Anti-thyroglobulin antibody (Thyroid autoantibody)
Anti-thyroglobulin antibody
What sample is needed for the Anti-thyroglobulin antibody?
- Collect 3 to 5 ml of blood and prepare serum.
- Keep the serum frozen if the test is not done on the same day.
- The fasting sample is preferred.
What Precautions will you take for Anti-thyroglobulin antibody?
- Stop multivitamins and any other medication that will interfere with the result.
- Oral contraceptives may increase their value.
- Older people, especially women, may have antithyroglobulin antibodies.
What are the Indications for Anti-thyroglobulin antibody?
- Useful for diagnosing thyroid diseases like Hashimoto’s thyroiditis and chronic lymphocytic thyroiditis.
- It differentiates Hashimoto’s thyroiditis and chronic lymphocytic thyroiditis in children.
- Hypothyroidism.
- Hyperthyroidism.
- Thyroid malignancies.
- In Graves’ disease (autoimmune hyperthyroidism).
- In Hashimoto’s thyroiditis (autoimmune hypothyroidism)
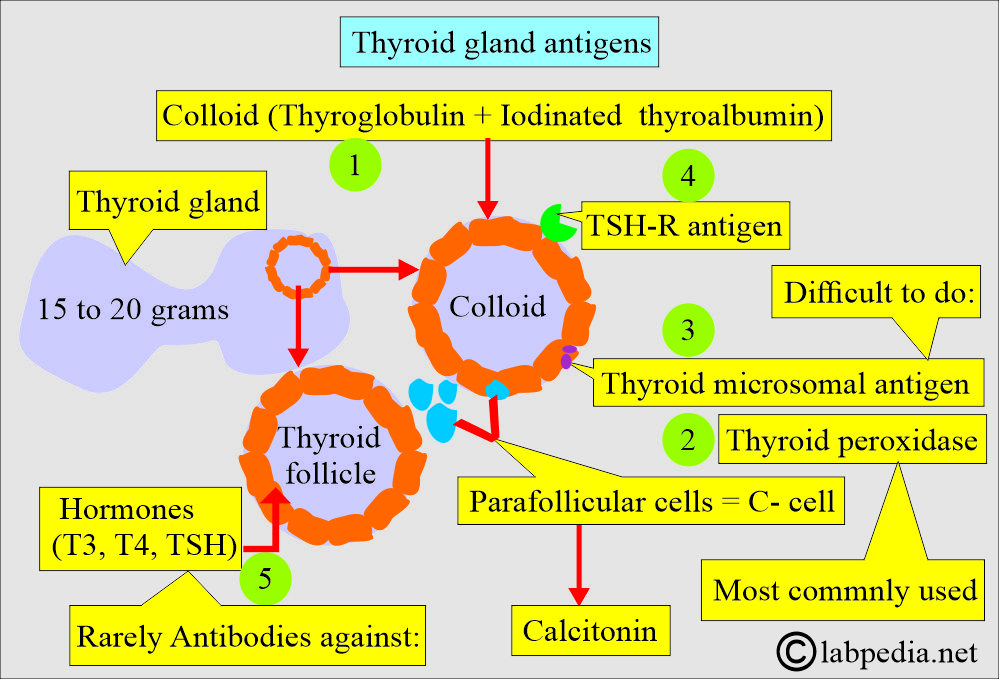
What are the Thyroid antigens?
- Several autoantibodies are organ-specific for the thyroid gland.
- The possible thyroid antigens giving rise to antibodies are:
- Hormone antigen.
- Thyroglobulin antigen.
- Thyroid microsomal antigen.
- Thyroid peroxidase antigen
- TSH-R antigen.
- Non-thyroglobulin colloidal antigen.
- Rarely can we measure:
- TSH antigen.
- T4 and T3 antigens.
- The physician most frequently orders anti-thyroglobulin and anti-thyroperoxidase.
- Anti-thyroglobulin antibodies are advised to evaluate:
- Hypothyroidism.
- Hyperthyroidism.
- Thyroid malignancies.
- In Graves’ disease (autoimmune hyperthyroidism).
- In Hashimoto’s thyroiditis (autoimmune hypothyroidism).
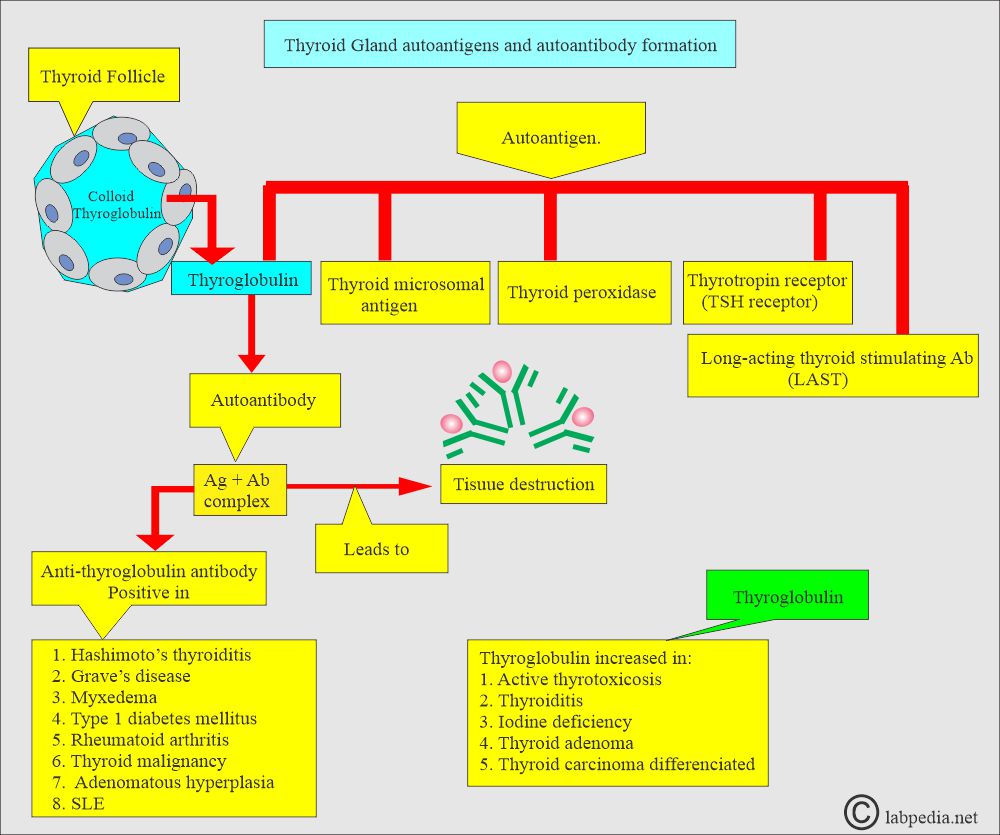
- This is an autoimmune phenomenon. An autoantibody against thyroglobulin is formed, called the anti-thyroglobulin antibody.
- Thyroperoxidase is mostly used for autoimmune thyroid diseases.
How will you discuss the Thyroglobulin?
- Thyroglobulin is also used as a tumor marker.
- 2/3 of the patients have preoperative raised levels of thyroglobulin.
- It is a 660 kD glycoprotein, a dimeric protein produced by the follicular cells, and is used entirely in the gland.
- This is the precursor of the thyroid hormone (thyroxine and triiodothyronine).
- Thyroglobulin combines with T4 by oxidation through peptide linkage.
- Thyroglobulin is synthesized in the follicular cells.
- There is a high concentration of thyroglobulin in the colloid inside the thyroid follicle.
- It enters the lumen of the follicle by the process of exocytosis.
- Circulating thyroglobulin’s half-life is about 65 hours.
- It takes nearly a month before thyroglobulin becomes undetectable after the total thyroidectomy.
- Thyroglobulin is cleared from blood circulation by catabolism in the liver and recycling in the thyroid.
- The thyroglobulin in the thyroid follicle can escape the follicle and become an antigen.
- Thyroperoxidase is located in the cytoplasm of the epithelial cells surrounding the follicles
What are the functions of autoantibodies against thyroglobulin?
- Anti-thyroglobulin antibodies exist in 10% of the normal population and >20% in thyroid cancer.
- These autoantibodies react with thyroglobulin and lead to thyroid destruction and inflammation.
- Anti-thyroid globulin antibodies can also be used to monitor residual disease (tumor recurrence).
- Increased levels of Anti-thyroid globulin antibodies may suggest a recurrence of the tumor.
- An increase in the anti-thyroglobulin antibody indicates antigenic stimulation, suggesting recurrence.
- If these antibodies are present in the mother, there is an increased risk of hypo- or hyperthyroidism in the fetus and the newborn.
What are the thyroid autoantibodies and thyroid diseases?
| Type of autoantibody | In the normal population | Autoimmune hypothyroidism | Grave’s disease |
|
|
|
|
|
|
|
|
|
|
80% to 99% |
|
What are other thyroid autoantibodies?
- Other thyroid autoantibodies form against microcosms and are called anti-microsomal antibodies; these are also used to diagnose thyroid diseases.
- The most commonly advised antibodies are thyroid peroxidase autoantibodies.
- Hashimoto’s thyroiditis is characterized by a high titer of anti-thyroglobulin and anti-microsomal antibodies, a level of >1:400.
- Thyroglobulin can be used as a tumor marker.
- 2/3 of the patients with thyroid cancer have raised levels of thyroglobulin.
- Anti-thyroglobulin antibodies can also be used to monitor the residual disease or to detect recurrence.
- An increased level of Anti-Thyroglobulin indicates the recurrence of the disease (cancer).
What are the antithyroglobulin antibodies in various diseases?
| Diseases | Antithyroglobulin Ab |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
When should you ask for an antithyroglobulin antibody test?
- If the patient has the following symptoms:
- If there is weight gain without any explanation.
- Patients have a history of fatigue.
- History of constipation.
- In the case of dry skin.
What is the normal level of antithyroglobulin antibody?
Source 2
- Negative = Titer = <1:100
- A small normal population may have an antithyroglobulin antibody.
- 5% to 10% of the normal population may show a low titer.
Source 4
- Anti-thyroglobulin = <1:100 (by haemagglutination).
- Negative by ELIZA.
- Negative by chemiluminescence.
- 10% of the population have low titer positive for the antibody without any symptoms of thyroid disease.
- This low titer is common in women and with increasing age.
- In some cases, this antibody production may be confined to the lymphocytes within the thyroid, resulting in negative serum tests.
How to measure anti-thyroglobulin antibodies?
There are different methods to detect anti-thyroglobulin antibodies, such as:
- Passive hemagglutination.
- The agar gel diffusion precipitation method.
- Immunofluorescence of the tissue biopsy.
- Enzyme-linked Immunoabsorbent assay (ELIZA).
- Chemilucent-based immunoassay.
What are the causes of increased Anti-thyroglobulin antibody levels?
- Chronic thyroiditis, like Hashimoto thyroiditis, in adults.
- The titer is high,>1:25,000, strongly suggesting Hashimoto’s disease.
- This autoantibody is positive in 50% of the cases of Hashimoto’s thyroiditis.
- The normal level of thyroglobulin antibody does not rule out Hashimoto’s disease.
- Chronic lymphocytic thyroiditis in children and young adults.
- Graves’ disease.
- Hypothyroidism.
- Atrophic thyroiditis.
- Thyroid cancer
- Thyrotoxicosis.
- Myxedema.
- Pernicious anemia.
- Sjögren’s syndrome.
- Lupus erythematosus.
How will you describe various thyroid diseases and autoantibodies?
| Disease | Anti-thyroglobulin antibody | Anti-microsomal antibody |
Antithyroperoxidase antibody |
Long-acting thyroid stimulating antibody (LATS) |
| Grave’s disease | positive 30% | positive 60 to 80% | positive >70% | positive 100% |
| Hashimoto’s thyroiditis | positive 70 to 90% | positive 80% | positive 100% | negative |
| Lymphocytic thyroiditis | positive 30 to 50% | positive 50% | positive | negative |
| Thyroid carcinoma | positive 20 to 50% | positive 15% | negative | |
| Normal person | positive low titer | positive 5 to 10% |
- LATS consists of two antibodies:
- TSI = Thyroid-stimulating immunoglobulin.
- TSH-R antibody = Thyroid hormone receptor antibody.
Questions and answers:
Question 2: Where are antithyroid peroxidase antibodies?