Bence-Jones Proteinuria and Multiple Myeloma
Bence-Jones Proteinuria
What sample is needed for Bence-Jones Proteinuria?
- This test is performed on the patient’s urine.
- First morning sample: approximately 50 mL of uncontaminated urine in the container.
- To know the amount of Bence-Jones protein, 24-hour urine samples may be collected.
- A morning sample may be advised.
- If there is a delay, then refrigerate the sample.
What are the precautions for Bence-Jones Proteinuria?
- Avoid dilute urine.
- If there is a delay in the test, then refrigerate the sample.
- Avoid heat because heat-coagulable proteins can decompose, which will cause a positive result.
What are the indications for Bence-Jones Proteinuria?
- This will help in the diagnosis of Multiple Myeloma.
- It may be used to monitor the treatment of multiple myelomas.
- This may be seen in Waldenstrom’s Macroglobulinemia.
What is the history of Bence-Jones Proteinuria?
- In 1845, a patient was admitted to St.George’s Hospital in London (UK) with continuous back, chest, and pelvis pain.
- Dr. Henry Bence Jones tested the urine and found a substance after adding nitric acid.
- He called this substance Hydrated Deutoxide of albumin.
- Bence-Jones proteins, as described by Bence-Jones, were used in a heat test to detect light chains in the urine. Since then, they have been referred to as Bence-Jones proteins.
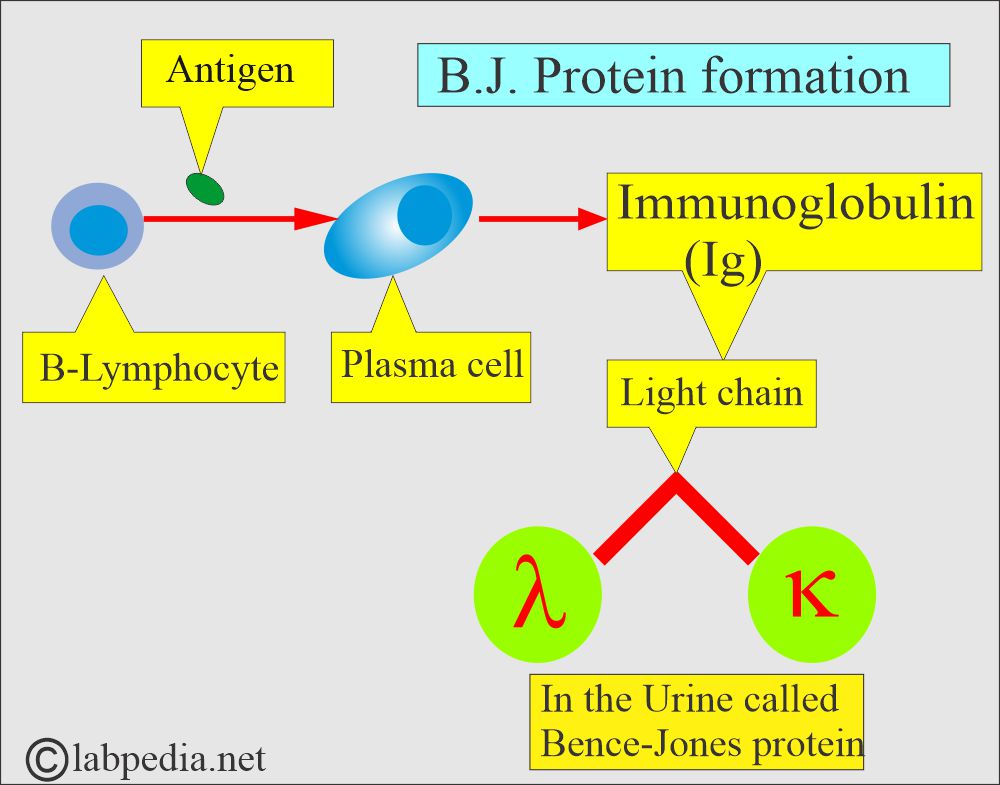
- Monoclonal immunoglobulin, which is also called paraprotein or myeloma components, may be:
- Polymer.
- Monomer.
- Or a fragment of an immunoglobulin molecule.
- If these are fragments, they are usually light chains, called Bence-Jones proteins, that appear in the urine.
How will you define Bence-Jones protein?
- This is an abnormal plasma or urine protein, consisting of monoclonal immunoglobulin light chains, excreted in neoplastic diseases and characterized by its unusual solubility properties as it precipitates at 50°C to 60°C and redissolves at 90°C to 100°C. When cooled, it then reappears again.
- There is the excretion of an abnormal light chain of immunoglobulins, kappa (κ) or lambda (λ), in the urine of Multiple Myeloma patients, which is called Bence-Jones protein.
- In about 10% of myeloma cases, B.J. protein is positive.
- B.J. protein is a single peptide chain with a molecular weight of 20,000.
- In the serum exists in two forms, κ and λ.
- These are abnormal light chain immunoglobulins secreted from the clonal proliferation of B lymphocytes.
- B.J. proteins are presented in two forms:
- Monoclonal gammopathy.
- As a free light chain disease.
What is the pathophysiology of Bence-Jones (BJ) proteins?
- These may be seen in tumor metastasis to bone, chronic lymphocytic leukemia, lymphoma, macroglobulinemia, and amyloidosis.
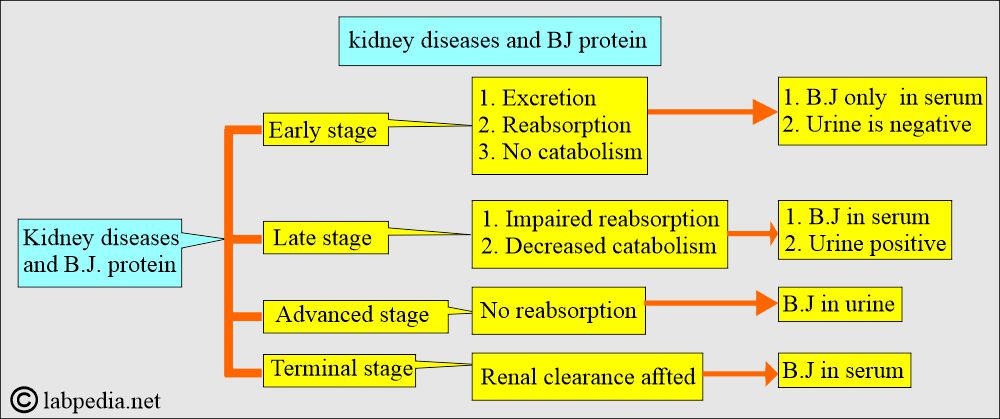
- B.J. proteins are very small in size, so they are easily filtered from the kidney glomeruli, can be detected in urine, and are difficult to find in the blood. So, the urine sample is used.
- Normally, BJ proteins are not found in the urine.
- B.J. protein present in serum, urine, or both depends upon the kidney function, like:
- Filtration.
- Reabsorption.
- Catabolism.
- Bence Jones protein is excreted in the urine:
- Around 70% (54% to 84%) of the multiple myeloma cases.
- 30% (0% to 78%) in Waldenstrom’s macroglobulinemia.
- Monoclonal gammopathy associated with lymphoproliferative malignancy yields a positive result in 20% (15% to 62%) of cases.
- In the case of benign secondary/idiopathic monoclonal gammopathy, it shows 10% (0% to 24%).
How will you summarize Bence-Jones proteinuria?
- It is used for the diagnosis of various types of gammopathies.
- This test is positive in 80% of the cases due to:
- Multiple myeloma (70% of all positive tests).
- Waldenstrom macroglobulinemia.
- Cryoglobulinemia.
- Benign monoclonal gammopathy.
- Adult Fanconi syndrome.
- Hyperparathyroidism.
- Primary amyloidosis.
Multiple myeloma
How will you define Multiple Myeloma?
- This is the malignancy of single clones of plasma cells. These plasma cells involve the bone marrow and frequently produce multisystem diseases.
- Plasma cells may form solitary nodules in the bone marrow, known as plasmacytoma.
- Osteolytic bone lesions will be produced.
- Other bone marrow cells, such as those affected, will lead to thrombocytopenia, leucopenia, and anemia.
What are the signs and symptoms of Multiple Myeloma?
- Age: Mostly, the patients are over 50 years of age. The peak age is 60 to 65 years.
- Sex: Approximately two-thirds of the cases involve males, which is observed in around 70% of the cases.
- The most important symptom is bone pain.
- These patients may have signs and symptoms of:
- Weight loss, weakness, and GI symptoms are found in 35% to 65% of the cases.
- Neurological signs are seen in 30% to 50% of the cases.
- Liver enlargement is seen in 20% of the cases, while splenomegaly is seen in 10%.
- Bone pain.
- Hypercalcemia: It is seen in 30% of the cases.
- Infections are seen in 10% to 50% of the cases. The common bacteria are encapsulated, like pneumococci. Other H. influenzae may also be seen.
- Pathological fractures are common.
- Markedly raised ESR.
- There is anemia.
- Frequent infections.
- Renal failure: Acute or chronic renal failure is seen in >50% of the cases.
What are the criteria for the diagnosis of multiple myeloma?
| Clinical criteria for the diagnosis | Signs/symptoms |
|
|
|
|
What is normal Bence-Jones (BJ protein)?
- Serum = Normally negative, B.J. protein is also negative in the urine.
- Qualitative urine = 0 in 50 x concentrated specimen.
- Quantitative urine :
- Kappa (κ) = <2.5 mg/dL.
- Lambda (λ) = <5.0 mg/dL.
How will you diagnose Multiple Myeloma?
- Anemia is seen in 60% to 80% of the cases. This is normocytic-normochromic anemia.
- There is increased rouleaux formation of the RBCs due to the presence of abnormal proteins. This picture can be seen in 60% to 85% of the cases and gives clues to the possibility of multiple myeloma.
- TLC shows leucopenia in 15% to 20% of the cases.
- In 1% to 2% of cases, plasma cells (>5%) may be seen in the peripheral blood smear.
- Some people say it is plasma cell leukemia, but others argue that this number should be greater than 20% plasma cells.
- Thrombocytopenia has been observed in around 10% of the cases.
- ESR is markedly raised in 90% of cases.
- Proteinuria is seen in 60% to 90% of the cases.
- Hypercalcemia is observed in approximately 30% of cases.
- Serum albumin levels are decreased in approximately 50% of patients.
- Hyperglobulinemia is seen in 60% (50% to 80%) of the patients.
- LDH level is raised in 20% to 40% of the cases.
- Radiological evidence has been found in 80% to 85% of the patients.
- The most typical lesion is a punched-out, osteolytic lesion.
- The common sites are the skull, vertebrae, spines, and pelvis.
- There are increased chances for a pathological fracture.
- The bone marrow aspirate shows more than 20% plasma cells.
- Sometimes, we may see 5% to 30% of plasma cells, along with the presence of a pathological fracture.
- If the plasma cells are <20%, then most plasma cells will show signs of immaturity.
- Bone marrow aspiration is diagnostic by the time S/S appears.
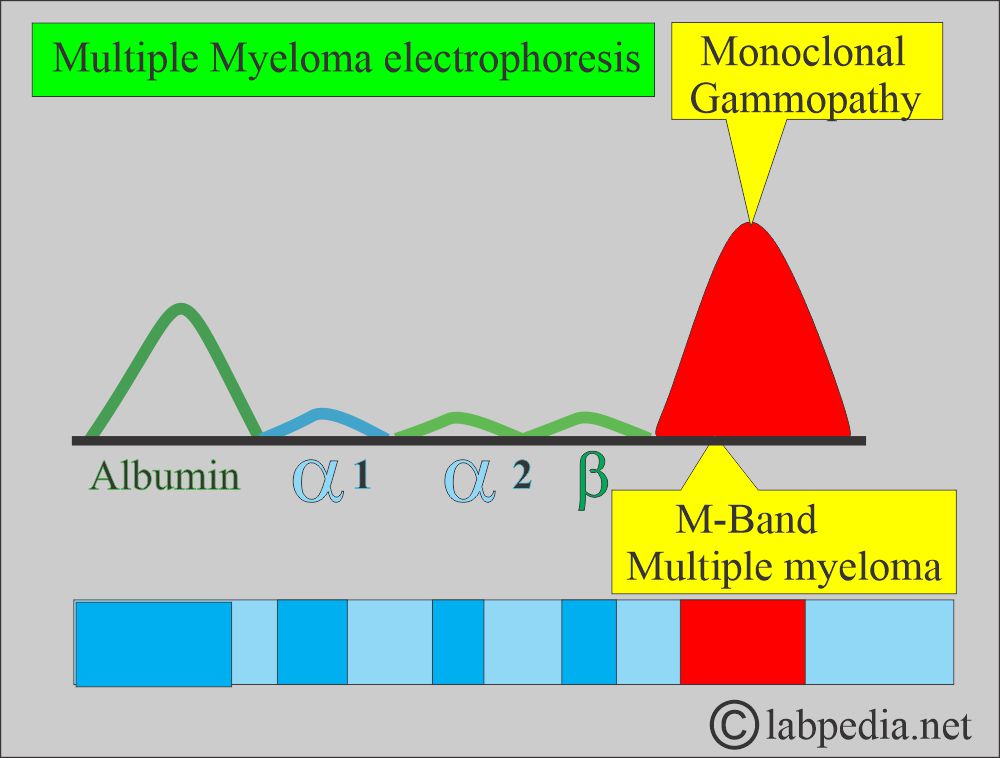
- Abnormal proteins, such as monoclonal immunoglobulins, are found in approximately 75% to 80% of myeloma patients, with a molecular weight of 160,000 daltons or 7S.
- These are usually present in the gamma-globulin area, occasionally in the beta-globulin, and rarely in alpha-2-globulin.
- Myeloma patients show monoclonal gammopathy where IgG is 70%, IgA is 25%, and <2% are IgD or IgE.
- Some of the patients’ secret, incomplete, and low-weight proteins are called Bence-Jones proteins.
- Bence-Jones protein consists of light chains (κ or λ) and has a molecular weight of 40,000 daltons or 3.5 S.
- Multiple myeloma shows:
- IgG = 60% (50% to 71%).
- IgA = 25% (22% to28%).
- Bence-Jones light chain = 20% (10% to 26%).
How will you perform Urine tests for light chains?
Heat test:
- The urine must first be acidified by adding I ml of 2 molar acetate buffer to 4 ml of filtered urine.
- Urine is concentrated 5 to 100 times to find the small amount of Bence Jones protein.
- These proteins (light chains of immunoglobulins) are soluble at room temperature.
- Precipitate at 60°C.
- Again, it disappears (redissolves) at boiling temperature or 80°C.
- These will reappear if the urine is cooled.
Protein precipitation test:
- The sulfosalicylic acid-positive test quantifies protein excreted in 24 hours of urine.
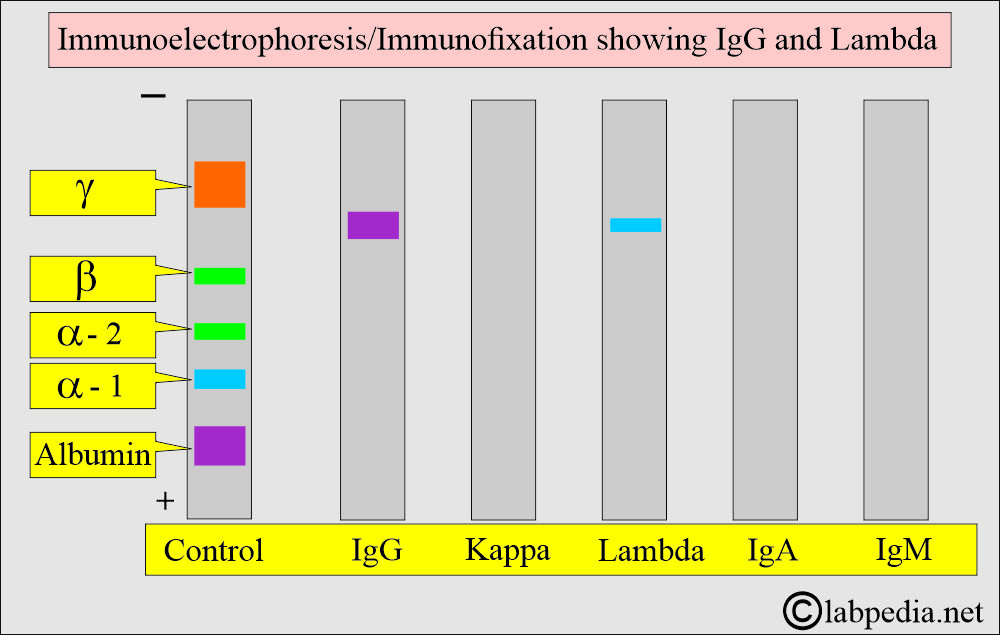
Immunoelectrophoresis:
- It is the definitive test differentiating Kappa and Lambda chains in the urine.
- This test may yield a negative result with the urine routine test strips.
Where will you find Bence-Jones (B.J.) Protein in various diseases?
- These are present in 75% of patients with multiple myeloma.
- Chronic lymphocytic leukemia.
- In Lymphoma.
- Amyloidosis.
- Waldenstrom macroglobulinemia.
- Monoclonal gammopathy of unknown significance.
- Tumor metastasis to the bone.
What are the causes of Bence-Jones proteinuria?
It indicates the various types of gammopathies. 80% of tests are positive in:
- Multiple myeloma (70% positivity).
- Waldenstrom macroglobulinemia.
- Primary amyloidosis.
- Cryoglobulinemia.
- Benign monoclonal gammopathy.
- Hyperparathyroidism.
- Adult Fanconi syndrome.
What are the causes of false positive tests (Roughly 20%)?
- Connective tissue diseases, such as rheumatoid arthritis, SLE, scleroderma, Wegener’s granulomatosis, and polymyositis.
- Chronic renal insufficiency.
- Lymphoma and leukemia.
- Metastatic carcinoma of the gastrointestinal tract and lungs.
- Presence of radiographic contrast material.
- High doses of penicillin and aminosalicylic acid.
- Dilute urine may give a false-negative result.
What is important for Bence-Jones proteinuria?
- In cases of positive Bence Jones (BJ) proteinuria, it should always be confirmed by electrophoresis and immunoelectrophoresis or immunofiltration of concentrated urine.
- A heat test is unreliable and should not be used to confirm the diagnosis.
- The reagent strips for the urine protein do not detect BJ protein.
Questions and answers:
Question 1: What could be a light chain in multiple myeloma?
Question 2: What is the role of Bence-Jones proteinuria?