Blood banking:- part 2 – Definition of blood banking, Donor selection, Cross Match Procedure, and Compatibility test
Blood banking
Sample for Blood banking
- Patient (recipient), venous blood in the disposable syringe is taken.
- Take the blood sample from the donor.
History of blood banking:
- In 1492 blood was taken from three young men and given to pope innocent VII in the hope of curing him. Unfortunately, all four died.
- This was the first time when a blood transfusion was recorded in history.
- Clotting was the main problem.
- Attempts to find nontoxic anticoagulants began in 1869 when sodium phosphate was recommended by Braxton and Hicks.
- Karl Landsteiner, in 1901 discovered the ABO blood groups in mankind. He also discovered the serious blood transfusion reaction due to the ABO system. He won the Nobel Prize.
- Edward E. Lindemann was the first person who succeeded in carrying out a vein-to-vein blood transfusion. This was a time-consuming procedure.
- Later on, Unger designed a special syringe-valve system that could transfuse blood without the help of anybody.
- In 1914, there was a breakthrough when Hustin reported using sodium citrate and glucose as a diluent and anticoagulant solution for the transfusion.
- In 1915, Lewisohn determined the minimum amount of nontoxic citrate needed for anticoagulation and transfusion. Then transfusion became more practical and safer for the patient.
- In 1916, Rous and Turner introduced the dextrose-citrate solution to preserve the blood.
- The common use of glucose was delayed as a preservative for the RBCs.
- World War II increased research on preserving blood and plasma because of the demand.
- Dr. Charles Drew’s work during world war II for preserving and transfusing blood led to a widespread system of blood banks.
- In 19041 February, Dr. Charles Drew was appointed the first American red cross society director at Presbyterian Hospital.
- 1943 Loutit and Mollison of England introduced the acid-citrate dextrose solution (ACD) formula.
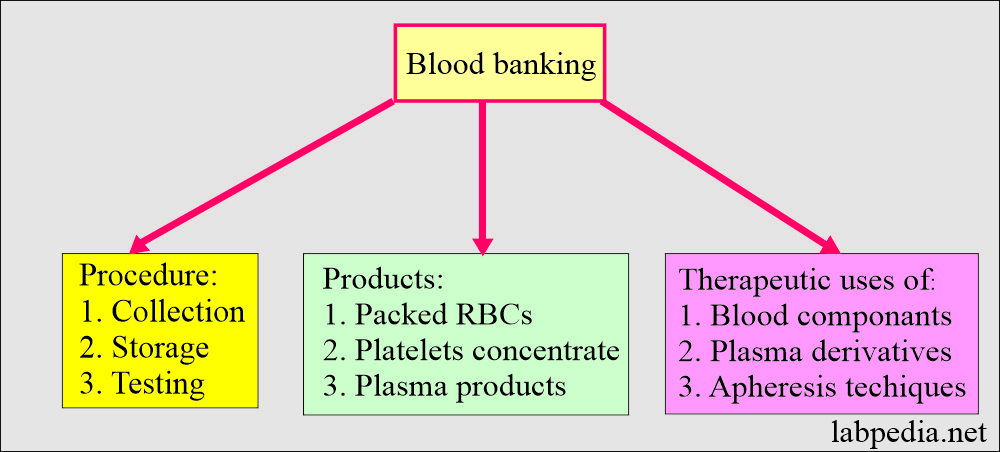
Definition of blood banking
- This is collecting, storing, and testing the blood components and derivatives.
- There is a therapeutic use of blood components, plasma derivates, and apheresis technology.
- It includes collecting, storing, and using hematopoietic and other blood-derived cells.
- Whole blood may be fractionated into:
- Packed RBCs.
- Platelets.
- Plasma products.
- Plasma after processing provides:
- Albumin.
- Blood coagulation factors concentrate.
- Immunoglobulins preparation.
Purpose of blood cross-matching (Indications):
- The primary purpose of the crossmatch is to prevent a transfusion reaction.
- Crossmatch is done before the major surgery.
- Crossmatch is also done before an operation where blood is usually unnecessary, e.g., hysterectomy and cholecystectomy.
- Packed RBCs transfusion:
- Anemia is when the hemoglobin is <7 G/dL or hematocrit <21% without cardiovascular function complications.
- Hb <10 g/dl and HcT <30% in patients with cardiovascular disease, sepsis, or hemoglobinopathy.
- Platelets transfusion:
- Prophylactically in the case of platelets count <10,000/cmm in adults and <50,000/cmm in neonates.
- In case of bleeding when platelets are <30,000/cmm.
- In the case of postoperative bleeding, when the platelets count is <50,000/cmm.
- In the case of the post-cardiopulmonary bypass, when the platelets are <100,000/cmm.
- Fresh frozen plasma:
- When the INR ≥ 2 and in the case of bleeding.
- In the case of nose bleeds, when the INR is ≥ 6.
- In thrombotic thrombocytopenic purpura.
- Cryoprecipitate:
- In the case of dysfibrinogenemia.
- When the fibrinogen is <100 mg/dL.
- In the case of Von Willibrand disease.
Precautions for the selection of donor (rejection of the donor):
- Do not take blood from the donor if:
- Blood was donated in less than 8 weeks.
- Poor health like cancer, cardiopulmonary disease, and bleeding disorder.
- Pregnancy during and after 6 weeks of delivery.
- The blood pressure is more than 180/100.
- Pulse when 50/min or more than 100/min. The only exception is the athlete, where the pulse is usually slow.
- Hemoglobin is <12.5 g/dL or hematocrit <38%; such donors are rejected.
- History of infectious agents:
- The donor with a history of viral hepatitis like HBV, HCV, HIV, etc.
- The donor with Malaria or coming from a malarial area should avoid giving blood for three years.
- The venereal disease person should not give blood for at least one year (Syphilis or Gonorrhoea).
- A person with rubella or varicella vaccination should not give blood for 4 weeks.
- Donor if running fever > 99.5 °C.
- The donor with leukemia or lymphoma.
- History of recent surgery or illness needs to be considered unfit. In case of illness, at least there should be a 2 to 3 weeks interval free of any signs/symptoms after the recovery.
- After the surgery, it depends upon the type of surgery, and if he is under the supervision of a physician should be deferred.
- If the donor has a cold, influenza, or tooth extraction, it should be deferred for one week.
- Donors with a history of allergies and allergies to drugs should be rejected.
- Donors on drug medication, like antihypertensive drugs, antibiotics, and corticosteroids, should be rejected.
- Donors who have recent vaccination should be deferred for at least one week.
- If there is H/O drug abuse.
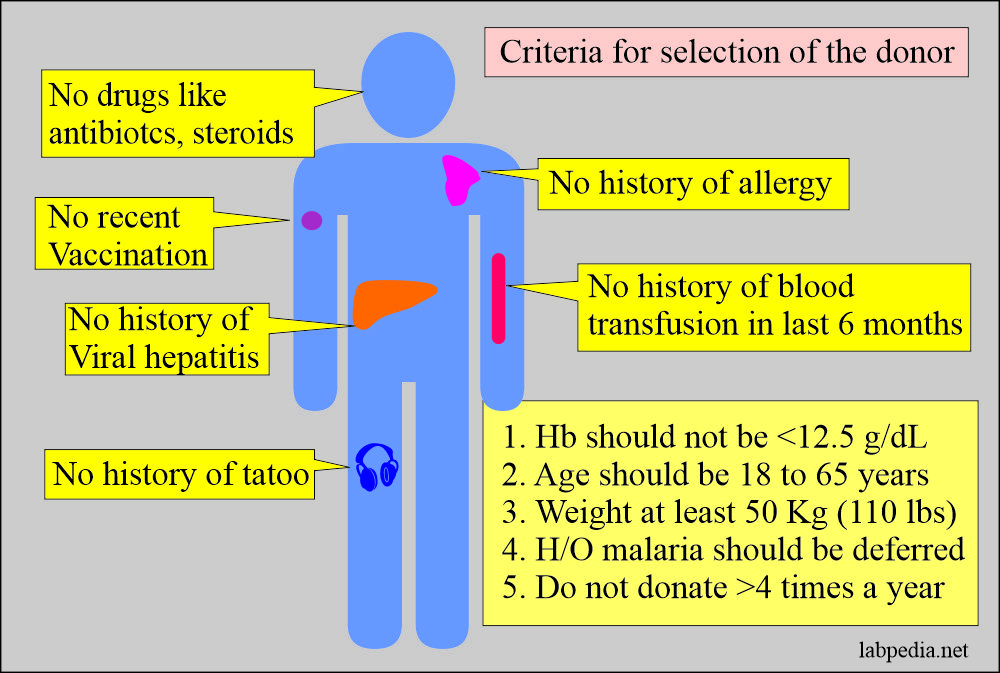
Criteria for the selection of the blood donor:
- History of the donor:
- There is no history of viral hepatitis in the last 6 months.
- No history of blood transfusion in the last 6 months.
- There should be no contact with the patient with viral hepatitis.
- Avoid drug addicts.
- No history of tattooing in the last 6 months.
- Avoid blood positive for HBV or HCV, or HIV.
- Hemoglobin should be at least 12.5 G/dL. This should be checked before taking the blood.
- Hct should be 38%, in the normal range.
- Age: Ideal age is between 18 to 65 years.
- Bodyweight: The donor should weigh at least 50 kg (110 lbs).
- The temperature should not be >99.6 °C. The purpose of the temperature is to avoid the transfer of the infection to the recipient.
- The pulse should be 50 to 100 beats/minute. Pulse rate >100/minute should be further evaluated.
- A pulse rate <50/minute may be found in the athlete.
- The donor may have anxiety, so allow him to relax for 10 to 15 minutes, then recheck the pulse.
- If still, the pulse is >100/minutes, then defer the donor.
- Blood pressure systolic should not be >180 mmHg, and diastolic not be >100 mmHg. These donors need to be evaluated before these donors are accepted.
- History of recent immunization: Defer this donor for at least one week till they have no signs and symptoms.
- Check skin lesions in the antecubital area to rule out habitual drug abuse.
- These donors are deferred because of the risk of Hepatitis virus or HIV infection,
- Check for psoriasis lesions, skin eruptions like such as poison ivy, and rash.
- History of malaria: Such donors with a history of malaria should be deferred for at least three years. The people who have traveled to the malarial area should also be deferred for three years.
- History of donation: Avoid professional donors because they always have low hemoglobin.
- The donor should not donate blood more than 4 times a year.
- Males should donate more than females.
- Females should donate less than males because of the menstrual cycle, where they may lose one point of blood annually.
- History of present or recent surgery or illness: Donors with long-standing illnesses should be excluded. Donors with recent surgery or hospitalization should be rejected.
Donors’ Medical history consists of the following:
- Have you ever had jaundice?
- Do you have H/O liver diseases?
- Do you have positive tests for viral hepatitis?
- Do you have blood donations in the last 12 months?
- Do you have organ transplantation?
- Do you have acupuncture in the last 12 months?
- Do you have close contact with the patient having yellow jaundice or hepatitis?
- H/O of malaria or intake of malarial drugs in the past 3 years?
- Is there H/O cancer, blood disease, or bleeding problems?
Summary of Donor selection criteria:
- In general appearance, the donor should be in good health.
- Temperature orally should not exceed 99.6 °C (37.5 °C).
- The pulse should be 50 to 100/minute and should not exceed this limit. The Pulse >100/minute should be further evaluated.
- Age of the donor. Don’t take blood from old senior persons.
- Blood pressure systolic should not be >180 and diastolic >100 mm Hg.
- Weight of the donor. The ideal weight maybe 110 lb (50 kg)
- Level of hemoglobin and Hematocrit (Hct). Hb at least 12.5 g/100 mL and Hct 38%.
- Frequency of blood donation per year.
The medical history for rejection of the donor:
- Infections of the donor include a history of viral infections, H/O malaria, or taken antimalarial drugs or H/O major surgery or illness.
- H/O psoriasis and its treatment.
- If there is H/O chest pain, heart disease, or lung disease.
- If there is H/O cancer, blood diseases, or bleeding disorder.
- If there are H/O convulsions, seizures, or fainting spells.
- If the donor has had a vaccination in the last 4 weeks.
- H/O extraction of teeth and dental works.
- Positive syphilis test in the last 12 months.
- If the positive test for AIDS.
Approved blood preservatives in use are:
| Preservatives name | Abbreviation used are | Storage time limit |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Comparison of the allogeneic donors and autologous donors (fitness of the donors):
| Clinical parameter | Autologous donor | Allogenic donor |
| Hemoglobin level | >11 g/dL | >12 g/dL |
| Hematocrit (Hct) | >33% | >38% |
| Screening for the infectious disease | Not needed | Needed (HBS, HCV, HIV, Syphilis) |
| The interval between the blood donation | Only 72 hours | At least 8 weeks |
| Type of donor | Self (same person, before surgery) | Volunteer |
Doner’s blood tests are the following:
- ABO typing.
- Rh typing.
- Hepatitis B surface antigen.
- Hepatitis Core B antibody (HBc-IgM).
- Hepatitis C antibody.
- For Syphilis (VDRL).
- HIV.
- SGPT (ALT).
- If possible, do PCR for HCV and HIV.
To rule out the possibility of infectious diseases, advise these tests:
- Must do to rule out:
- Serologic test for syphilis.
- Antibody to HCV (hepatitis C virus).
- HCV RNA.
- HBS antigen (hepatitis B surface antigen).
- Antibody to Core-antigen (antibody to HBV core antigen).
- Antibody to HIV-1 and HIV-2.
- HIV-1 RNA
- West Nile virus RNA
- Screening for bacterial infection can do platelets count only.
- Optional and may be needed in some areas:
- CMV antibody.
- SGOT/SGPT for any abnormality in the liver. Sometimes this simple test helps to rule out hepatotropic virus infection.
Procedure for the blood donation:
- Blood bags should not be released before it is tested for:
Before issuing the blood bag for donation, all blood bags are tested as follows:
Advise forward blood grouping (Donor’s RBCs):
- ABO typing.
- Rh typing, including weak D antigen in the case of D negative.
- All Rh0 (D) negative units are confirmed and tested with anti-CD and anti-DE.
- Du tests are performed on all r’ and r” units.
- Screening for non-ABO donor antibodies.
Advise reverse blood grouping (Donor’s serum):
- Antibody screening tests using enzyme and antiglobulin methods.
- Advise VDRL test for syphilis.
- Advise Hbs Ag and HbS Ab test.
Recipient blood screening includes:
- ABO typing.
- Rh typing.
Cross-Matching:
History of blood cross-matching (compatibility testing):
- This was introduced by Ottenberg in 1908; the direct compatibility test, or cross-match, between the donor and the recipient (patient), was absolutely important for safe blood transfusion.
- The direct cross-match was preceded by antibody screening for several decades as part of patients’ pretransfusion testing.
- In 1960, phenotyped RBCs were used for this purpose and were commercially available.
- In 1964, Grove-Rasmussen advised the need for the antiglobulin test as part of the crossmatch when antibody testing was negative.
- Two main functions of the crossmatch are:
- This is a final check for the ABO compatibility between the patient and the donor.
- This may detect the antibody in the patient’s serum that was not detected in antibody screening.
- Major crossmatch is much more important than minor crossmatch.
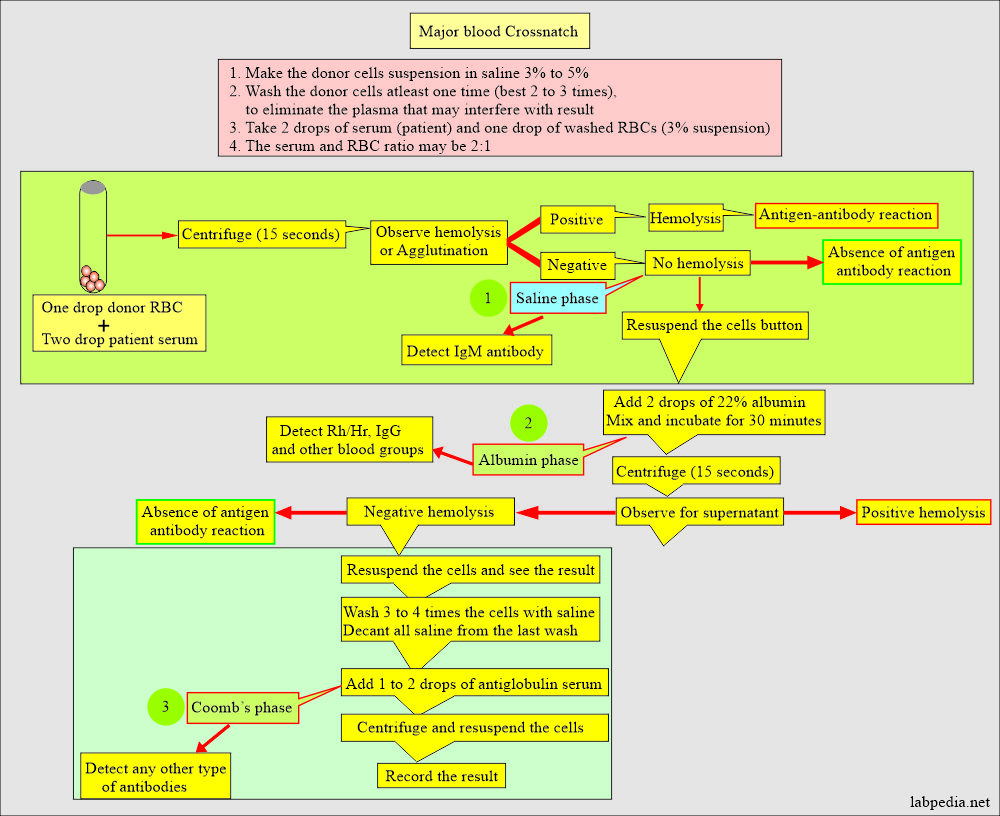
Procedure for blood cross-matching:
- Make the Donor’s RBCs suspension in the normal saline.
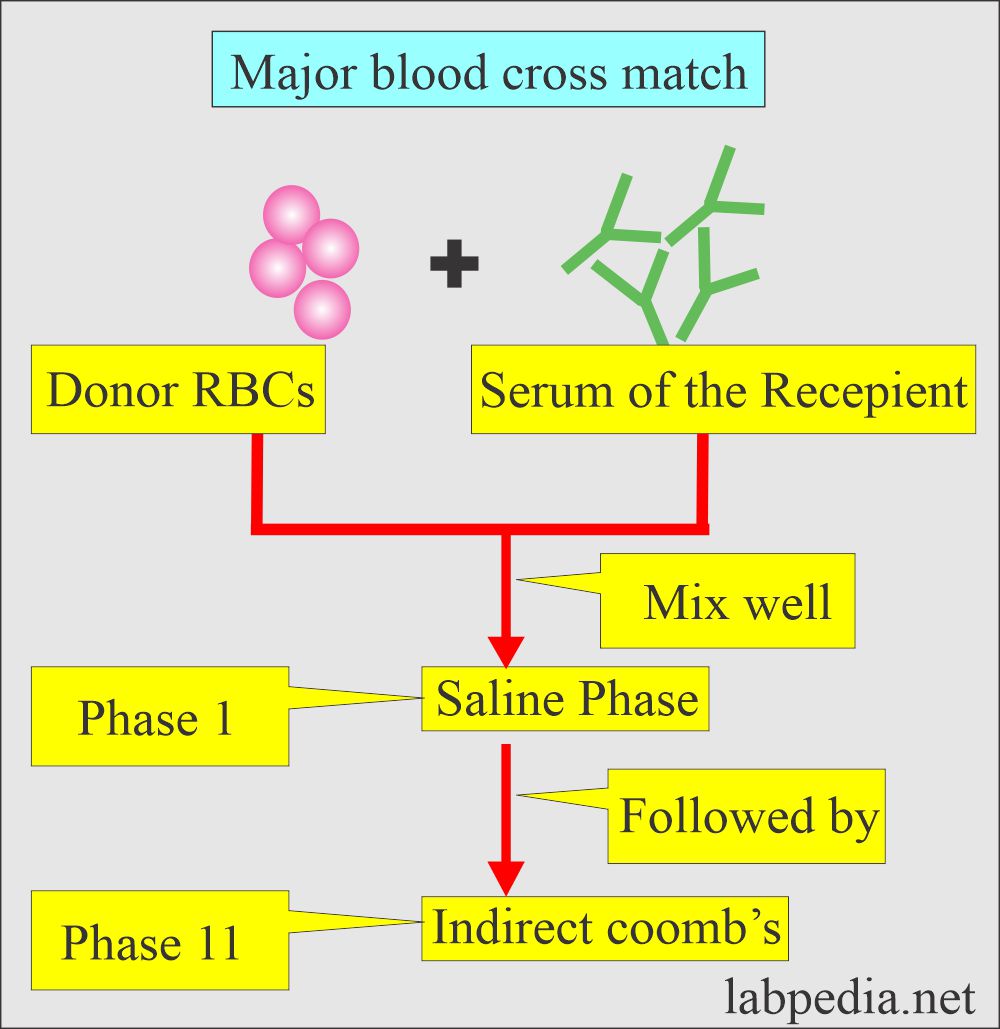
Major blood cross-match:
- It is also called a direct cross-match.
- Donor RBC and recipient serum are mixed in the saline phase.
- This is followed by an indirect Coombs test, where the above RBC is washed with saline three times, and then Coomb’s serum is added.
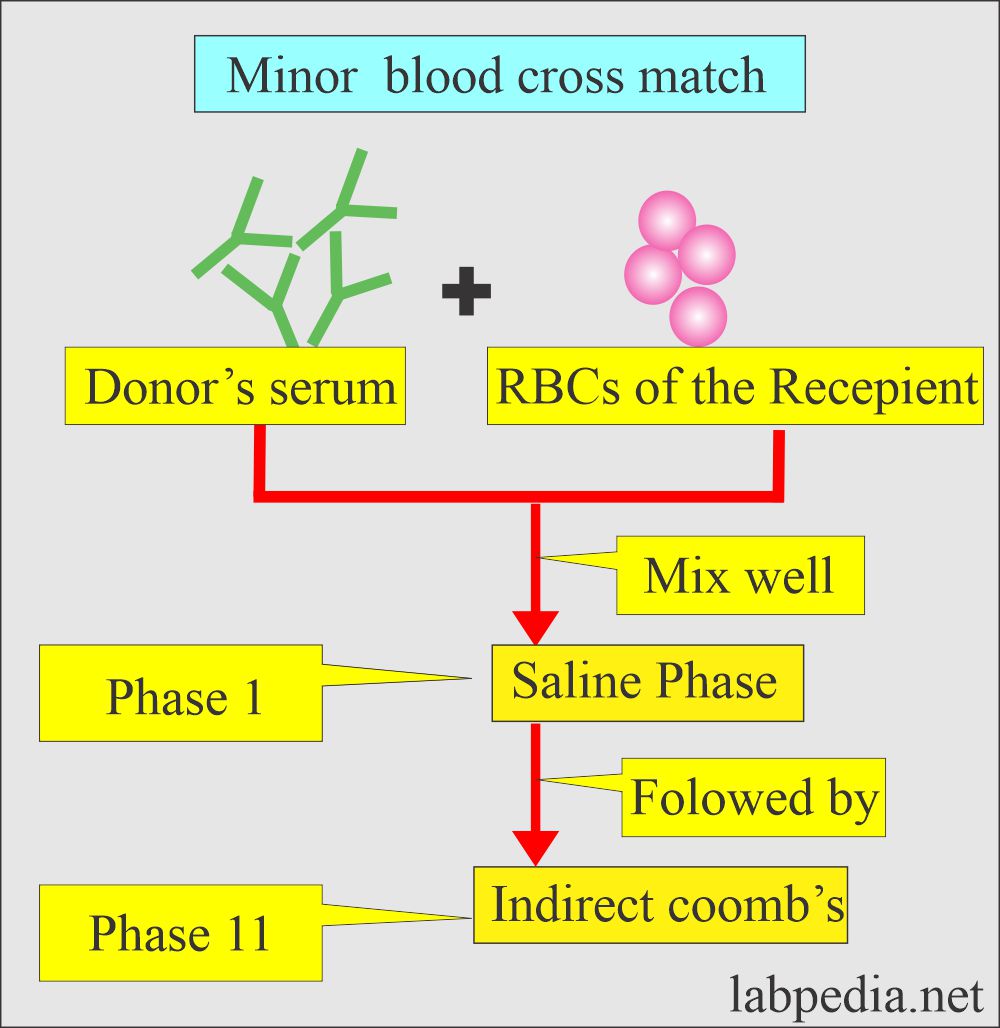
Minor blood cross-match:
- It is also called the reverse cross-match.
- Now take recipient RBC and donor serum.
Read the crossmatch:
- Negative = No cell clumping or hemolysis should be seen (No agglutination should be observed).
- Positive = Shows agglutination or hemolysis.
ABO donor and recipient compatibility:
| Donor’s blood group | Antigen | Antibody | Recipient blood group |
| Blood group O | None | Anti-A and B | O, A, B, AB |
| Blood group A | Antigen- A | Antibody- B | A, AB |
| Blood group B | antigen-B | Antibody- A | B, AB |
| Blood group AB | Antigen-A and B | None | A, B |
Blood grouping and cross-match:
| Blood grouping and compatibility: | Donor blood group | ||||
| O (universal donor) | A | B | AB | ||
| Recipient blood groups | O | Compatible | Incompatible | Incompatible | Incompatible |
| A | Compatible | Compatible | Incompatible | Incompatible | |
| B | Compatible | Incompatible | Compatible | Incompatible | |
| AB (universal recipient) | Compatible | Compatible | Compatible | Compatible | |
Blood components:
Whole blood:
- Proper storage of the blood is crucial:
- Whole blood needs to be stored at a constant 4 °C (± 1 °C).
- At this temperature, bacterial growth and cell metabolism slow down.
- Some researchers say that a temperature of 2 °C is better, but the disadvantages are:
- White blood cells and platelets become irreversibly clumped at this temperature.
- Also, at 2 °C, RBCs are swollen due to the presence of dextrose, become fragile, and maybe hemolyzed.
- At temperature >10 °C:
- Bacterial growth is enhanced.
- Cell survival is decreased by around 20%.
When blood is stored for some time, the changes seen are:
- Blood deterioration starts when stored in Citrate phosphate dextrose anticoagulant (CPD) or Acid Citrate Dextrose anticoagulant (ACD) within the collection of a few days.
- RBCs will lose their ability to metabolize glucose.
- The cells suffer the loss of K+ to plasma.
- The osmotic and mechanical fragility is increased.
- There is a loss of membrane lipids.
- The survival of the RBCs is lost in vivo:
- 5% after the first week.
- 10 to 15% after 2 weeks.
- 15 to 30% after 3 weeks.
- The addition of Adenine (Adenine+CPD) will prolong the shelf life of RBCs to 35 days.
- In storage, there is a decrease in the 2,3-diphosphoglycerate (2,3-DPG) and Adenosine triphosphate (ATP).
- The concentration of the 2,3-DPG is better maintained in the CPD than in the ACD.
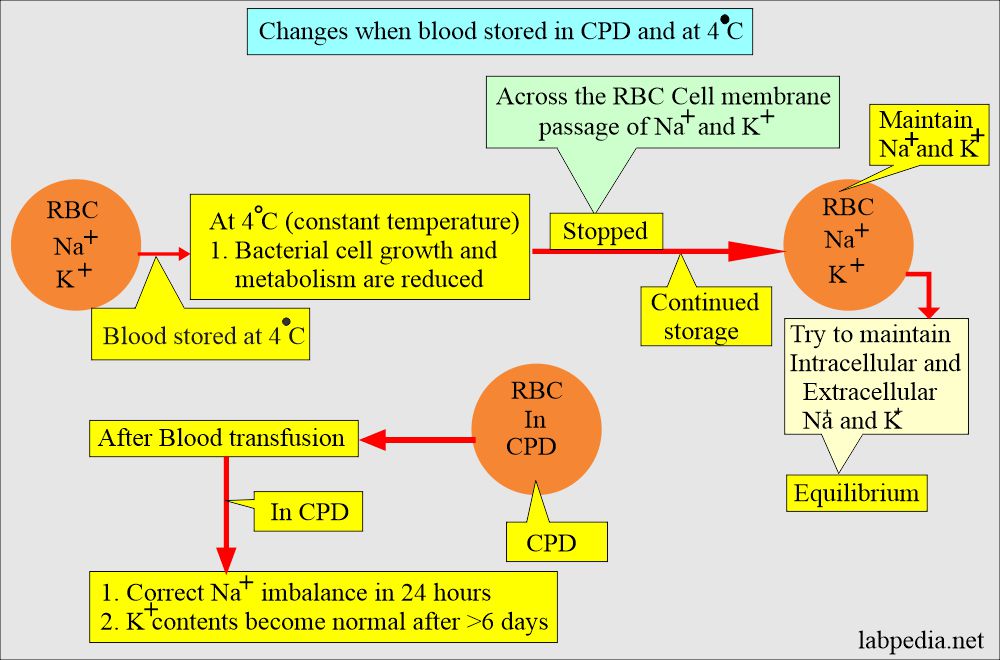
- Blood stored at 4 °C stops the transport of the Na+ and K+ across the RBCs membrane.
- If storage is continued, then:
- In that case, Na+ and K+ intracellular and extracellular concentrations are maintained.
- After the blood transfusion in CPD, Na+ is corrected within 24 hours.
- But the K+ level does not become normal and takes >6 days.
- If storage is continued, then:
- Uses of the whole blood:
- It is advised in patients with enough acute blood loss leading to hypovolemia.
- This may be given in patients with severe anemia, preferably by giving packed RBCs.
Fresh frozen plasma (Plasma):
- Plasma is separated from the RBCs by centrifugation at 4 °C and is frozen as rapidly as possible.
- This is stored at -30 °C for a maximum period of one year.
- At -20 °C can store for 3 months.
- In the storage of fresh frozen plasma, deterioration occurs for labile clotting factors.
- Use of the fresh frozen plasma:
- It is used for the deficiency of labile coagulation factors.
- With concentrated RBCs and frozen plasma.
- Stored plasma is useful in treating protein replacement or increasing blood volume.
- Stored plasma is also used in burns, hypovolemic shock, coagulation factors deficiencies ( except factors V and VIII), and an anticoagulant reversal.
Packed red blood cells:
- When Red blood cells concentrate is prepared in a closed atmosphere, the cells’ sterility is unaffected.
- In this way, you can avoid bacteria proliferation.
- These are used to avoid disturbing Hct and circulatory overload.
- This will also avoid the reaction because of the donor antibodies.
- Uses of packed RBCs:
- This is indicated where the Hct needs to be increased without affecting the blood volume, e.g., anemia.
- Packed cell’s advantages over the whole blood are:
- This will minimize circulatory overload.
- This will reduce the reaction due to the donor antibodies.
- It will reduce the quality of anticoagulants and electrolytes transfused in whole blood.
- It will minimize the reaction due to plasma components.
The difference between the whole blood and packed cells:
| Characteristic features | Packed cells | Whole blood |
| Hct % | 70 ± 5 | 40 ± 5 |
| Volume of transfusion | 300 ± 25 mL | 500 ± 25 mL |
| Plasma volume | 100 ± 25 mL | 300 ± 25 mL |
| RBC volume | 200 ± 25 mL | 200 ± 25 mL |
| Albumin contents are | 4 to 5 grams | 10 to 12 grams |
Human serum albumin:
- This is prepared from normal human plasma.
- Human albumin is prepared by cold ethanol plasma fractionation and is available in a 5% or 25% concentration.
- 25% albumin is stored at 2 to 8 °C and should not be frozen.
- 5% albumin is stored at room temperature, and the temperature should not exceed 37 °C and should not be frozen.
- The shelf life for both products is 3 years; expiry dates should not be ignored.
- Storage has no effect if it is stored at the proper temperature and used before the expiry dates.
- Uses of the human albumin:
- It is used in the case of shock due to hemorrhage or surgery.
- This can be used as a fluid replacement during manual or automated therapeutic plasma exchange.
- In the case of neonatal hyperbilirubinemia.
- A complication of human albumin is:
- The patient may have a pyogenic or allergic reaction.
- There may be a hypotensive reaction.
- The above S/S disappears when the infusion is slowed down or stopped.
- The patients may have dilutional anemia.
- It should not be given to patients with contraindications in a rapid increase in the volume affecting their health.
Gamma Globulin (Immune serum Globulin):
- Immune serum globulins are stored at 2 to 8 °C for 2 years without any deterioration.
- Uses of the immunoglobulins are:
- These are given to boost passive immunity (passive antibody) and protect against exposure to some diseases.
- In congenital immune deficiency disorders.
- These immunoglobulins are effective in:
- Measles.
- Hepatitis A infection.
- Hypogammaglobulonemia.
Antihemophilic factor (Factor VIII concentrate):
- Factor VIII concentrate is obtained from the pooled fresh frozen plasma.
- This is in lyophilized form, and it should be stored at 2 to 8 °C and should not be frozen.
- This can be stored at room temperature for a short limited period of time.
- Cruprecipitate factor VIII is prepared from a single donation of fresh blood by cold precipitation.
- Uses of the antihemophilic factor VIII:
- This is used in the case of hemophilia A (congenital factor VIII deficiency).
- In the cases of acquired factor VIII inhibitors.
Platelet-rich plasma or platelet concentrate:
- Platelet-rich plasma concentrate can be stored at room temperature for up to 72 hours with constant agitation.
- Effect of storage: With time, there is a progressive decrease in hemostatic efficiency.
- After 72 hours, the pH falls to 6.0, where the platelet’s hemostatic activity is lost or decreased.
- Now plastic bags (O2 diffusible) are available where the platelet activity remains for 5 days.
- Uses of platelets concentrate:
- It is used to treat or prevent thrombocytopenia.
- These are used to treat bleeding disorders due to platelet functional disorders.
Blood components and their indications:
| Components | Composition | Indications |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Questions and answers:
Question 1: What is the major cross-match?
Question 2: What is minor cross-match?

thkyou a lot.
Thanks a lot.
Most relevant.
Thanks
Thanks.