Anemia:- Part 5 A – Sickle Cell Anemia, Discussion and Workup
Sickle Cell Anemia
What sample is needed for Sickle Cell Anemia?
- Take EDTA blood for the sickling test.
- Make a fresh smear of the blood.
- Take blood samples for electrophoresis.
How can we make a good concept of sickle cell anemia?
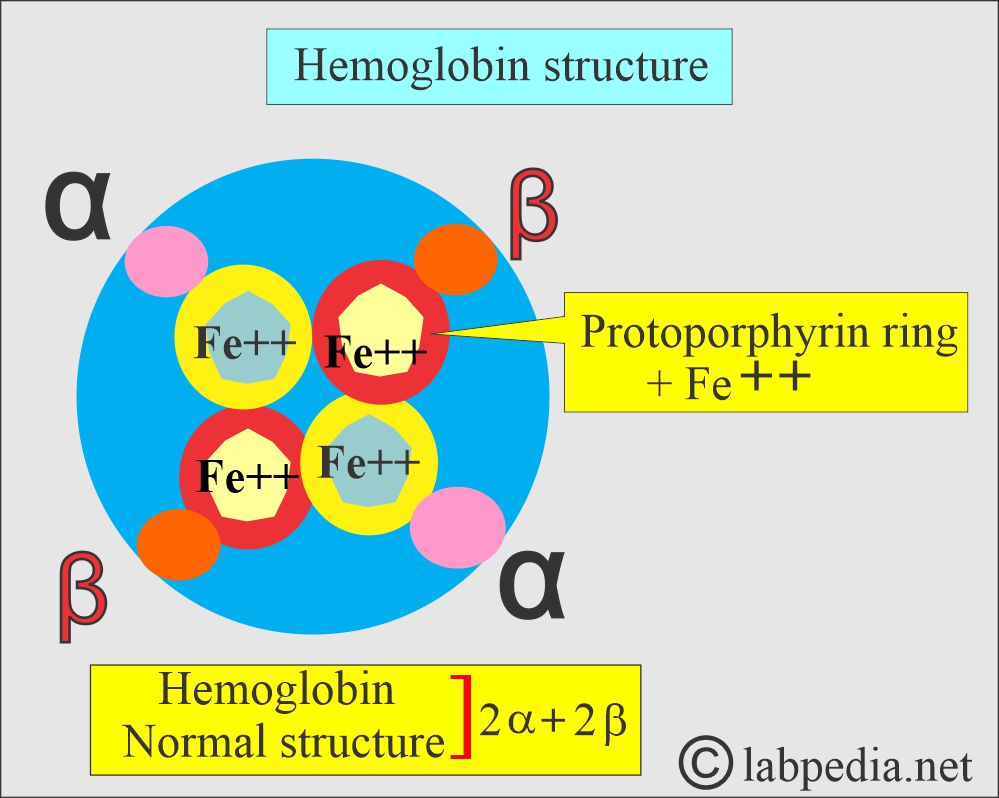
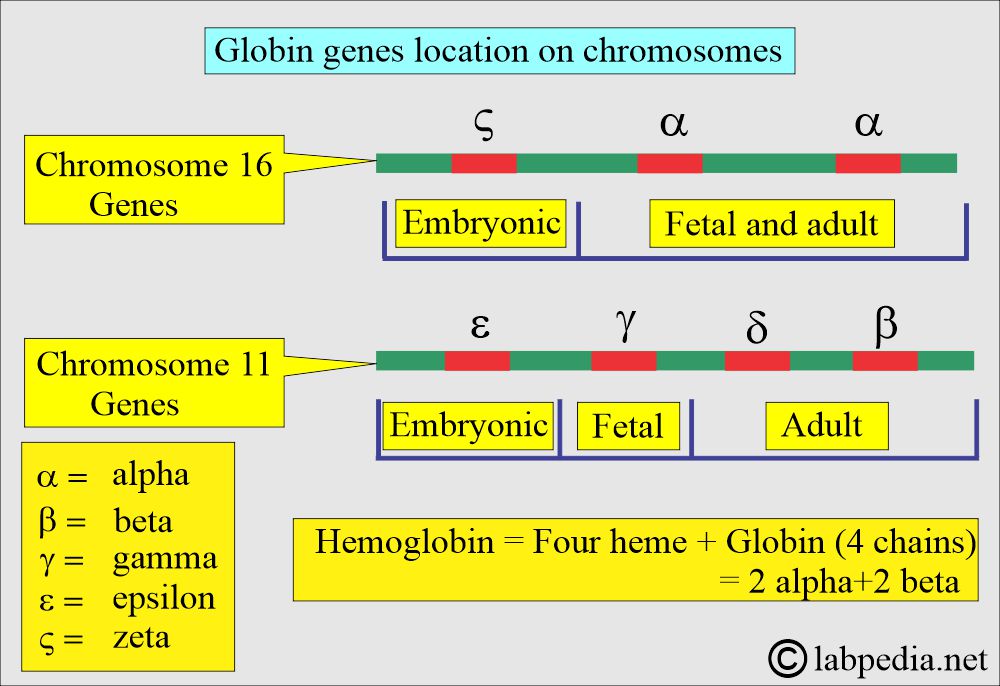
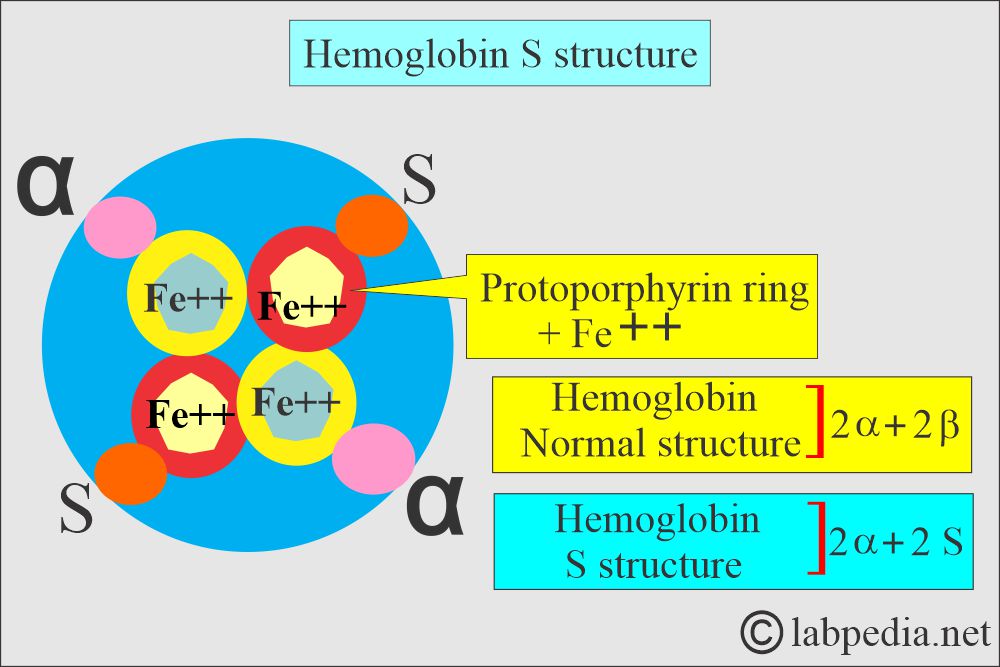
- The normal globin, part of the hemoglobin, consists of 2 alpha and 2 beta chains.
- The genetic code is located on chromosome 11, which are γ, δ, ε, and β-chains.
- While on chromosome 16, there are α and ζ loci.
What are the various types of hemoglobin?
| Type of hemoglobin | Genotype of hemoglobin | Functions of the hemoglobin |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Sickle cell syndrome:
What is the background of sickle cell disease?
- This condition was described in 1910 in Chicago in black patients.
- The carrier state in the USA is around 8%, while it is very high among blacks.
- This is also found in Mediterranean countries like Greece, Italy, Israel, Saudi Arabia, India, and Pakistan.
- The sickle cell gene has some advantages and protects from malaria infection (Plasmodium falciparum).
How would you define Sickle cell disease?
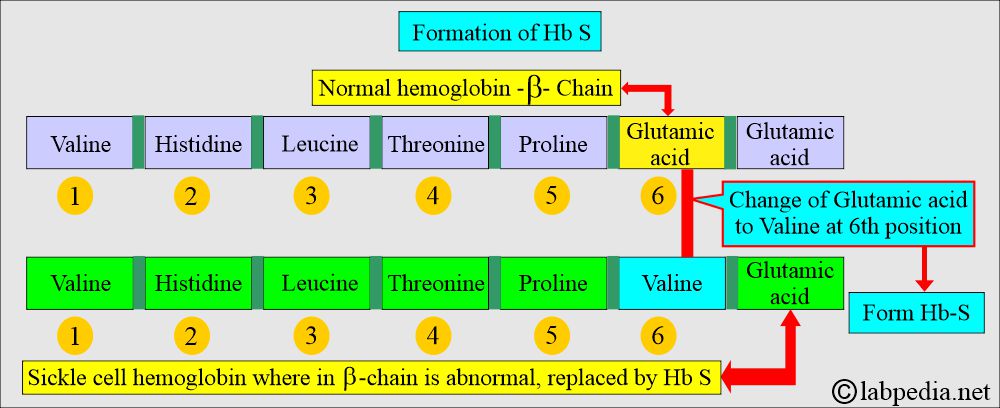
- Sickle cell disease occurs with the autosomal recessive inheritance of an abnormal β-chain of hemoglobin, where glutamic acid is replaced by valine. The end result is precipitation and polymerization of the Hb-S under conditions of deoxygenation and hypertonicity.
- A rigid crystal formation that deforms the RBCs is called sickling, leading to the occlusion of microvasculature and hemolysis.
- Sickle cell disease is defined as a condition where HbA is absent and only HbS is found. There is a homozygous expression of the S hemoglobin.
How would you define sickle cell anemia?
- In sickle cell anemia. Hemoglobin S agglutinates with deoxygenation and hypertonicity.
- In the case of homozygous disease (HbSS), sickling can occur at physiologic oxygen tension.
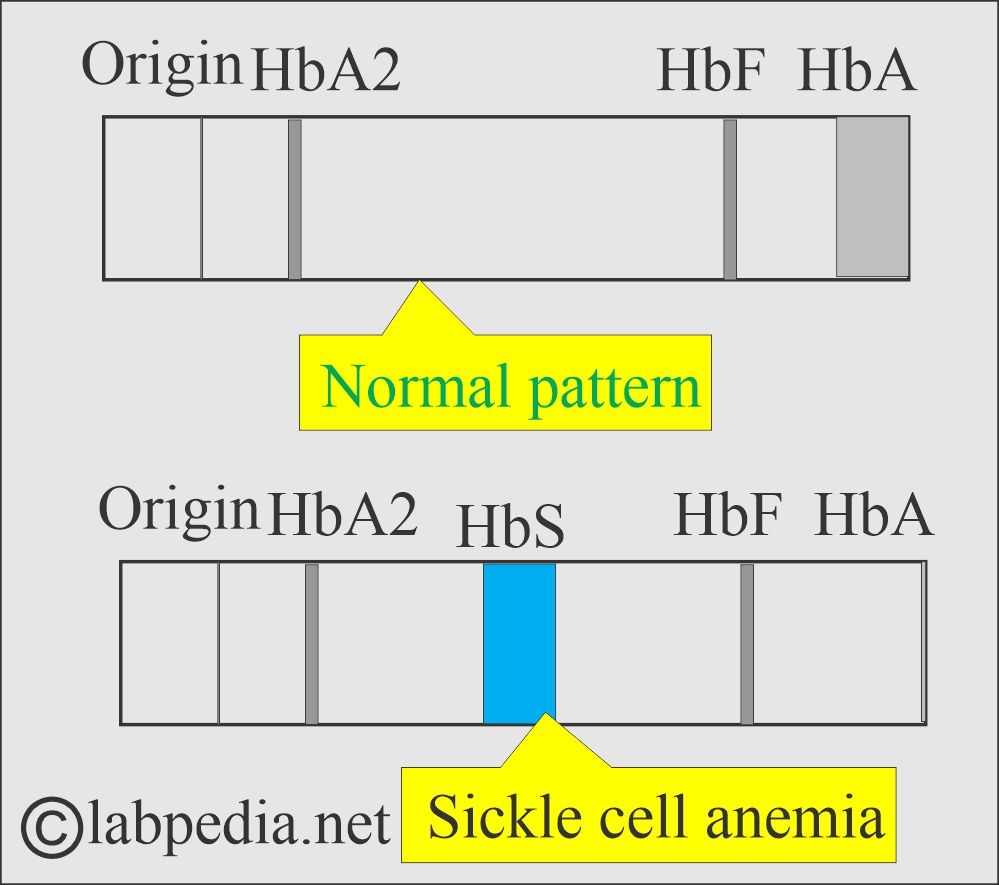
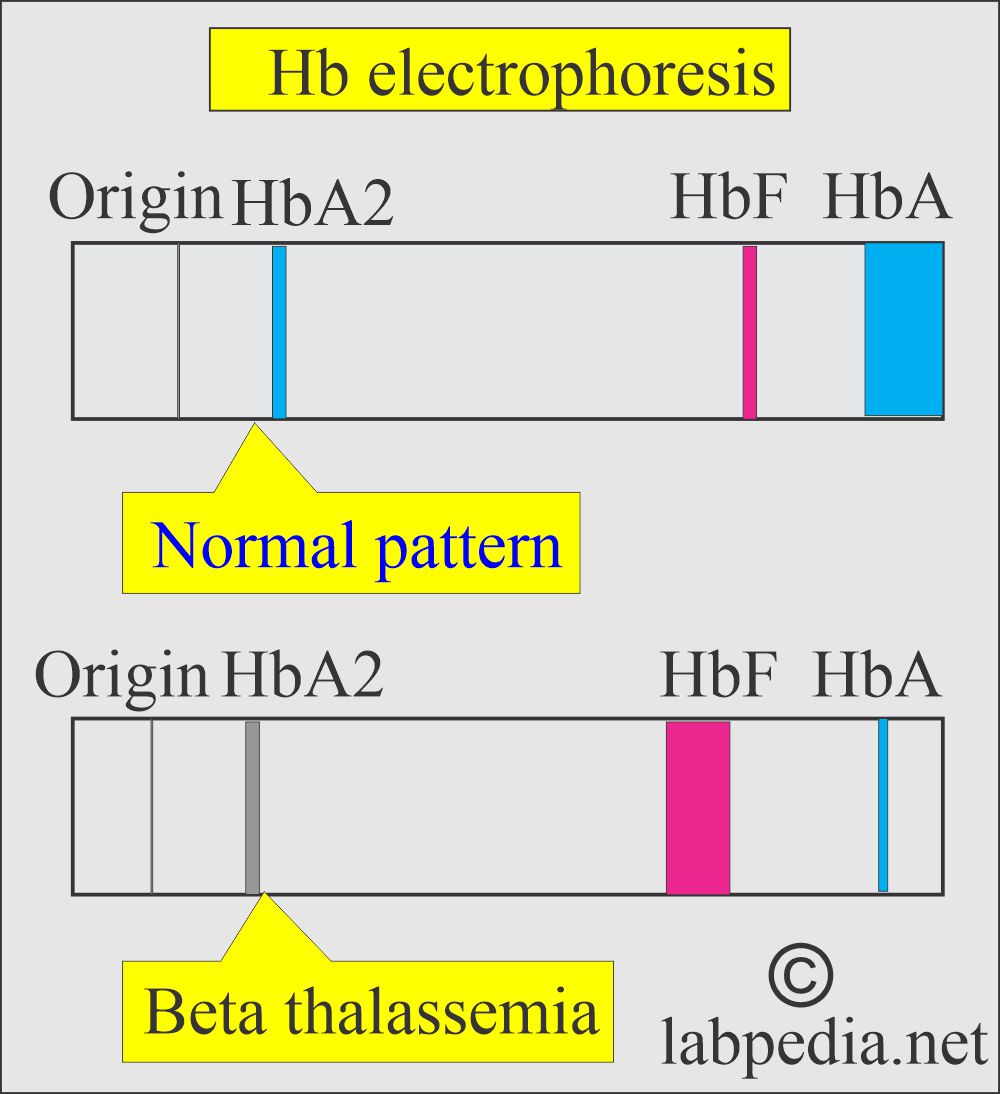
- On electrophoresis, Hb S is 80% to 100%. HbF is the rest, and there is no HbA.
What is Sickle Cell Disease?
- It includes all the hemoglobinopathies where HbS is present, e.g.:
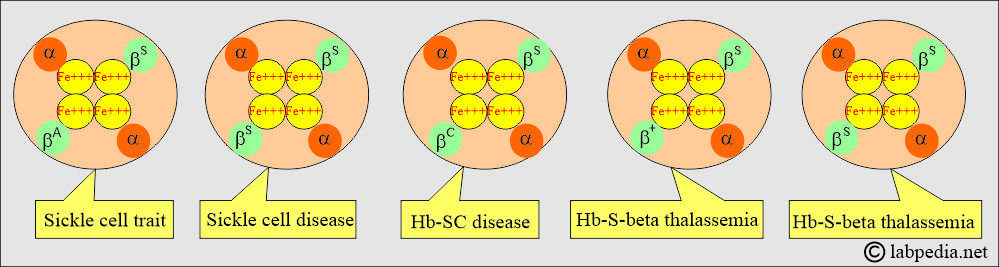
- Sickle cell trait: AS heterozygous (a combination of HbA+HbS = α2 βAβS).
- Hb A = ≅ 60% Hb S = 40%
- Sickle cell disease: SS homozygous (a combination of HbS+HbS = α2 βS βS).
- No HbA, Hb S = >80% Hb F = <1% to 20% Hb A2 = 1% to 4%.
- HbSC disease = α2 βS βC.
- HbS-beta thalassemia disease = α2 βS β0.
- HbS- beta thalassemia = α2 βS β+.
- Sickle cell trait: AS heterozygous (a combination of HbA+HbS = α2 βAβS).
What are the possible combinations of Sickle cell (HbS) disease?
What is the basic defect in Sickle cell anemia?
- The amino acid defect is in the β-chain at the 6th position, where the valine replaces the glutamic acid, giving the Hb a lower negative charge than HbA.
- This is the genetic mutation of Glutamic acid to valine.
- Sickle cell RBCs have been transformed into rigid, inflexible cells with at least one prominent projection.
How would you discuss Sickle cell trait (A/S)?
- This is a benign condition with no anemia and a normal RBC appearance on the blood smear.
- Hematuria is a common symptom and is thought to be due to small interactions in the kidneys.
- Sickle cell traits are usually asymptomatic.
- This is a heterozygous condition, Hb S (α2/β+βS).
- The peripheral blood smear shows normal CBC or mild normocytic or normochromic anemia.
- These patients are at risk of splenic infarcts at high altitudes.
- These patients also have the risk of renal medullary carcinoma.
- Peripheral blood smears also do not show sickle cells.
- Avoid or take care of anesthesia: pregnancy and high altitude.
- Electrophoresis shows:
- Hb S = 35% to 45%,
- Hb F = <1%
- Hb A2 = 1% to 3%
- Hb A = 50% to 55%.
How would you discuss the signs and symptoms of sickle cell disease (S/S)?
- This is a homozygous condition for Hb S (α2/2βS) disease.
- These patients have moderate to severe normochromic and normocytic anemia, and hemoglobin is 5 to 11 g/dL.
- Circulating nucleated RBCs are seen.
- Due to splenectomy, peripheral blood smears may show Howell-Jolly bodies and anisopoikilocytosis.
- Repeated attacks of spleen infarction (autosplenectomy) may occur.
- Indirect bilirubin is raised.
- Sickle cell preparation is positive.
- Electrophoresis shows:
- Hb S = >80%
- Hb F = <20%
- Hb A2 = 3% to 8%
- Hb A = absent
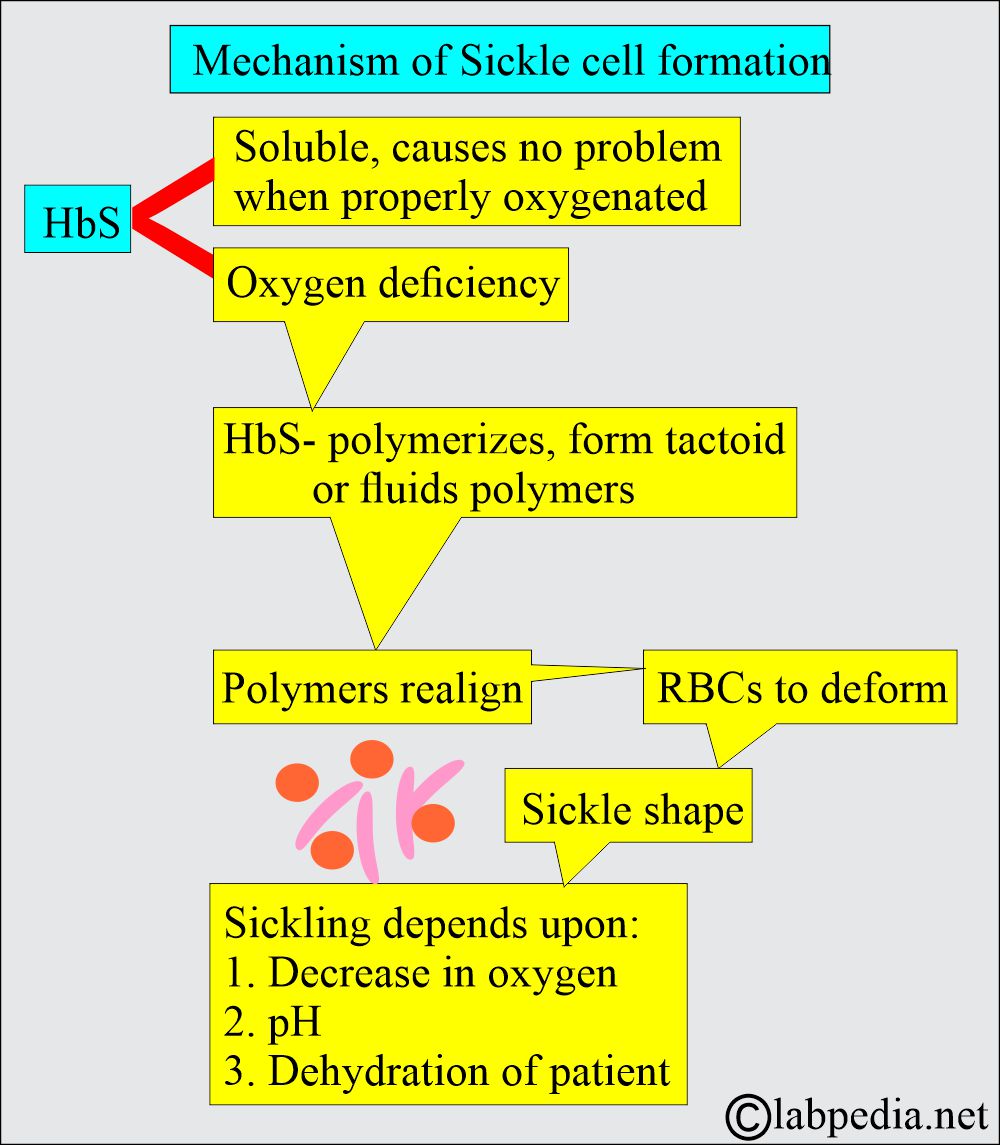
What is the mechanism of Sickling?
- HbS is soluble and usually causes no problems when properly oxygenated.
- Sickling depends upon the degree of oxygenation.
- When HbS is deoxygenated in vitro under near-physiological conditions, it becomes relatively insoluble compared to HbA and aggregates into long, rigid polymers called tactoids.
- Hb S, also called sickle hemoglobin, reacts to deoxygenation and dehydration by solidifying and stretching the RBCs into an elongated sickle shape, producing hemolytic anemia.
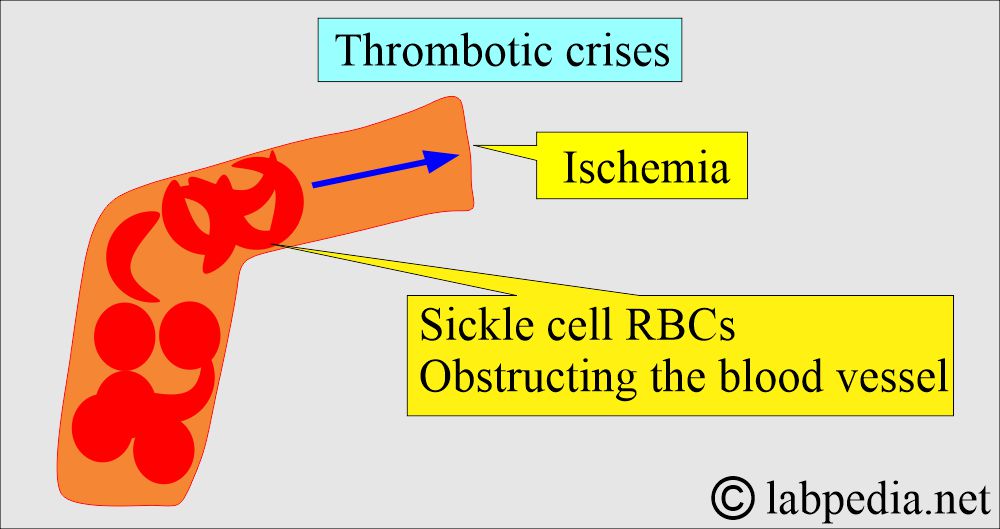
- These sickled RBCs settle in the small blood vessels, giving vaso-occlusive crises, such as abdominal crises, painful crises, and stroke.
- These cells have shortened the half-life of RBCs in the blood by an average of 17 days, whereas the normal half-life of RBCs is 120 days.
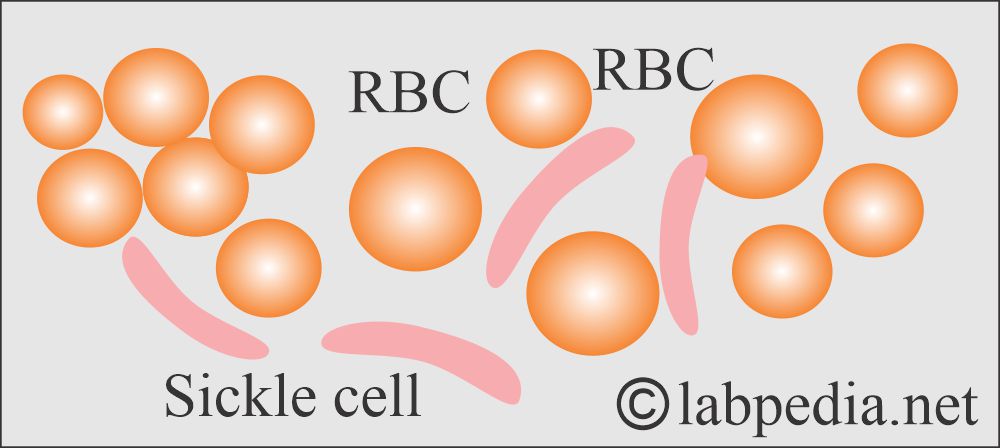
- These cells appear crescent in shape on a stained blood film.
- These cells return to their normal shape when they are oxygenated.
- After several sickling episodes, irreversible damage occurs to these RBCs; the macrophagic cells in the liver, spleen, or bone marrow phagocytose them, leading to anemia.
- This process of phagocytosis and hemolytic crises will depend upon the number of damaged RBCs in circulation.
- The rigid sickle RBCs cannot deform and circulate through the small capillaries, resulting in the blockage of these capillaries.
- This will lead to hypoxia and extreme pain and ultimately cause the death of the affected tissue. Infarction in the spleen is common.
- In this case, repeating this process in the spleen will lead to necrosis and scarring, and the result is a nonfunctional spleen called autosplenectomy.
How would you describe the clinical findings of sickle cell anemia?
- The clinical manifestation of sickle disease does not occur until the infant is 6 months old. At this point, Hb F decreases, and Hb S rises.
- When sickling takes place, which leads to hemolytic anemia, the patient will have the following:
- Pallor and fatigue.
- Jaundice.
- Irritability.
- In the case of acute crises, the patient will manifest a sickle crisis.
What are the Sickle cell crises?
| Organs involved | Clinical manifestations |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
How would you discuss the thrombotic crises (vasoactive changes) caused by the sickle cells?
- This will occur due to sickled cells’ obstruction of the microcirculation. There is thrombosis and infarction. Vasoactive crises are very painful and may last days or weeks, with an average duration of 4 to 6 days.
What are the Aplastic crises due to Sickle cells?
- These are due to decreased erythropoiesis instead of increased need because of hemolytic anemia. This is due to the short life of RBCs, which is just 10 to 20 days. Normally, compensatory erythropoiesis is 5 to 8 times normal. When this compensatory mechanism is compromised, aplastic crises develop.
What are the Pooling crises due to Sickle cells?
- These are due to a large pool of blood in the liver and spleen. This type of crisis is seen only in early life. The spleen can hold 1/5th of the body’s blood. There may be death due to cardiovascular collapse.
What are the Hemolytic crises due to Sickle cells?
- These are unusual but may occur with some drugs or infections.
What are the causes of Infections due to Sickle cells?
- It is the most common cause of death. Sepsis and meningitis develop in as many as 10% of children during the first 5 years of life, with a mortality rate of 25%.
- Survival is unpredictable, but many patients die in their twenties.
How would you discuss the signs and symptoms of sickle cell anemia?
- Anemia.
- Skin manifestations include leg ulcers.
- Arthritis.
- Renal diseases.
- Eye involvement.
- Bone marrow infarcts.
- Autosplenectomy.
- Hepatomegaly.
- Gall bladder stones.
- Priapism.
- GI tract symptoms.
What are the Long-term complications of sickle cell disease?
- There is an increased susceptibility to infection.
- The spleen may be completely infarcted.
- There are chronic leg ulcers.
- There are gallstones due to repeated hemolysis.
- There may be aseptic necrosis of the bone, particularly of the femoral heads.
- Chronic renal disease.
- There may be blindness due to retinal detachment or proliferative retinopathy.
- There may be an infarction of the lungs.
- Bone marrow necrosis may cause fat embolism syndrome.
What are the factors influencing the severity of Sickle cell anemia?
It depends upon various factors like:
- Amount of the Hb-S.
- It’s association with thalassemia.
- Influence of deoxygenation.
- Presence of an amount of Hb-F.
- If it is associated with G6PD deficiency.
- There is an effect of the temperature.
- There is the effect of dehydration.
- It depends on MCHC.
- Vascular stasis also influences sickle cell disease.
- There is a role for the pH of the body.
How will you diagnose sickle cell anemia?
- Low hemoglobin (7 to 9 G/dL).
- The peripheral blood smear shows sickled RBCs.
- How will you make the Sickle cell preparation?
- Procedure No. 1:
- Take one drop of blood on the slide.
- Put the cover glass and seal the edges with paraffin.
- Characteristic sickling may be seen in 6 hours or earlier.
- This may not be seen after 24 hours.
- Procedure No. 2:
- Add the reducing substance sodium metabisulfite 2%.
- Metabisulfite is mixed with the blood.
- After mixing it with the blood, cover it with a cover glass.
- Now, seal the edges with paraffin.
- The result may be readable in 15 to 60 minutes.
- Procedure No. 3:
- There are commercially available kits based on immunoassays.
- There are antibodies specific for the Hb-S.
- This method is very sensitive for newborn screening.
- This method has no interference from the Hb-F or Hct.
- Peripheral blood smears show:
- There are marked poikilocytosis and inclusion bodies.
- Sickle cell 6% to 18% may be seen on the peripheral blood smear.
- Platelets are increased.
- Reticulocytes are 10% to 20%.
- ESR is very low.
- Bone marrow shows marked erythroid hyperplasia.
- An iron stain shows low deposits of iron.
- Bilirubin is increased.
- Serum iron is increased.
- TIBC is normal.
- % saturation is normal.
- RBC survival is decreased.
- Electrophoresis of blood shows Hb S and no normal Hb A.
- This is the definitive method for diagnosis.
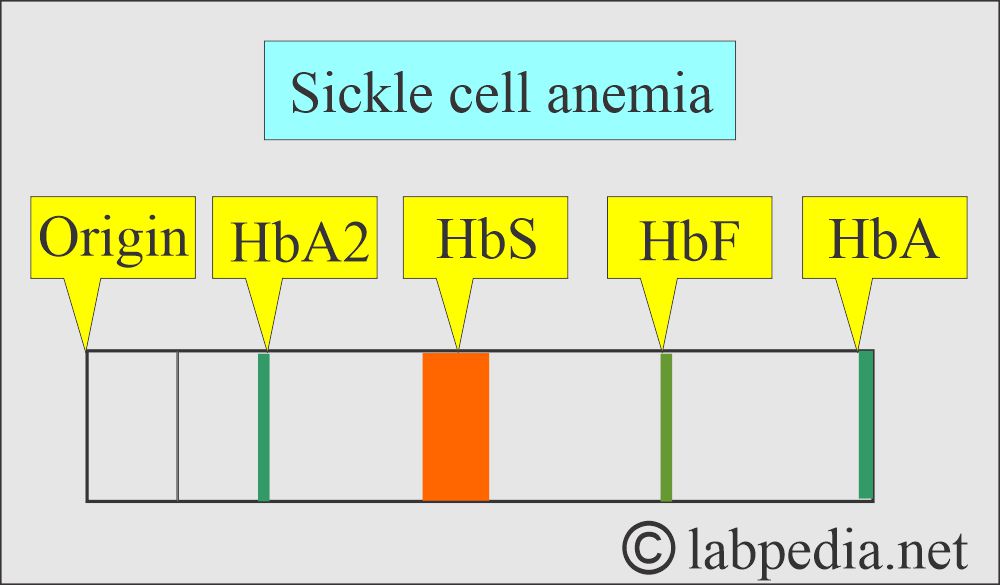
Hb S electrophoresis
- The parents of sickle cell disease patients will show features of the sickle cell trait.
What are the laboratory findings on sickle cell anemia?
| Type of anemia | Hemoglobin | Hct | Reticulocytes | MCV | Hb electrophoresis | RBC morphology | The severity of the disease |
| Sickle cell trait (α2/β+βs) | Usually normal | Usually normal | Normal | Usually normal |
|
Normal | Mostly asymptomatic |
|
Sickle cell disease (α2/βsβs) |
6 to 9 g/dL | 18 to 30 fl | 4 to 30% | 93 |
|
|
It is moderate to severe |
How will you treat Sickle cell anemia?
- Prophylaxis:
- Avoid those factors known to precipitate crises, especially dehydration, anoxia, infections, circulation stasis, and skin surface cooling.
- Folic acid 5 mg once weekly should be given.
- Patients should have good general nutrition and hygiene.
- Sickle cell trait does not affect life unless severe hypoxia is caused by shock, vigorous exercise, high altitude, and anesthesia, leading to vasooclusive episodes.
- Sickle cell disease needs supportive treatment for hemolytic anemia and to avoid crises.
- In the case of crises:
- Treat by rest, warmth, rehydration by oral fluids, or I/V normal saline. Can give 3 L in 24 hours.
- Antibiotics are given in case of infection.
- Analgesic is given in case of need, paracetamol, non-steroidal anti-inflammatory agents, and opiates.
- Blood transfusion is given in case of anemia.
- Stem cell transplantation can cure the disease; many patients are successfully treated.
Questions and answers:
Question 1: How much is Hb S in sickle cell disease?
Question 2: What is the most common complication of sickle cell anemia?

Excellent information. I wish you had a section about Sickle Cell S/C.
Thanks for the comments. I will try to discuss that topic also.