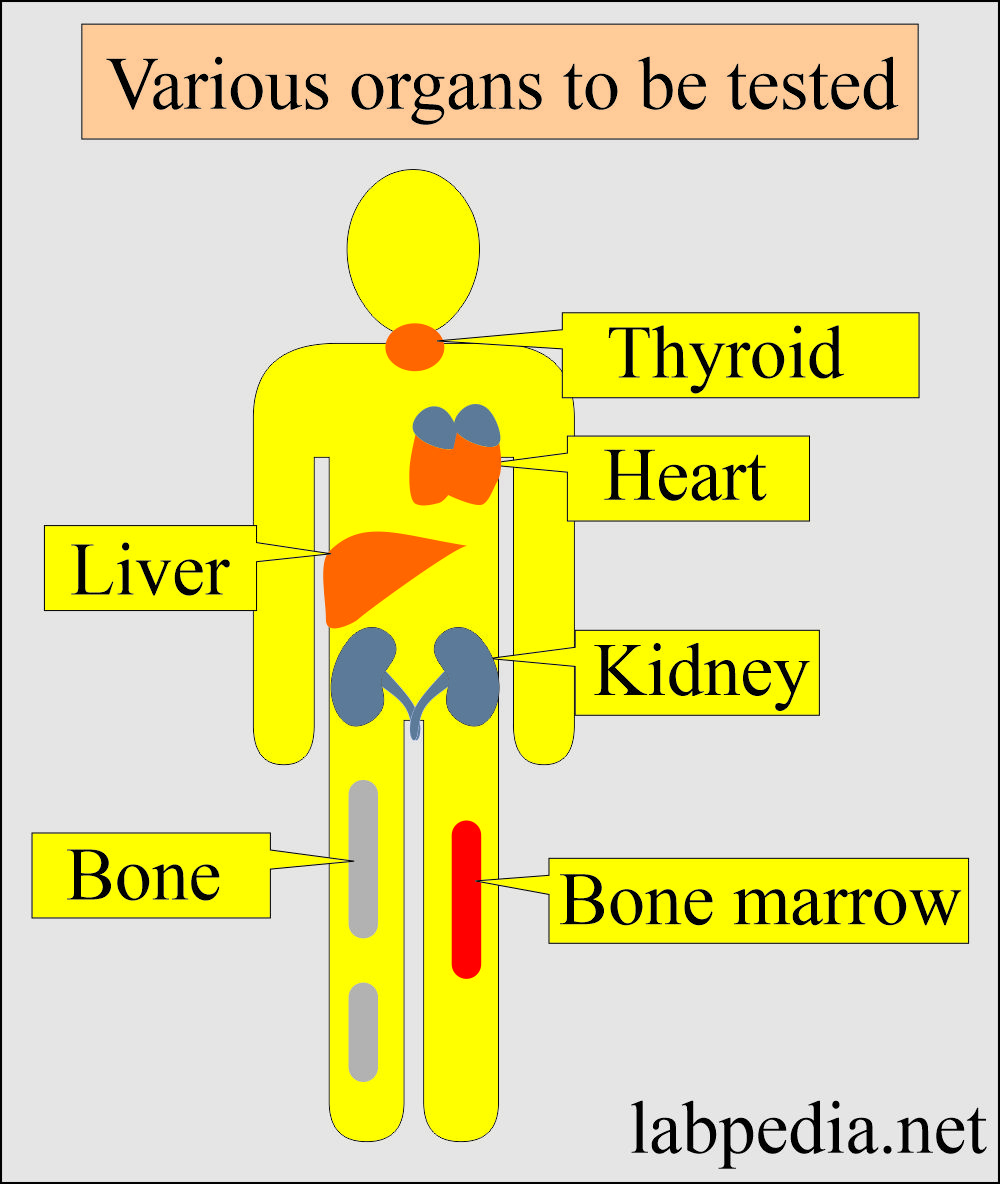
How would you describe a summary of various organs that need tests?
- Blood tests are mainly used to investigate various diseases.
- The most common tests are described, and their indications are given.
What samples are needed for various lab tests?
- Mostly, tests are done on the patients’ serum.
- Plasma can be used in some cases.
- Some time we need random urine or 24 hours urine sample.
Summary of various organ tests?
| Important Blood Tests | Normal values | Clinical Importance |
| Biochemical parameters |
||
|
|
It can evaluate:
|
|
|
Used for:
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Hematology | ||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Hormones | ||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Free testosterone
Women
Total testosterone
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Tumor markers | ||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Cardiac markers | ||
|
|
|
|
|
|
|
|
|
|
|
|
Questions and answers:
Question 1: Which test is important to diagnose AMI?
Question 2: What is the importance of myoglobin?
Question 3: What is the significance of PSA?