Anemia:- Part 1 – Anemia Classification, Diagnosis, and Routine Work up
Anemia
What sample is needed for an Anemia workup?
- EDTA blood is needed.
- For RBC morphology, a direct smear is preferred.`
- Bone marrow is also advised.
- Also, a bone biopsy may be needed.
How will you define Anemia?
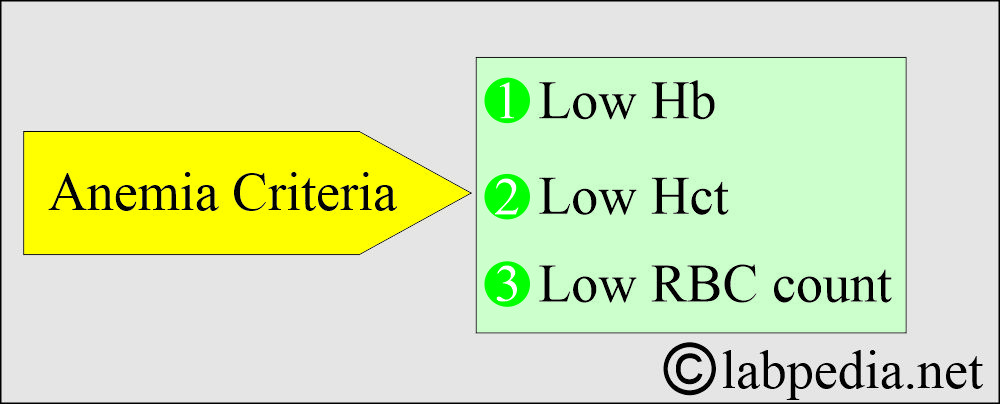
- Anemia is a decrease in hemoglobin concentration depending on the patient’s age and sex.
- The diagnostic criteria are low hemoglobin, hematocrit (Hct), or decreased RBC count.
What are the criteria for anemia?
- Hemoglobin:
- Male = Hb <13.5 g/dL.
- Female = Hb 11.5 g/dL.
- 2 years to puberty = 11.0 g/dL.
- A Newborn = 14.0 g/dL is a lower limit because of the high Hb.
- Hematocrit (Hct)
- Male = <42%.
- Female = <37%.
- In a broad sense, anemia is the inability of the blood to supply adequate O2 to the tissues for proper metabolism.
- These are the most common hematological disorders.
- Diagnosis is essential for the physician in treating the cause of anemia.
What are the factors for effective erythropoiesis?
- Level of iron and cobalt.
- Vitamin B12.
- Vitamin B6.
- Riboflavin.
- Thiamine.
- Vitamin C.
- Vitamin E.
- Hormones like:
- Androgens.
- Thyroxine.
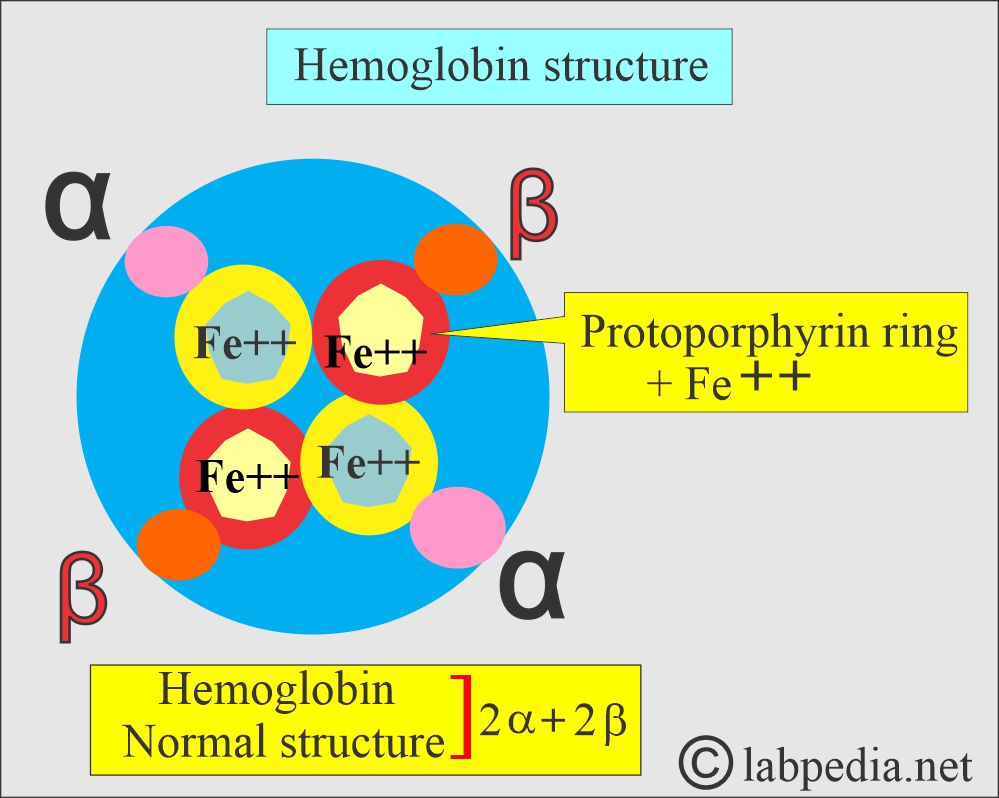
What are the types of Hemoglobin?
- To understand the anemias, it is better to know the hemoglobin types and structure:
| Type of hemoglobin | Structure of hemoglobin | Frequency of the hemoglobin |
| At birth | ||
| Hb F | α2 / γ2 | 60% to 90% |
| Hb A | α2 / β2 | 10% to 40% |
| At adult age | ||
| Hb A1 |
α2 / β2 | >95% |
| Hb A2 |
α2 / δ2 | <3.5% |
| Hb F |
α2 / γ2 | <1% to 2% |
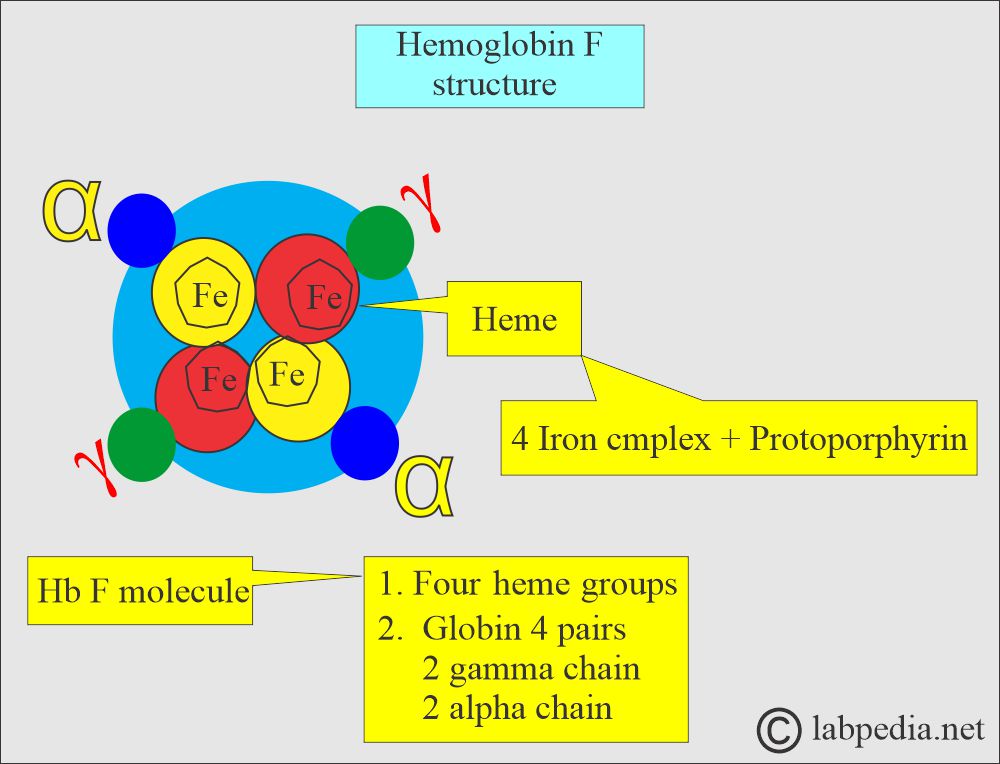
Hb F structure
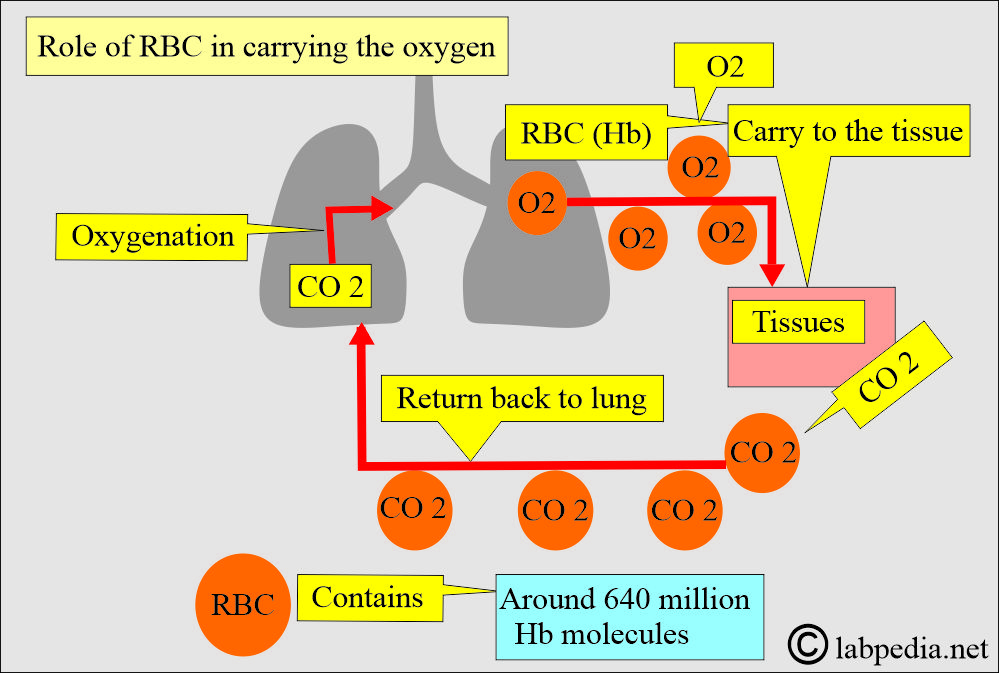
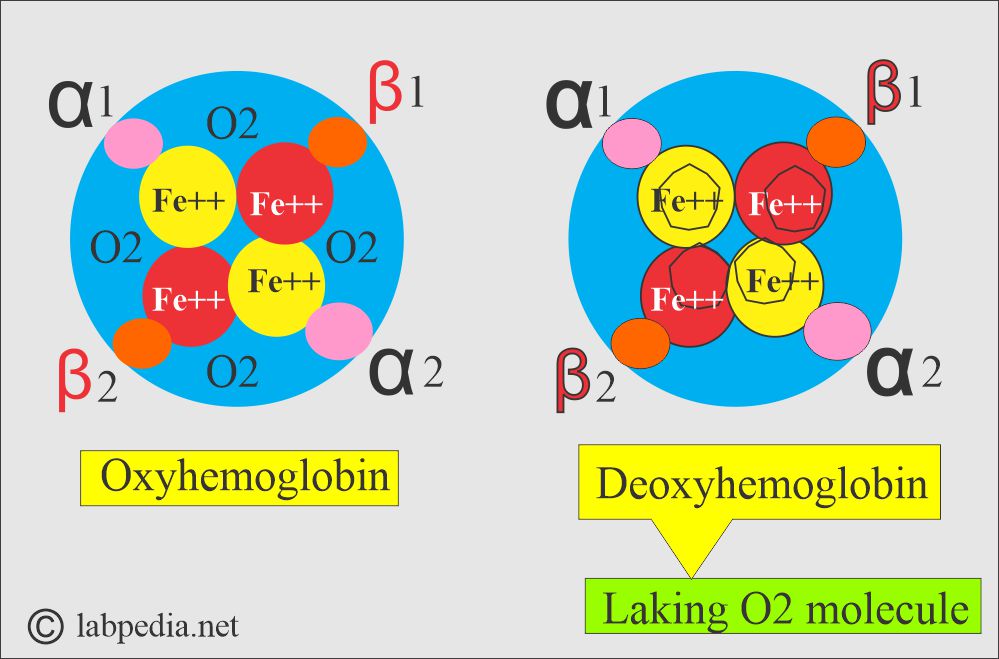
What is the role of hemoglobin in O2 transport (Hb/O2 dissociation curve)?
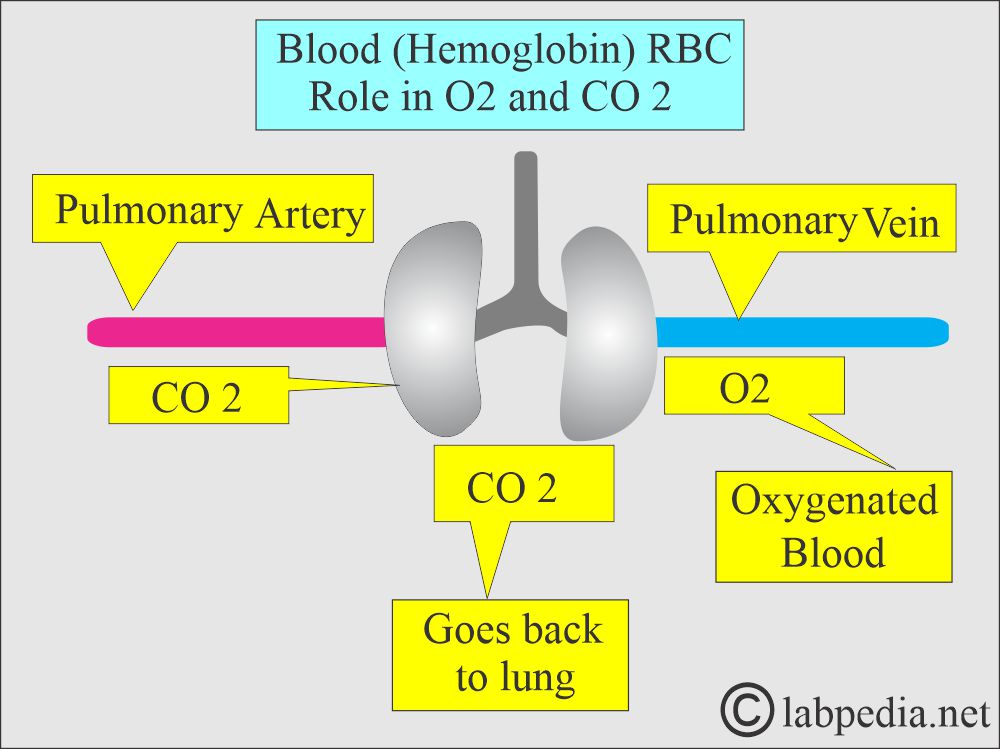
- The RBCs carry O2 from the lungs to the tissues and bring CO2 in the venous blood to the lungs.
- This is dependent upon the 2,3-diphosphoglycerate (2,3-DPG).
- When O2 is unloaded, the β-chain of Hb pulls apart, permitting the entry of the metabolite 2,3-DPG, which results in a lower molecular affinity for O2.
- O2 saturation is an indicator of the % of Hb saturated with O2.
- When 92% to 100% of the Hb carries O2, the tissues adequately provide the O2 supply, which means normal O2 dissociation.
- Normally, O2 exchange takes place:
- 95% saturated arterial blood with a mean arterial O2 tension of 95 mmHg.
- 70% saturated venous blood with a mean venous O2 tension of 40 mmHg.
- The curve’s normal position depends upon the concentration of 2,3-DPG, H+ ions, and CO2 in the RBCs and the structure of the Hb molecule.
What are the functions of Hemoglobin?
- RBCs in arterial blood carry O2 from the lungs to the tissues and take back CO2 in the venous blood.
- The main function is with the help of hemoglobin (Hb) molecules, as the Hb molecule loads and unloads the O2.
- α1β1 and α2β2 globin stabilize the molecule.
How will you classify Anemia?
Anemia may be classified roughly based on Hb level:
- Severe anemia when the Hb is <7 g/dL.
- Moderate when the Hb is 7 to 10 g/dL. This group will not produce evident S/S. in most cases.
How will you classify Anemia based on RBC morphology?
- Normochromic and normocytic anemias are due to:
- Anemia of acute hemorrhage.
- Hemolytic anemia.
- Anemia due to chronic diseases.
- Hypochromic and microcytic anemias are due to:
- Iron deficiency anemia.
- Thalassemia.
- Normochromic and macrocytic anemias are due to:
- Vit. B12 deficiency.
- Folate deficiency.
- Normochromic and macrocytic anemia is a late vitamin B12 and folate deficiency.
How will you classify anemia based on physiologic abnormality?
- Defective maturation of erythropoiesis.
- Hemolytic anemia is where the increased breakdown of the RBCs occurs.
- The defect is due to increased RBC precursors compared to the degree of anemia.
How will you classify the anemia based on etiology?
- Increased RBC destruction due to intra or extra-red blood cell defects.
- Increased blood loss, which may be acute or chronic.
- Defective RBC formation due to a lack of factors necessary for erythropoiesis.
How will you classify Anemia based on the category?
- Increased destruction of the RBCs
- Hemolytic anemia (nonimmune).
- Immune hemolytic anemia.
- Anemia due to blood loss in hemorrhage.
- Nutritional deficiency, such as folate or vitamin B12 deficiency.
- Toxicity due to drugs.
- Infections.
- Infiltration of the bone marrow by the cancer cells.
- Hereditary or acquired defect in the RBCs.
- Hematopoietic stem cell arrest or damage.
- Idiopathic or unknown cause.
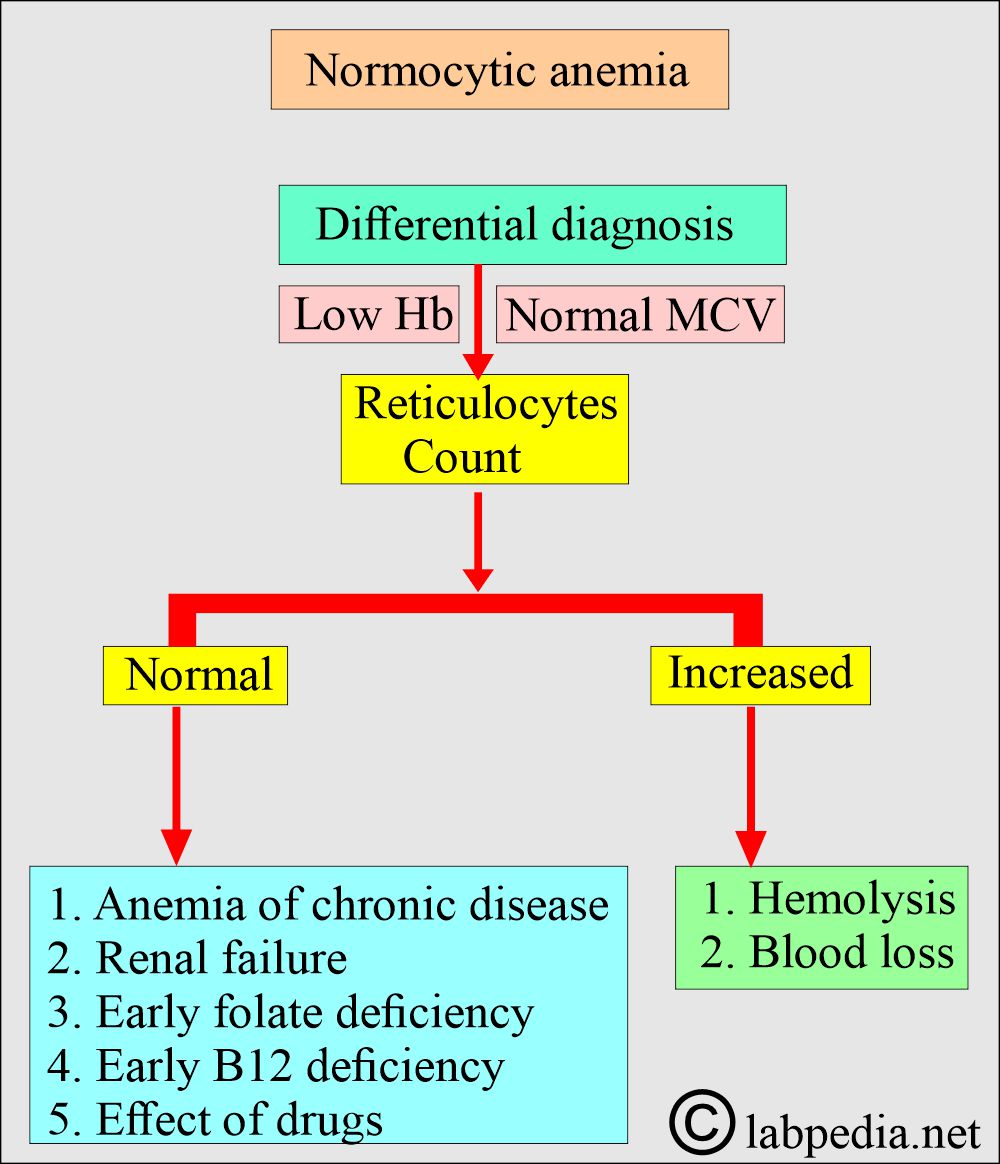
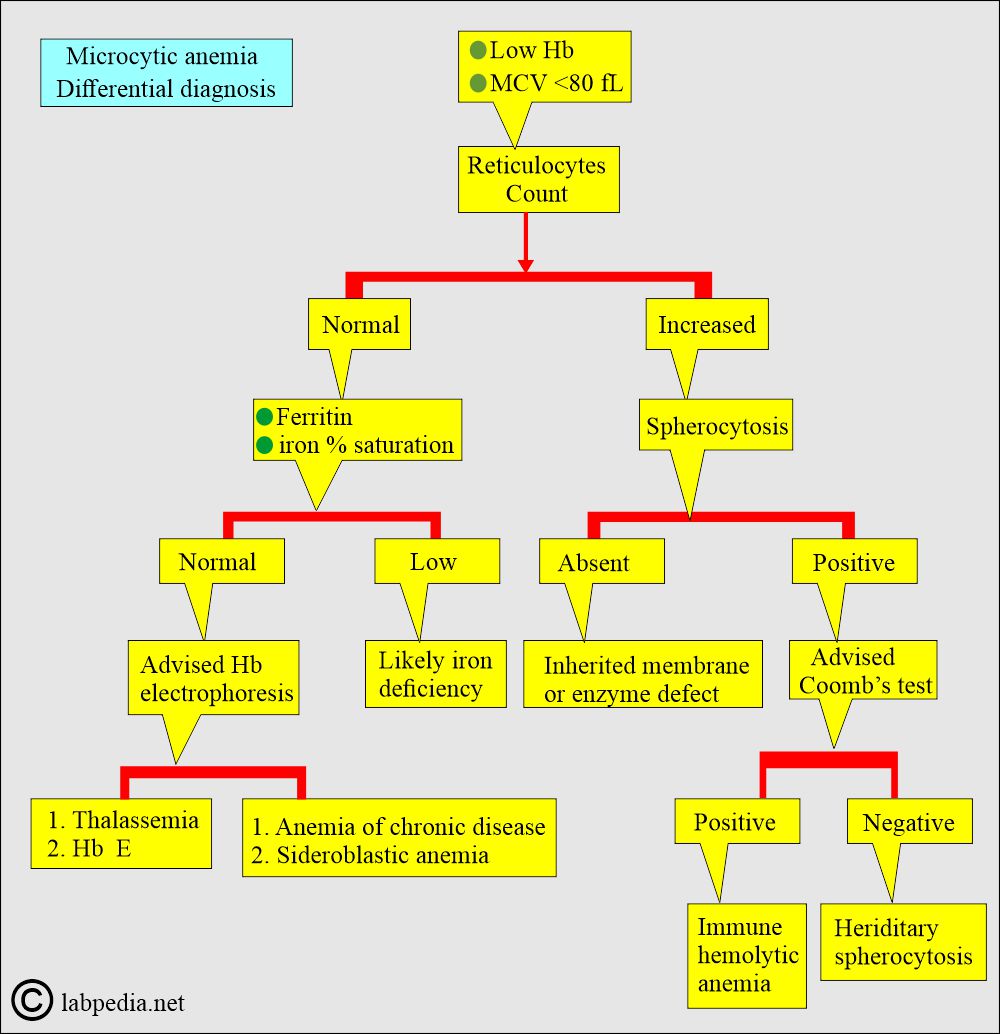
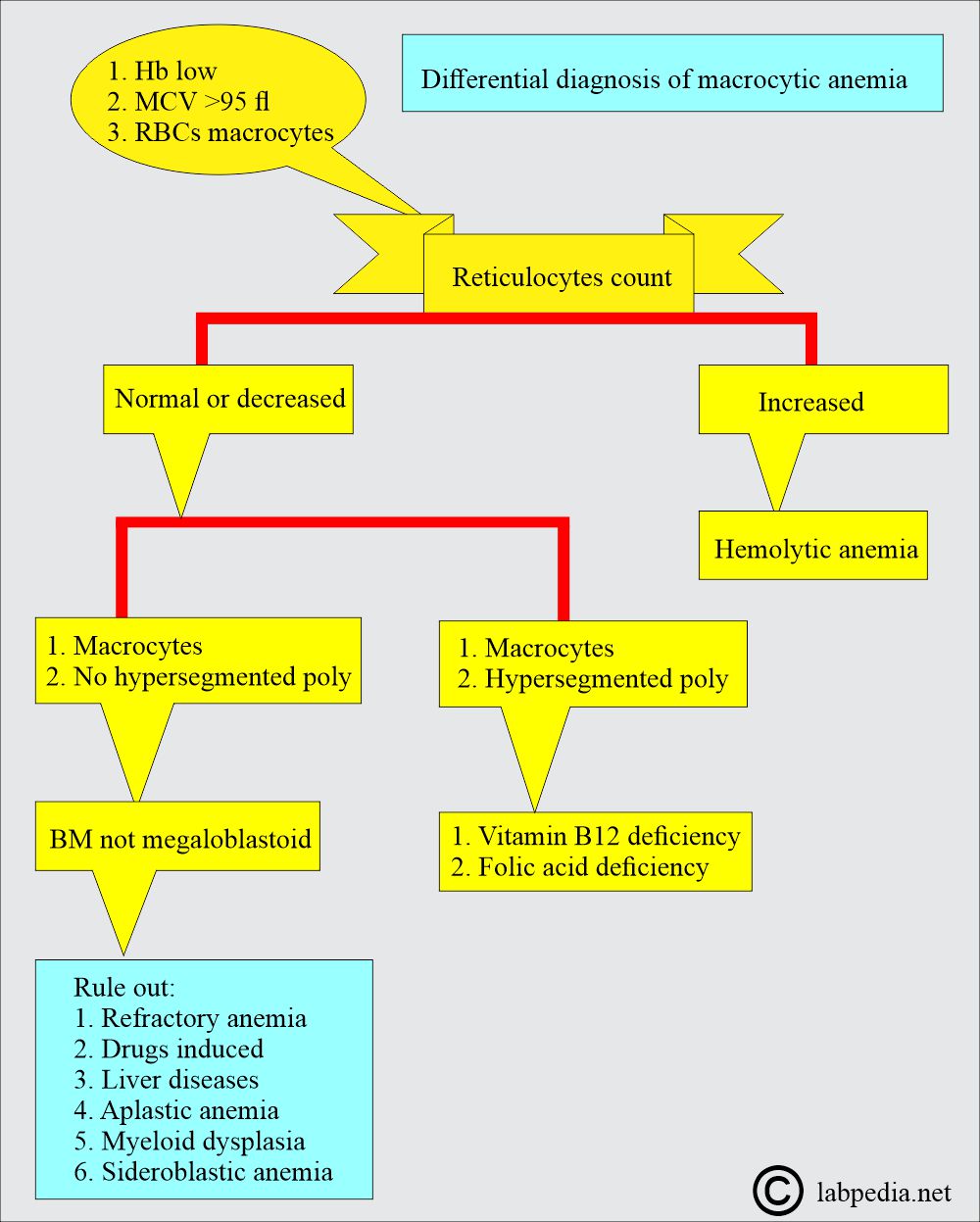
What are the types of Anemias based on MCV?
Anemia is divided based on RBC indices (MCV) into the following broad categories:
- Microcytic, MCV <80 fl.
- Normocytic, MCV 80 to 100 fl.
- Macrocytic, MCV >100 fl.
How will you classify the anemia based on RBC indices?
- Normocytic:
- MCV is 80 to 100 fl (femtoliter).
- MCHC = 32 to 36%
- Macrocytic:
- MCV = >100 fl.
- Microcytic and hypochromic:
- MCV = <80 fl.
- MCHC = <32%.
How will you classify anemia?
| Type of anemia | MCV fl | MCHC% |
|
|
|
|
|
|
|
|
What are the findings in various anemias?
| Characteristics findings | Microcytic hypochromic | Normocytic normochromic | Macrocytic |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What are the signs and symptoms of anemia?
Clinically, S/S seen are:
- The main symptoms are due to cardiovascular system adaptation.
- Increased stroke volume, tachycardia, and the Hb O2 dissociation curve changes.
- Hyperdynamic circulation leads to tachycardia, a bounding pulse, systolic murmurs, especially at the apex, and cardiomegaly.
- Older adults may find S/S of congestive heart failure.
- Some patients with anemia have no S/S, while mild anemia may have severe S/S.
- Acute onset effect:
- The speed of onset is affected; acute onset has more S/S than the slow onset.
- The severity of the anemia: In the case of mild anemia, there are no S/S.
- When the Hb is <9 to 10 g/dL, it may show S/S.
- Even Hb as low as 6 g/dL may not produce severe S/S.
- Age:
- Older people tolerate less than young people.
- There is pallor on the face, and it is better judged from the tongue.
- The patient will feel weakness and fatigue.
- There is lethargy and malaise.
- On exertion, there is dyspnoea and palpitation.
- The older patients may have cardiac failure, angina, intermittent claudication, or confusion.
- This may cause retinal hemorrhage, and this may complicate anemia of rapid onset.
- The patient may like to eat clay, ice, and starch.
- The patient may have syncope after the exercise.
- They may have dizziness and headaches.
- There is tinnitus or vertigo.
- Usually, these patients are irritable.
- These patients may have gastrointestinal symptoms.
- These patients may have difficulty sleeping or concentrating.
What are the specific Signs of anemia?
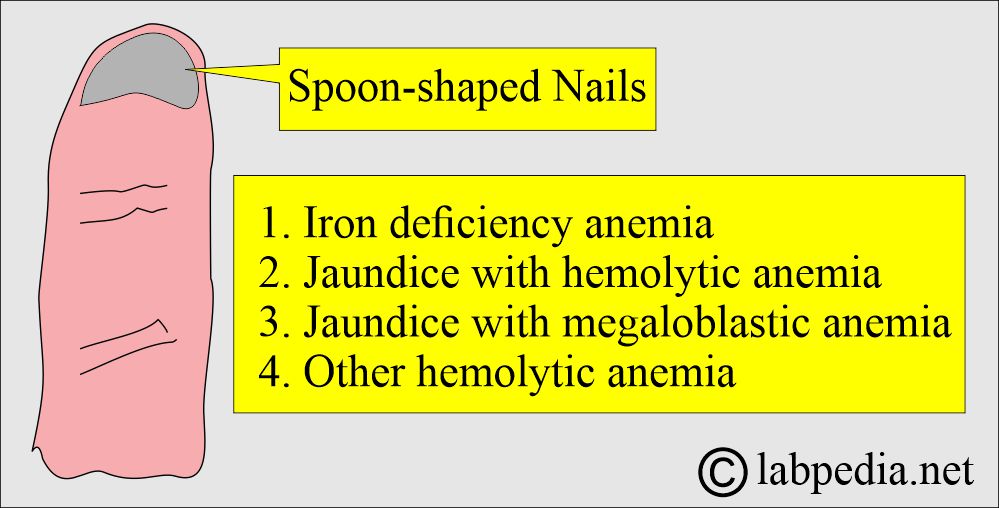
- Koilonychia:
- Which are spoon-shaped nails. This is usually seen in:
- Iron-deficiency anemia.
- Jaundice with hemolytic or megaloblastic anemia.
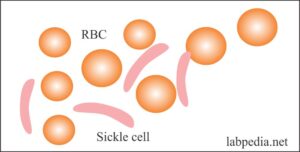
- Leg ulcers in Sickle cell anemia.
- Other hemolytic anemias.
- Bone deformities are seen in thalassemia and other severe congenital anemias.
- There may be infections and bruising with anemia due to bone marrow failure related to thrombocytopenia and neutropenia.
What are the Laboratory Criteria for the Diagnosis of Anemias?
- Hemoglobin is less than 12 to 13 G/dL.
- Hematocrit is less than 36 to 41%.
- Reticulocyte count was normal at 0.5 to 1.5%.
- MCV is a better choice for classifying anemias and their differentiation. This is useful for the screening of occult alcoholism.
- If MCV is high, then advise:
- Reticulocyte count.
- Vit.B12.
- Folate level.
- If MCV is low, then advise:
- Serum Iron.
- Iron binding capacity (TIBC).
- If the above two tests are low, advise Ferritin and Bone marrow examination.
- If normal, then advise electrophoresis.
- If MCV is normal, then advise:
- Serum Iron.
- Iron Binding Capacity. (TIBC).
- Comb’s test.
- Peripheral blood for RBC morphology.
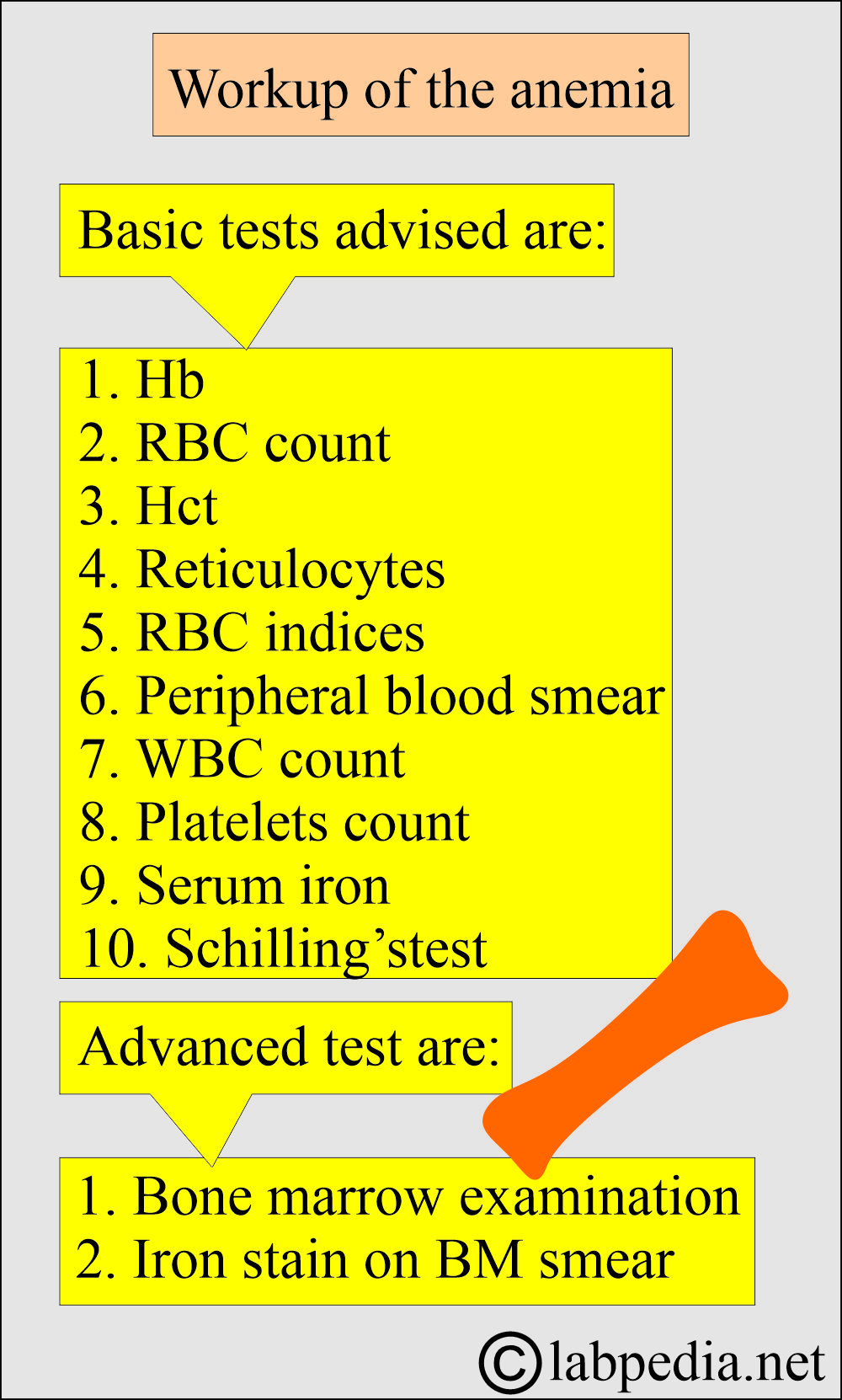
How will you do the routine workup of the patient with anemia?
- The patient’s detailed clinical history for diagnosis, physical examination, signs, and symptoms, with the following lab workup.
- Hemoglobin and hematocrit.
- Red blood cell count.
- Blood indices:
- MCH:
- It has limited value in the differential diagnosis of anemias. This is instrumental calibration.
- MCHC:
- It is also instrumental in calibration, and changes occur very late in iron-deficiency anemia when it is very severe.
- This is better for evaluating hypochromasia than MCH.
- Red cell distribution width (RDW):
- It helps to classify anemia with the help of MCV.
- RDW is more sensitive to the differentiation of microcytic anemia than macrocytic RBCs.
- This has no value in patients without anemia.
- Serum iron:
- Normal = 50 to 150 µg/dL).
- Total iron serum helps diagnose anemia.
- It differentiates between hemochromatosis and hemosiderosis.
- It should be measured along with TIBC to evaluate iron deficiency.
- This also helps to evaluate acute iron toxicity in children.
- Total iron-binding capacity (TIBC):
- Normal = 250 to 450 µg/dL).
- It helps in the differential diagnosis of anemias.
- It should be done along with serum iron to evaluate the % saturation and diagnose iron deficiency anemia.
- Transferrin:
- Serum Transferrin level is needed for the D/D of anemia.
- Percent transferrin saturation:
- Normal % transferrin saturation = 20% to 50%.
- Calculation of the % transferrin saturation =
- Serum iron ÷ TIBC x 100
- Transferrin is usually 33% saturated.
- This is used for the D/D of the anemias.
- This helps in the screening of hereditary spherocytosis.
- Ferritin:
- Serum ferritin (normal = 20 to 250 ng/dL).
- It correlates with the total body iron stores.
- It differentiates between iron deficiency and excess.
- It correlates with total body iron stores.
- It will predict and monitor iron deficiency.
- It will give an idea about the effectiveness of iron-deficiency anemia treatment.
- It differentiates iron deficiency from chronic diseases.
- It monitors the iron status in patients with chronic kidney disease with or without dialysis.
- It is used to study the population’s iron level and response to iron supplements.
- It can detect iron overload and monitor iron accumulation.
- It can help guide the response to iron depletion therapy.
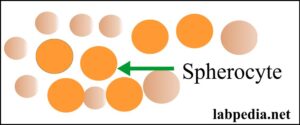
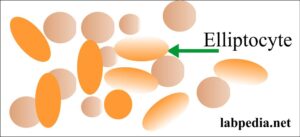
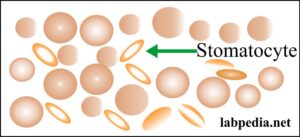
- Peripheral blood smear:
- This will inform the abnormality of the RBC shape, size, and any inclusions.
- There is a dimorphic picture in a mixed deficiency of iron, vitamin B12, or folate; there are microcytes and macrocytes. In this case, blood indices may be normal.
- Also, find the abnormal white cells and assess the platelets.
- It can find blast cells like normoblasts or granulocyte blast cells.
- Reticulocyte count:
- The normal range is 0.5 to 2.5%, and the absolute count is 25 to 125 x 109/L.
- Reticulocytes are raised in anemia because of the raised level of erythropoietin.
- After the acute hemorrhage:
- Erythropoietin level rises in 6 hours.
- Reticulocyte level increases in 2 to 3 days, and the peak level reaches 6 to 10 days.
- Reticulocytes will be raised until the Hb becomes normal.
- If the reticulocyte count is not raised in anemia, it means a bone marrow abnormality or a lack of erythropoietin stimulus.
- White blood cell count and platelet count:
- This will rule out the pancytopenia from the anemia.
- In hemolysis or hemorrhage, the neutrophils and the platelets are raised.
- In leukemias, the white cells are also raised.
- This will rule out the pancytopenia from the anemia.
- Bone marrow examination:
- Bone marrow may be aspirated, or a biopsy may be taken.
- This will give the cellularity like myeloid: erythroid ratio, and the presence of abnormal cells, like cancer cells, that infiltrate.
- Can do Special stains like iron.
What are the normal adult blood indices values?
| RBCs values | Male | Female |
| Hemoglobin (Hb g/dL) | 13.5 to 17.5 g/dL | 11.5 to 15.5 g/dL |
| Hematocrit (Hct % or Packed cell volume = PCV) | 40 to 52 % | 36 to 48% |
| RBC count | 4.5 to 6.5 x1012 /L | 3.6 to 5.6 x 1012/L |
| Mean cell volume (MCV) | 80 to 95 fL | |
| Mean cell hemoglobin (MCH) | 27 to 34 pg | |
| Mean cell hemoglobin concentration (MCHC) | 30 to 35 g/dL | |
| Reticulocytes count | 25 to 125 x 109/L |
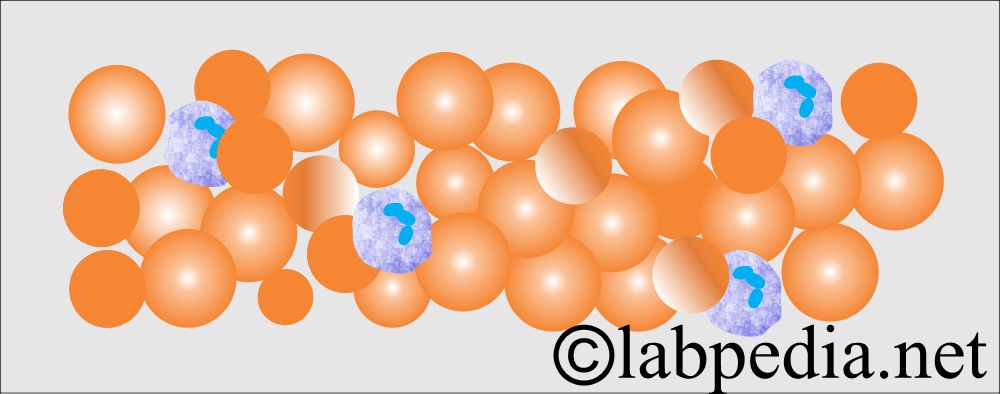
How would you describe Normochromic and normocytic Anemia?
Lab findings:
- Low hemoglobin.
- Normal MCV 80 to 95 fL.
- Normal MCH ≥27 pg.
- Normal MCHC.
- Mostly, these are due to acute blood loss.
- The peripheral blood smear shows normal-looking RBCs and normal RBC indices.
-
- The RBCs produced by the bone marrow are normal, but the number of RBCs in circulation is reduced for many reasons.
What are the causes of normochromic and normocytic anemia?
- Iron deficiency in the early stages.
- Acute blood loss.
- Chronic diseases of the kidneys and the liver.
- Infiltration by leukemia and multiple myeloma.
- Drugs like chloramphenicol cause aplastic anemia.
- Acquired hemolytic anemia may be from the prosthetic surgery of the heart.
- Pregnancy is due to increased plasma volume.
- Overhydration.
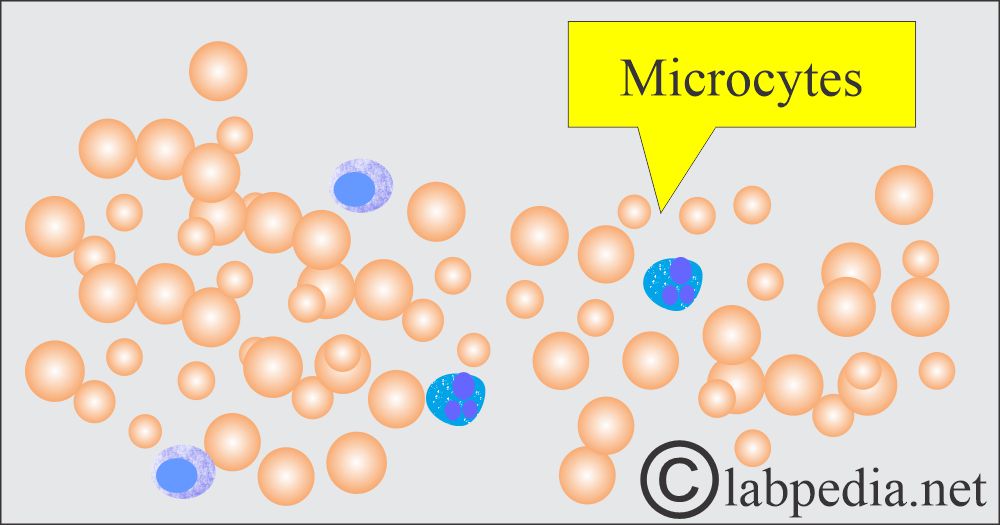
How would you describe microcytic and hypochromic anemia?
- These are the most common types of anemia, and iron deficiency is the most common cause.
What are the causes of microcytic hypochromic anemia?
- This is due to iron deficiency caused by decreased iron intake in the diet or impaired absorption.
- Iron deficiency anemia.
- Lead poisoning.
- Thalassemia.
- There may be an increased iron loss due to chronic bleeding.
- There may be an abnormality in iron metabolism.
- Increased demand by the body in:
- Infancy.
- Pregnancy.
- Lactation.
- Due to cancer.
- Hemorrhoids.
- Hookworms.
- Drugs like salicylates (aspirin).
How will you diagnose microcytic hypochromic anemia?
- Low hemoglobin, males <12 g/dL and females <10 g/dL.
- Low MCV <80 fL.
- MCH < 27 pg.
- Findings in the iron-deficiency anemia:
- Serum iron is deficient.
- TIBC is very high.
- Serum ferritin = <10 ng/dL
- Free RBC protoporphyrin is high.
- RDW is high.
- RBC survival time is slightly less.
- Peripheral blood smears show microcytes and pale, hypochromic RBCs.
- There may be leucopenia.
- Platelets are high in cases of bleeding.
- Reticulocytes are lower than expected in the degree of anemia.
- Bone marrow shows erythroid hyperplasia.
- Iron stain shows deficient iron.
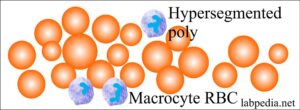
How would you describe Macrocytic Anemia?
- These are megaloblastic anemias resulting from the deficiency of vitamin B12, folic acid, or a combination of both.
What are the lab findings of macrocytic anemia?
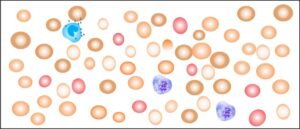
- Low hemoglobin.
- MCV > 99 fL.
- The peripheral blood smear shows macrocytosis and many hypersegmented neutrophils.
- Occasionally, you may see leucopenia and thrombocytopenia.
What are the causes of macrocytic anemia?
- Vitamin B12 deficiency.
- Folic acid deficiency.
- Or a combination of both
- Chemotherapy side effects.
- In the case of hydantoin therapy.
How would you describe Hemolytic Anemia?
How will you define hemolytic anemia?
- Hemolytic anemia is a disorder associated with the decreased life span of RBCs.
- The shortened life span of RBCs may be an intracorpuscular or extracorpuscular abnormality.
- The severity depends on the rate of destruction and the removal of RBCs.
- The normal bone marrow can increase its work by 6 to 8 times, so the anemia may not be apparent until the RBC’s life span reaches only 20 days.
What are the causes of hemolytic anemia?
- Intrinsic defects like:
- Hereditary defects like:
- An abnormal RBC membrane detects hereditary spherocytosis.
- Inherited RBC enzyme disorders like G-6-phosphate dehydrogenase deficiency.
- Disorders of abnormal hemoglobin production, such as sickle cell disease.
- Thalassemia syndrome.
- Paroxysmal nocturnal hemoglobinuria.
- Hereditary defects like:
- Extrinsic defects like:
- Chemical and toxic agents.
- Infection causing hemolysis.
- Hypersplenism.
- Immune hemolytic anemia.
How will you diagnose hemolytic anemia?
- There is a raised bilirubin level.
- There are increased reticulocytes.
- There is polychromasia.
How will you summarize lab findings in various anemias?
| Type of anemia | Hb | MCV | MCH | MCHC |
|---|---|---|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
How will you summarize lab findings in various anemias?
Anemia type |
HB |
MCV |
MCH |
MCHC |
Ferritin |
Iron binding capacity |
serum iron |
RDW |
| Iron deficiency | low | low <76 fl | low | low/normal | decreased | increased | decreased | increased |
| Megaloblastic | low | high >100 fl/cell |
increased >32 pg |
low 32 to 36 g/dL | raised/normal | increased | ||
| Chronic illness | low | low/normal | low | low | normal/ increased | normal / decreased | decreased | normal |
| Alpha Thalassemia | low or normal | low | low | low | normal /increased | normal |
normal or increased |
increased |
| Beta Thalassemia | low | low | low | low | increased/normal | normal | increased/normal | increased |
| Aplastic anemia | low | increased | normal | normal | normal |
How will you classify anemia based on RDW?
| Cell size |
Normal RDW |
High RDW |
|
|
|
|
|
|
|
|
|
What is the relation between MCV and RDW in various diseases?
| Red cell distribution (RDW) | Mean corpuscular volume (MCV) | Etiology (causes ) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
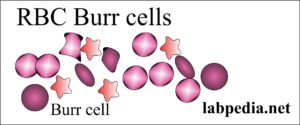
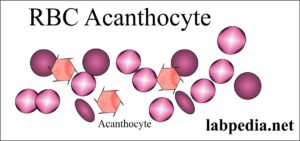
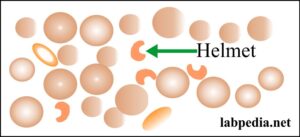
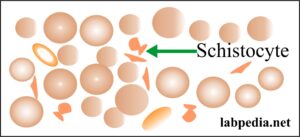
What are the abnormalities of RBCs and their etiology?
How will you summarize lab findings in various anemias?
| Lab test | Iron-deficiency anemia | Pernicious anemia | Folic acid deficiency | Aplastic anemia | Thalassemia | Sideroblastic anemia | Hemolytic anemia | Post-hemorrhagic anemia | Anemia of chronic diseases |
| Hemoglobin | Low | Low | Low | Low or normal | Low | Low | Low | Normal or low | Low |
| Hematocrit | Low | Low | Low | Low or normal | Low | Low | Low | Normal or low | Low |
| MCV | Low | High | High | A normal or mild increase | Low | Low | Normal or high | Slightly low | Low or normal |
| Reticulocytes count | A normal or mild increase | Low | Low | Low | Increased | A normal or mild increase | High | Increased | Normal |
| Plasma Iron | Low | Increased | Increased | Increased | Increased or normal | Increased | Normal or high | Normal | Low |
| TIBC | Increased | Normal | Normal | Normal | Normal | Normal | Normal | Normal | Low |
| Ferritin level | Low | Increased | Increased | Normal | Increased or normal | Increased | Normal | Normal | Normal |
| Folate level | Normal | Normal | Low | Normal | Normal | Normal | Normal | Normal | Normal |
| Serum B12 level | Normal | Low | Normal | Normal | Normal | Normal | Normal | Normal | Normal |
| Transferrin | Low | Mild increase | Mild increase | Normal | Increased | Normal | Normal | Mildly low | |
| Bilirubin level | Normal | Mild increase | Mild increase | Normal | Increased | Increased | Increased | Normal | Normal |
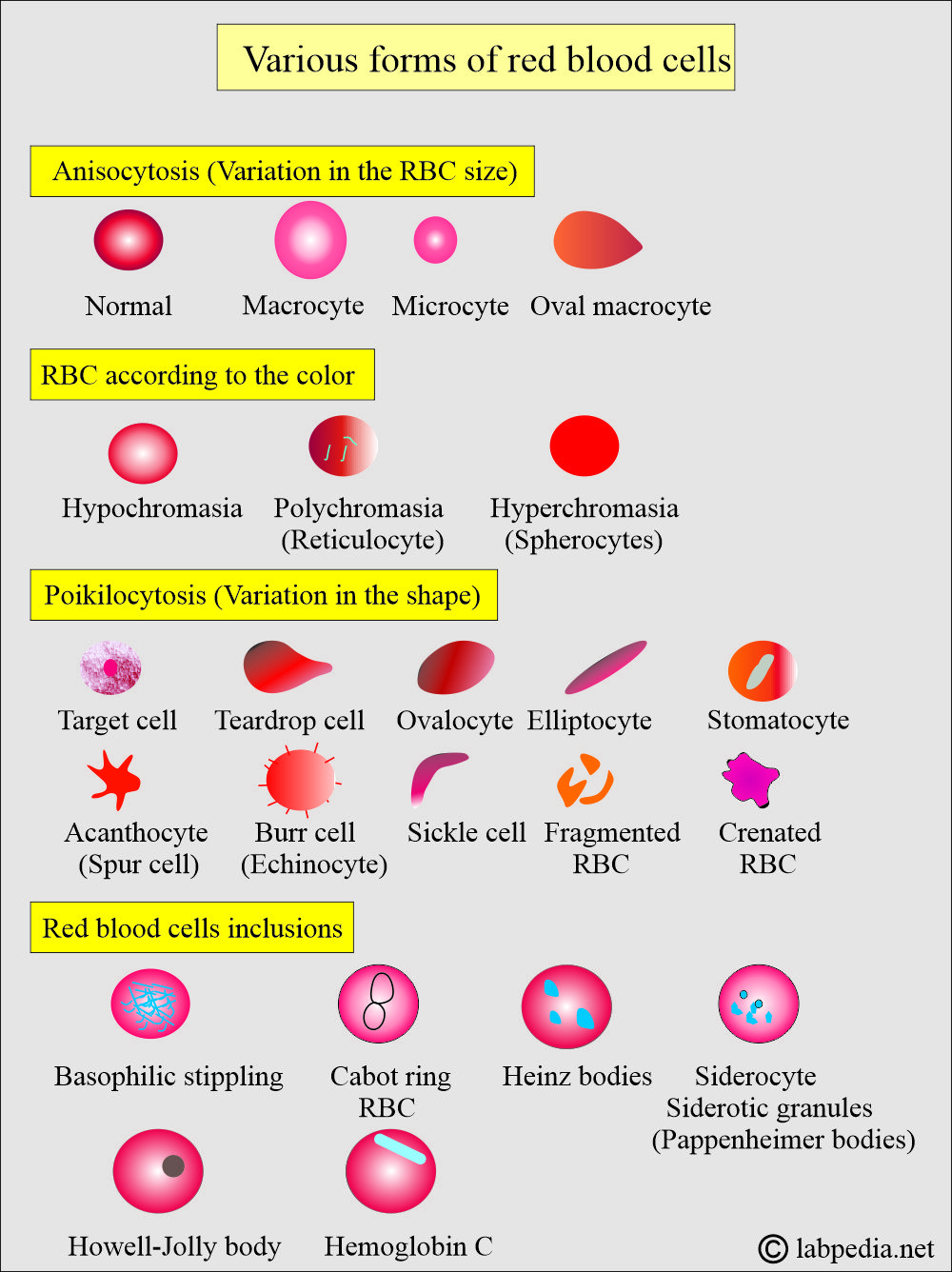
What are the various forms of red blood cells?
Panic values are:
- Hb = <5 g/dL or >20 g/dL
- Hct = <20 % ( leads to heart failure) or > 60% (leads to spontaneous clotting).
Questions and answers:
Question 1: Does red blood cell distribution (RDW) differentiate between thalassemia, anemia of chronic diseases, and iron deficiency anemia?
Question 2: What will happen to the following laboratory parameters in hemolytic anemia: 1. Reticulocytes 2. RDW 3. Indirect bilirubin 4. Haptoglobin?



Thanks
Thanks for the appreciation.
very insightful sir…
Thanks.
Dead written content, Really enjoyed reading through.
Thanks
Thank you so much for this. We have a discussion about Anemia in class and this has helped me a lot.
Thanks.
Many thank.
You are welcome.
really great write up. very informative .thanks
Thanks.
Wow, good work
Thanks.
Dr. Riaz,
This was AWESOME! How in the world did you put this all together? I want to share this with my classmates. My name is Rhonda and I am a NP student graduating in August 2022. I so happy that this popped up into my feed. Thank you so much for the time and effort you put into this presentation on anemia. I will print this and use this in my practice years to come. Have you written anything else?
Thanks for the remarks. You can see other topics on labpedia.net.
Helpful for ME thank you 😊
Thanks.
thanks!
Awesome
Thanks.
I really appreciate this
Thanks.
Amazing content! Much appreciated
Thanks.
Thank you for all this information, I really appreciate it.
Thanks.
Hi, this really was helpful for me , especially the charts! Thanks Dr. Riaz!
Thanks.
Thanks ,is really helpful
Thanks.
is really helpful notes. thanks for sharing
Thanks.
Assalamu Alaykum,
This was awesome and really captures every important aspect of Anaemia, may Allah reward your efforts Dr !
Thanks.
Good morning
I think DR.Riaz in Anemia classification based on RBC morphology:
3-(Normochromic)* and macrocytic anemias are due to:
* I think the correct (Hyperchromic)
I have tried to see many references, but mostly says normochromic and macrocytic. Please check the topic again. I have made some changes.
This is exactly what I have been looking for! As a Registered Dietitian, I am brushing up on anemia. Took me quite a while to find information that is cut and dry and easy to follow. Thank you.
Thanks.
Wow it’s so awesome
Thanks.