Blood banking:- part 2 – Donor selection, Cross Match Procedure, and Compatibility test
Blood Banking, Donor Selection
What type of blood sample is needed?
- The patient (recipient) has their venous blood taken in a disposable syringe.
- Take the blood sample from the donor.
What is the History of blood banking?
- In 1492, blood was taken from three young men and given to Pope Innocent VII in the hope of curing him. Unfortunately, all four died.
- This was the first recorded instance of a blood transfusion in history.
- Clotting was the main problem.
- Attempts to find nontoxic anticoagulants began in 1869 when Braxton and Hicks recommended sodium phosphate.
- Karl Landsteiner, in 1901, discovered the ABO blood groups in humans. He also found the severe blood transfusion reaction due to the ABO system. He won the Nobel Prize.
- Edward E. Lindemann was the first person to carry out a vein-to-vein blood transfusion successfully. This was a time-consuming procedure.
- Later on, Unger designed a special syringe-valve system that could transfuse blood without assistance.
- In 1914, a breakthrough occurred when Hustin reported using sodium citrate and glucose as a diluent and anticoagulant solution for transfusion.
- In 1915, Lewisohn determined the minimum amount of nontoxic citrate needed for anticoagulation and transfusion. Then, transfusion became more practical and safer for the patient.
- In 1916, Rous and Turner introduced the dextrose-citrate solution to preserve the blood.
- The common use of glucose was delayed as a preservative for red blood cells (RBCs).
- World War II led to increased research on preserving blood and plasma due to the demand.
- Dr. Charles Drew’s work during World War II in preserving and transfusing blood led to the development of a widespread system of blood banks.
- In February 1941, Dr. Charles Drew was appointed the first American Red Cross Society director at Presbyterian Hospital.
- In 1943, Loutit and Mollison of England introduced the acid-citrate-dextrose (ACD) solution formula.
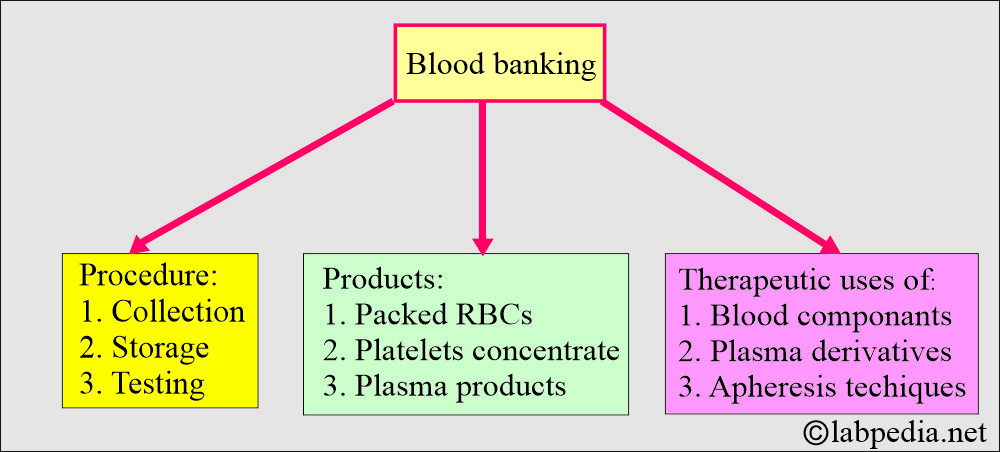
How will you define blood banking?
- This is collecting, storing, and testing the blood components and derivatives.
- There is a therapeutic use of blood components, plasma derivatives, and apheresis technology.
- It includes collecting, storing, and using hematopoietic and other blood-derived cells.
- Whole blood may be fractionated into:
- Packed RBCs.
- Platelets.
- Plasma products.
- Plasma after processing provides:
- Albumin.
- Blood coagulation factors concentrate.
- Immunoglobulin preparation.
What are the indications for blood cross-matching?
- Whole blood: The primary purpose of the crossmatch is to prevent a transfusion reaction.
- Crossmatch is done before the major surgery.
- Crossmatch is also done before an operation where blood is usually unnecessary, e.g., hysterectomy and cholecystectomy.
- Packed RBC transfusion:
- Anemia is when the hemoglobin is <7 G/dL or the hematocrit is <21% without cardiovascular function complications.
- Hb <10 g/dl and HcT <30% in patients with cardiovascular disease, sepsis, or hemoglobinopathy.
- Platelet transfusion:
- Prophylactically, in the case of platelet count <10,000/cmm in adults and <50,000/cmm in neonates.
- In case of bleeding when platelets are <30,000/cmm.
- In the case of postoperative bleeding, when the platelet count is <50,000/cmm.
- In the case of the post-cardiopulmonary bypass, when the platelets are <100,000/cmm.
- Fresh frozen plasma:
- When the INR ≥ 2, and in the case of bleeding.
- In the case of nose bleeds, when the INR is ≥ 6.
- In thrombotic thrombocytopenic purpura.
- Cryoprecipitate:
- In the case of dysfibrinogenemia.
- When the fibrinogen is <100 mg/dL.
- In the case of Von Willebrand disease.
What are the precautions for the selection of a donor (rejection of the donor)?
- Do not take blood from the donor if:
- Blood was donated in less than 8 weeks.
- Poor health, such as cancer, cardiopulmonary disease, and bleeding disorders.
- Pregnancy during and after 6 weeks of delivery.
- The blood pressure is more than 180/100.
- Pulse when 50/min or more than 100/min. The only exception is the athlete, where the pulse is usually slow.
- Hemoglobin is <12.5 g/dL or hematocrit <38%; such donors are rejected.
- History of infectious agents:
- The donor with a history of viral hepatitis, such as HBV, HCV, HIV, etc.
- The donor with Malaria or coming from a malarial area should avoid giving blood for three years.
- The person with a venereal disease should not give blood for at least one year (Syphilis or Gonorrhoea).
- A person who has received rubella or varicella vaccination should not donate blood for 4 weeks.
- The donor is running a fever > 99.5 °C.
- The donor has leukemia or lymphoma.
- The history of recent surgery or illness needs to be considered unfit. In case of illness, at least there should be a 2 to 3-week interval free of any signs/symptoms after the recovery.
- After the surgery, it depends on the type of surgery, and if he is under the supervision of a physician, it should be deferred.
- If the donor has a cold, influenza, or has undergone a tooth extraction, it should be deferred for one week.
- Donors with a history of allergies and allergies to drugs should be rejected.
- Donors on drug medication, like antihypertensive drugs, antibiotics, and corticosteroids, should be rejected.
- Donors who have received a recent vaccination should be deferred for at least one week.
- If there is H/O drug abuse.
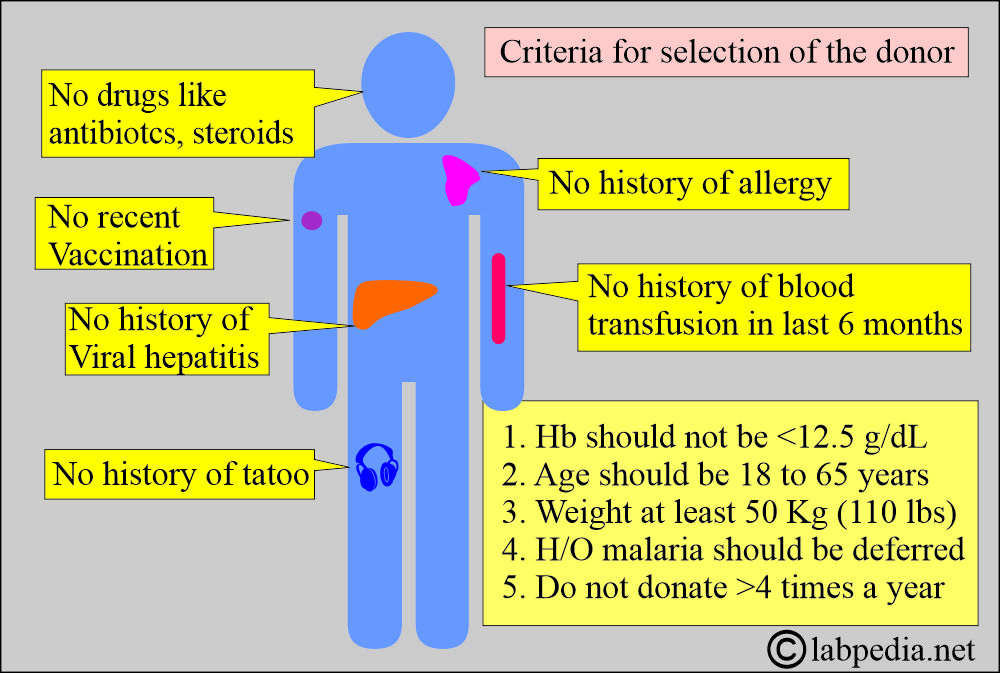
What are the criteria for the selection of a blood donor?
- History of the donor:
- There is no history of viral hepatitis in the last 6 months.
- No history of blood transfusion in the last 6 months.
- There should be no contact with the patient with viral hepatitis.
- Avoid drug addicts.
- No history of tattooing in the last 6 months.
- Avoid blood positive for HBV, HCV, or HIV.
- Hemoglobin should be at least 12.5 G/dL. This should be checked before taking the blood.
- Hct should be 38%, in the normal range.
- Age: The Ideal age is between 18 and 65 years.
- Bodyweight: The donor should weigh at least 50 kg (110 lbs).
- The temperature should not be >99.6 °C. The purpose of the temperature is to avoid the transfer of the infection to the recipient.
- The pulse rate should be 50 to 100 beats per minute. A pulse rate greater than 100/minute should be further evaluated.
- A pulse rate <50/minute may be found in the athlete.
- The donor may have anxiety, so allow him to relax for 10 to 15 minutes, then recheck the pulse.
- If still, the pulse is >100/minutes, then defer the donor.
- Blood pressure systolic should not be >180 mmHg, and diastolic should not be >100 mmHg. These donors need to be evaluated before they are accepted.
- History of recent immunization: Deferral of this donor for at least one week till they have no signs and symptoms.
- Check skin lesions in the antecubital area to rule out habitual drug abuse.
- These donors are deferred because of the risk of the Hepatitis virus or HIV infection.
- Check for psoriasis lesions, skin eruptions such as poison ivy, and rash.
- History of malaria: Such donors with a history of malaria should be deferred for at least three years. People who have traveled to malarial areas should also be deferred for three years.
- History of donation: Avoid professional donors because they often have low hemoglobin levels.
- The donor should not donate blood more than 4 times a year.
- Males should donate more than females.
- Sex: Females should donate less than males due to their menstrual cycle, during which they may lose approximately one point of blood annually.
- History of present or recent surgery or illness: Donors with long-standing illnesses should be excluded. Donors with a history of recent surgery or hospitalization should be rejected.
What should you note in the medical history of Donors?
- Have you ever had jaundice?
- Do you have H/O liver diseases?
- Do you have positive tests for viral hepatitis?
- Have you had blood donations in the last 12 months?
- Do you have an organ transplantation?
- Have you had acupuncture in the last 12 months?
- Do you have close contact with the patient having yellow jaundice or hepatitis?
- H/O of malaria or intake of malarial drugs in the past 3 years?
- Is there H/O cancer, blood disease, or bleeding problems?
How will you summarize the selection of the Donor?
- In general, the donor should be in good health.
- The oral temperature should not exceed 99.6 °C (37.5 °C).
- The pulse should be 50 to 100 beats per minute and should not exceed this limit. The pulse rate over 100/minute should be further evaluated.
- Age of the donor. Don’t take blood from old senior persons.
- Blood pressure should be systolic < 180 and diastolic < 100 mmHg.
- Weight of the donor. The ideal weight may be 110 lb (50 kg)
- Level of hemoglobin and Hematocrit (Hct). Hemoglobin at least 12.5 g/100 mL and Hct 38%.
- Frequency of blood donation per year.
How will you reject a donor based on their medical history?
- Infections of the donor include a history of viral infections, a history of malaria, or the use of antimalarial drugs, or a history of major surgery or illness.
- H/O psoriasis and its treatment.
- If there is H/O chest pain, heart disease, or lung disease.
- If there is H/O cancer, blood diseases, or bleeding disorders.
- If there are H/O convulsions, seizures, or fainting spells.
- If the donor has had a vaccination in the last 4 weeks.
- H/O extraction of teeth and dental works.
- Positive syphilis test in the last 12 months.
- If the positive test for AIDS.
What preservatives are used in blood banking?
| Preservatives name | Abbreviations used are | Storage time limit |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What are the criteria for allogeneic donors and autologous donors?
| Clinical parameter | Autologous donor | Allogenic donor |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What should be tested on Doner’s blood?
- ABO typing.
- Rh typing.
- Hepatitis B surface antigen.
- Hepatitis Core B antibody (HBc-IgM).
- Hepatitis C antibody.
- For Syphilis (VDRL).
- HIV.
- SGPT (ALT).
- If possible, do PCR for HCV and HIV.
How will you rule out infectious diseases?
- Must do to rule out:
- Serologic test for syphilis.
- Antibody to HCV (hepatitis C virus).
- HCV RNA.
- HBS antigen (hepatitis B surface antigen).
- Antibody to Core-antigen (antibody to HBV core antigen).
- Antibody to HIV-1 and HIV-2.
- HIV-1 RNA
- West Nile virus RNA
- Screening for bacterial infection can only be done on the platelet count.
- Optional and may be needed in some areas:
- CMV antibody.
- SGOT/SGPT for any abnormality in the liver.
- Sometimes this simple test helps to rule out hepatotropic virus infection.
What is the procedure for blood donation?
- Blood bags should not be released before it is tested for:
- Before issuing the blood bag for donation, all blood bags are tested as follows:
Advise forward blood grouping (Donor’s RBCs):
- ABO typing.
- Rh typing, including the weak D antigen in the case of D-negative individuals.
- All Rh0 (D) negative units are confirmed and tested with anti-CD and anti-DE.
- Du tests are performed on all r’ and r” units.
- Screening for non-ABO donor antibodies.
Advise reverse blood grouping (Donor’s serum):
- Antibody screening tests using enzyme and antiglobulin methods.
- Advise VDRL test for syphilis.
- Advise Hbs Ag and HbS Ab test.
Recipient blood screening includes:
- ABO typing.
- Rh typing.
Cross-Matching:
How will you discuss the history of blood cross-matching (compatibility testing)?
- This was introduced by Ottenberg in 1908; the direct compatibility test, or cross-match, between the donor and the recipient (patient), was crucial for the safe administration of blood transfusions.
- The direct cross-match was preceded by antibody screening for several decades as part of patients’ pretransfusion testing.
- In 1960, phenotyped RBCs were used for this purpose and were commercially available.
- In 1964, Grove-Rasmussen recommended the use of the antiglobulin test as part of the crossmatch when antibody testing was negative.
- The two main functions of the crossmatch are:
- This is a final check for the ABO compatibility between the patient and the donor.
- This may detect the antibody in the patient’s serum that was not detected in the antibody screening.
- Major crossmatch is much more important than minor crossmatch.
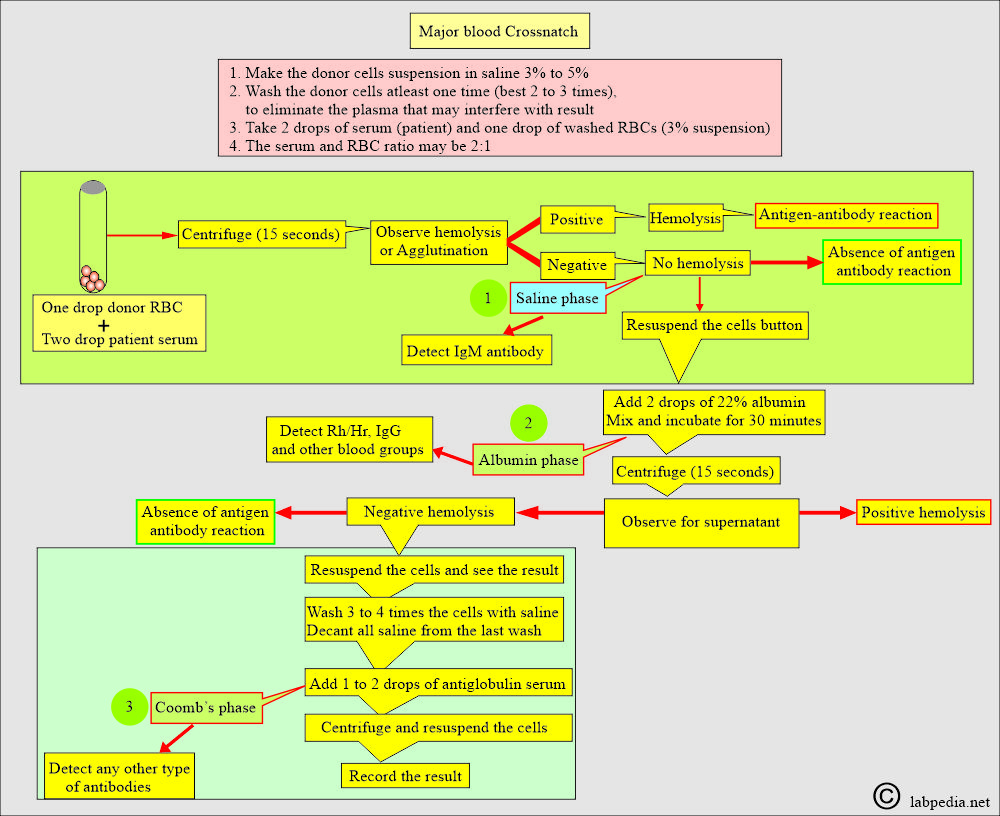
What is the procedure for blood cross-matching?
- Make the Donor’s RBC suspension in normal saline.
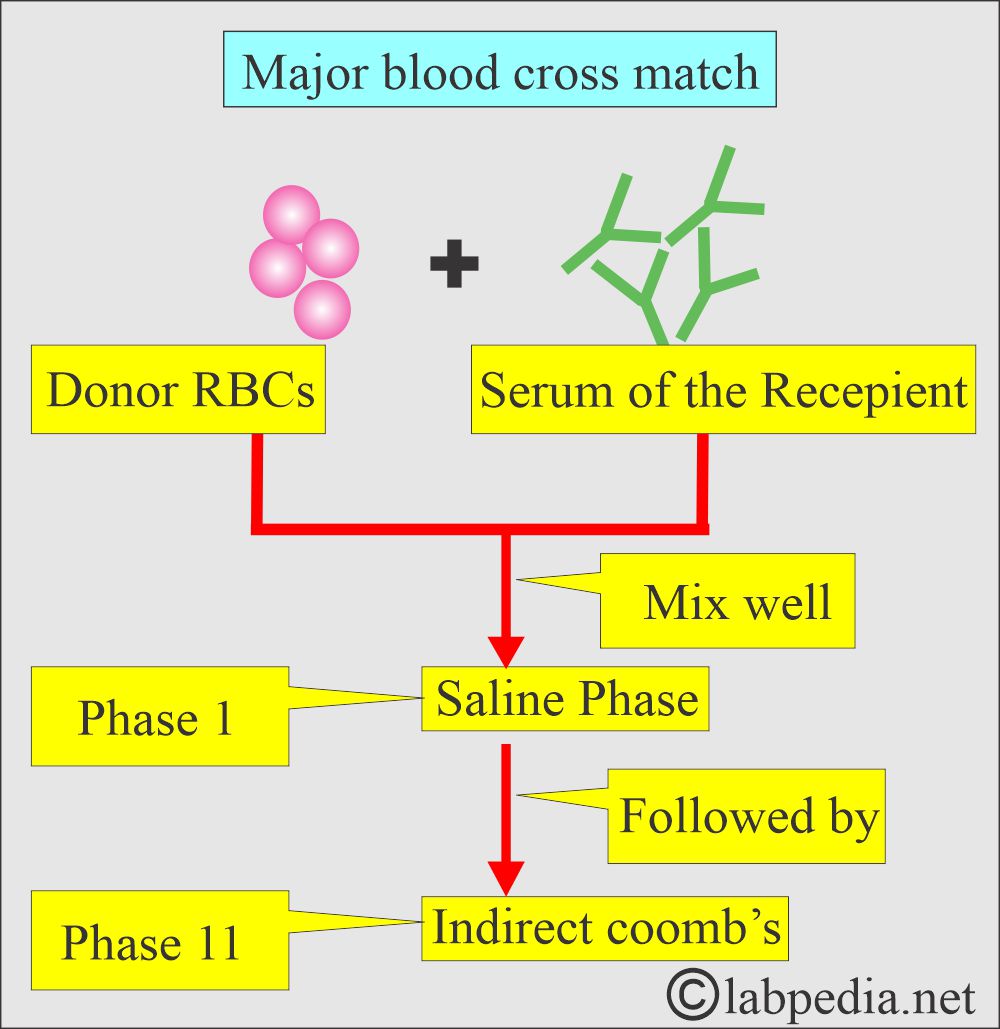
How will you perform the major blood cross-match?
- It is also called a direct cross-match.
- Donor RBC and recipient serum are mixed in the saline phase.
- This is followed by an indirect Coombs test, where the above RBC is washed with saline three times, and then Coombs’ serum is added.
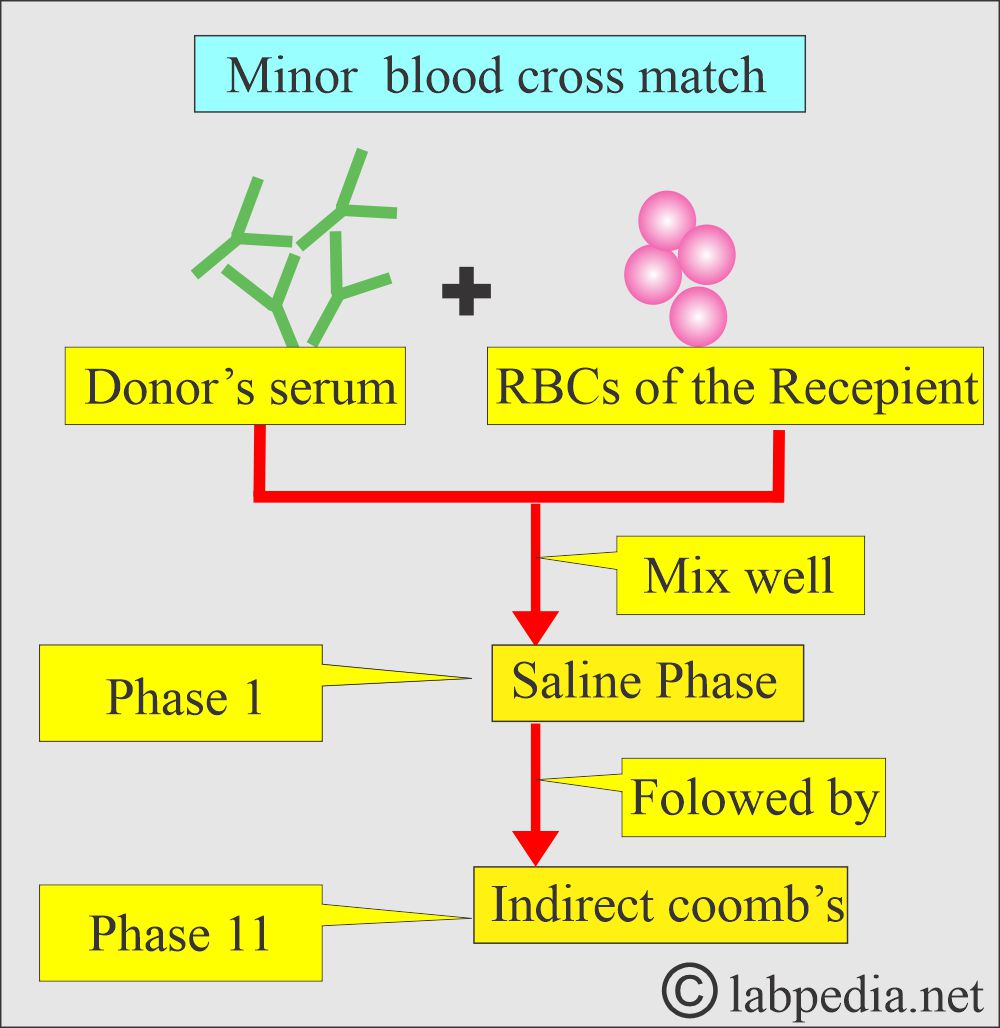
How will you perform the minor blood cross-match?
- It is also called the reverse cross-match.
- Now, take the recipient RBC and the donor serum.
How will you read the cross-match?
- Negative (can transfuse the blood), Compatible = No cell clumping or hemolysis should be seen (No agglutination should be observed).
- Positive (can not transfuse blood), Not compatible = Shows agglutination or hemolysis.
Discuss the ABO donor and recipient compatibility?
| Donor’s blood group | Antigen | Antibody | Recipient blood group |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Blood grouping and cross-match:
| Blood grouping and compatibility: | Donor blood group | ||||
| O (universal donor) | A | B | AB | ||
| Recipient blood groups |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(universal recipient) |
|
|
|
|
|
Question and answers:
Question 1: What is the major cross-match?
Question 2: What is minor cross-match?

thkyou a lot.
Thanks a lot.
Most relevant.
Thanks
Thanks.
Thank you so much.
Welcome.
What is the response of Reticulocytes to blood loss?
The reticulocyte is the single most useful test to detect the hemolytic state.
Reticulocytosis in a single episode of blood loss starts after 2 to 4 days, and the peak level is between 4 to 7 days. When hemoglobin becomes normal, then reticulocyte counts also become normal.
In the case of persistent reticulocytosis, a second rise in the reticulocyte count indicates a continuing or second episode of blood loss. In iron deficiency anemia or anemia due to blood loss, the reticulocytes will become normal in 4 to 7 days when the iron supplement is given.