Amyloidosis, Samples, and Diagnosis
Amyloidosis
What sample is needed for the diagnosis of Amyloidosis?
- Gingiva: The gingival biopsy is positive in one-half to two-thirds of the cases.
- Rectum: The rectal biopsy is also positive in two-thirds of the cases.
- Kidney: A needle biopsy of the kidney is needed when gingival and rectal biopsies are not helpful.
- Skin: The skin biopsy may also be the site for amyloidosis diagnosis.
- Other sites depend upon the involvement of other organs like the GIT, spleen, and respiratory tract.
- Serum and urine will show a monoclonal band on electrophoresis.
How would you define Amyloidosis?
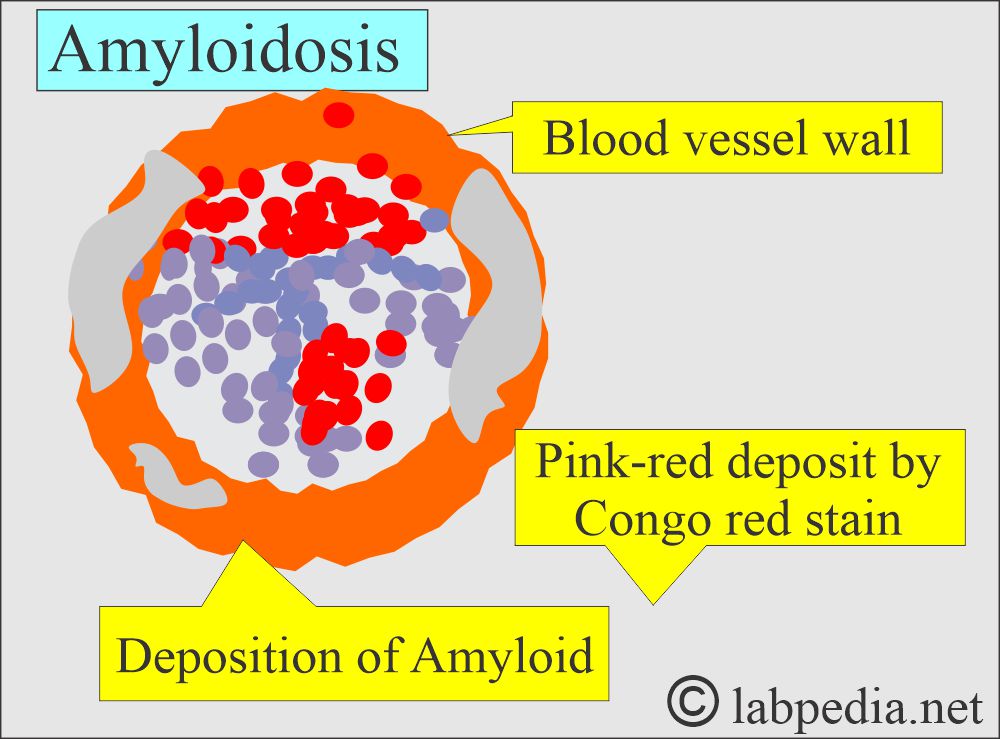
- Amyloidosis is a disorder of protein metabolism in which the extracellular deposition of pathologic insoluble fibrillary proteins in organs and tissues is present.
- Amyloidosis is the accumulation of various insoluble fibrillary proteins between the tissue cells and gives rise to the loss of the function of that organ.
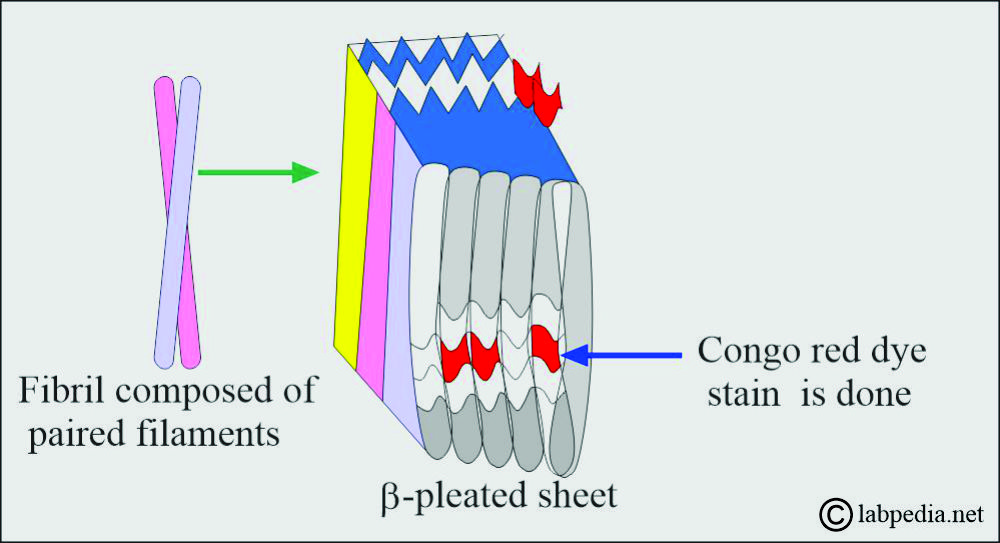
- The fibrils generally represent proteolytic fragments of various plasma proteins and possess the structure of a β-pleated sheet.
- These β-pleated sheets are insoluble and resistant to proteolysis.
- The term amyloidosis is a misnomer, as it was originally thought that fibrils are starch-like.
- Its affinity with Congo red is the basis of its definition and identification in the biopsy material.
What are the causes of Amyloidosis?
- Leprosy in 1/3 of the cases.
- Chronic infections like osteomyelitis and tuberculosis. Etc.
- Multiple myelomas.
- Other malignancies like renal cell carcinoma and lymphomas.
How would you discuss the pathophysiology of Amyloidosis?
- Amyloid is a Greek word resembling starch because it stains with iodine and other dyes.
- Amyloidosis is a rare disease that occurs when a substance called amyloid (folded protein) builds up in various organs.
- The most common precursor proteins are immunoglobulin light chains.
- Amyloid is a pathological extracellular deposit that appears structureless and translucent.
- It stains with iodine and various dyes.
- Under polarized light, amyloid with Congo red shows apple-green fluorescence.
- Amyloid exerts pressure on the vital organs and lead to death.
- Amyloid is an abnormal protein usually produced in bone marrow, an insoluble protein, and can be deposited in any tissue or organ.
- Amyloidosis is usually seen in the heart, liver, spleen, kidney, nervous, and gastrointestinal systems.
- Amyloid is an extracellular deposit of the amyloid protein.
- Hematoxylin and eosine stains show amyloid as amorphous, eosinophilic, hyaline extracellular substances.
- It encroaches on the adjacent cells and leads to atrophy of the surrounding cells.
- This is not a single disease; rather, it is a group of diseases that share the deposition of similar-appearing proteins.
What is the biochemistry of the amyloid?
- Amyloid is an insoluble protein resistant to normal proteolysis due to its β- conformation.
- The above feature is common to all types of amyloid, whatever their composition.
- Amyloid fibrils may have multiple soluble plasma protein precursors modified by proteolysis to make them insoluble.
- The end result of this insoluble amyloid is the disease called amyloidosis.
- This deposit may be local or systemic.
- This amyloid material exerts local pressure, resulting in the tissue’s death.
What is the structure of the amyloid?
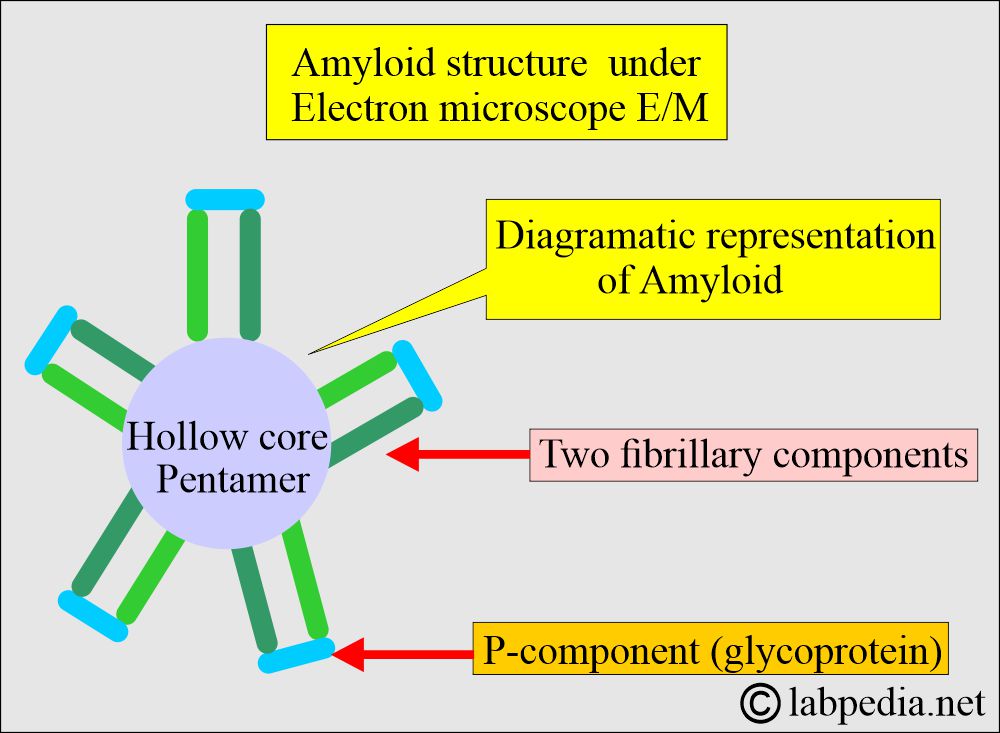
- Amyloids are nonbranching fibrils 7.5 to 10 nm in width by electron microscopy.
- The Electron microscopic picture shows:
- Two fibrillary components with characteristic periodicity.
-
- One rod-like structure P-component is a glycoprotein on their head.
How would you describe the Amyloid E/M structure?
- This has a hollow core and is a pentamer.
- These fibrillary components are crossed β-pleated sheets, seen by X-ray crystallography.
- Any fibrillar proteins deposited in the tissue that look like β-pleated sheets are amyloid.
- 95% of the amyloid is fibril proteins, and the rest 5% consists of P components or glycoproteins.
What is the chemical nature of the Amyloid?
- There are roughly 15 amyloid proteins, three of which are very common.
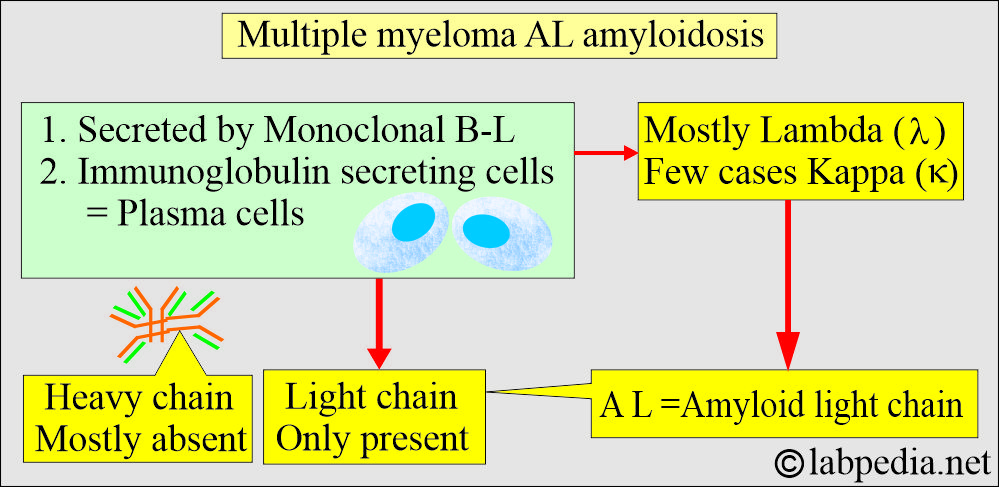
- Amyloid light chains (AL):
- These are derived from plasma cells and consist of immunoglobulin light chains.
- This may be light chain κ or λ.
- This is seen in plasma cell neoplasm, lymphomas, cardiomyopathy, macroglossia, and hepatosplenomegaly.
- Amyloid-associated amyloid (AA):
- These are non-immunoglobulin proteins synthesized by the liver.
- This is also called serum amyloid-A protein (SAA).
- This is secondary amyloidosis. This is seen in the following conditions:
- Chronic diseases like tuberculosis, bronchiectasis, Crohn’s disease, nephrotic syndrome, cardiomyopathy, and rheumatoid arthritis.
- αβ amyloid is a β-precursor protein and is found in:
- Patients with Alzheimer’s disease.
- Type 2 diabetes.
- β2 –Microglobulin amyloid is β2 –Microglobulin and is found in:
-
- Renal failure.
- Musculoskeletal diseases.
- Long-term hemodialysis.
-
- ATTR amyloid is transthyretin. It is found in the following conditions:
- Neuropathy.
- Cardiomyopathy.
- Senile amyloidosis with cardiomyopathy.
How will you classify Amyloidosis according to etiology?
1. Primary Amyloidosis:
- It comprises a portion of the light chain called immunoglobulin light chain (AL) amyloidosis.
- This is produced spontaneously from plasma cells and may be seen in bone marrow cancers like Multiple myelomas.
- Amyloidosis is associated with multiple myeloma.
- These two types are associated with increased plasma cells (Plasmacytosis).
- The monoclonal proliferation of the cells results in two identical light chains known as AL amyloid.
- This primary amyloidosis is derived from the variable region of the immunoglobulin’s light chains, and the most common is lambda (λ).
2. Amyloidosis is associated with multiple myeloma:
- Groups 1 and 2 are associated with plasmacytosis in the bone marrow, and these will produce an excess of the light chain of the immunoglobulins called AL amyloidosis.
- Multiple myeloma is associated with 20% to 30% of the cases.
- Electrophoresis shows the monoclonal peak in serum and urine in 50% of the cases.
- Immunoelectrophoresis is positive in the serum and urine in about 90% of the cases.
3. Secondary Amyloidosis (Reactive systemic):
- It results from chronic illnesses like tuberculosis, osteomyelitis, or other chronic inflammatory diseases like rheumatoid arthritis and ankylosing spondylitis.
- This is called secondary amyloidosis or AA amyloidosis.
- AA protein is an amino-terminal fragment of serum amyloid A protein with a molecular weight of 220 to 235 kDa. It forms a complex with HDL and circulates in the blood.
- AA amyloid is an acute-phase protein that increases rapidly in infectious or noninfectious inflammation.
- These are associated with chronic inflammatory diseases.
- Rheumatoid arthritis has an incidence of 20% and Other inflammatory joint diseases.
- AA is also deposited in chronic suppurative and granulomatous diseases (TB, osteomyelitis).
- Deposits of AA amyloid most frequently occur in the kidney, liver, and spleen.
- AA may deposit in non-lymphoid tumors like renal and gastric carcinoma. This is also found in Hodgkin’s lymphoma.
- There may be nephrotic syndrome and hepatosplenomegaly.
4. Aging (senile amyloidosis):
- Amyloidosis is associated with the aging process.
- This is also called senile amyloidosis, and most often, the heart is involved, which is called senile cardiac amyloidosis.
- This may also be found in the pancreas and brain.
- Nodular or infiltrative amyloid deposits are seen in the skin, lungs, trachea, and endocrine organs (thyroid medullary carcinoma) and long-standing diabetics (pancreas).
- These patients are usually asymptomatic except for the cardiac form.
5. Familial Amyloidosis:
- These are autosomally dominant transmitted diseases where the mutant protein forms amyloid fibrils, usually starting in middle age.
- The most common form is a mutant – transthyretin, a tetrameric protein with four identical subunits.
- This is a transport protein for thyroxine and retinol-binding protein, and it is mainly synthesized in the liver.
- It can cause amyloid polyneuropathy or cardiomyopathy. It can involve the kidneys and blood vessels.
How will you classi5fy Amyloidosis according to clinical presentation?
- Amyloidosis may be:
- Generalized or systemic: Multiple organs are involved.
- Primary amyloidosis occurs when there is a disturbance in the immune system.
- Seen in multiple myeloma and monoclonal B-cell proliferation.
- Secondary amyloidosis is when the cause is a chronic inflammatory disease.
- Reactive systemic amyloidosis.
- Primary amyloidosis occurs when there is a disturbance in the immune system.
- Localized: In this type, only one organ is involved, like amyloidosis of the heart.
- Senile cerebral changes were seen in Alzheimer’s disease.
- In medullary carcinoma of the thyroid (endocrine).
- Islets of Langerhans (endocrine).
- Isolated atrial amyloidosis.
- Hereditary or familial amyloidosis is a separate group with a different pattern of organ involvement.
- Familial Mediterranean fever.
- Familial amyloidotic neuropathies.
- Senile systemic amyloidosis. This is often found in the heart and is called senile cardiac amyloid. This may also be seen in the brain and pancreas.
- Nodular or infiltrative amyloid deposits may be seen in the skin, lungs, and trachea.
- It may be seen in long-standing diabetes mellitus in the pancreas.
- It may be seen in the thyroid in the case of medullary carcinoma.
-
- These forms are asymptomatic except for the heart.
-
Another classification of Amyloidosis:
- Reactive (secondary) amyloidosis.
- Nodular deposits.
- Light chain (primary) amyloidosis.
- Hereditary amyloidosis.
- Endocrine amyloidosis.
- Cerebral amyloidosis.
- Cardiac amyloidosis.
- Hemodialysis-associated amyloidosis.
- Other types.
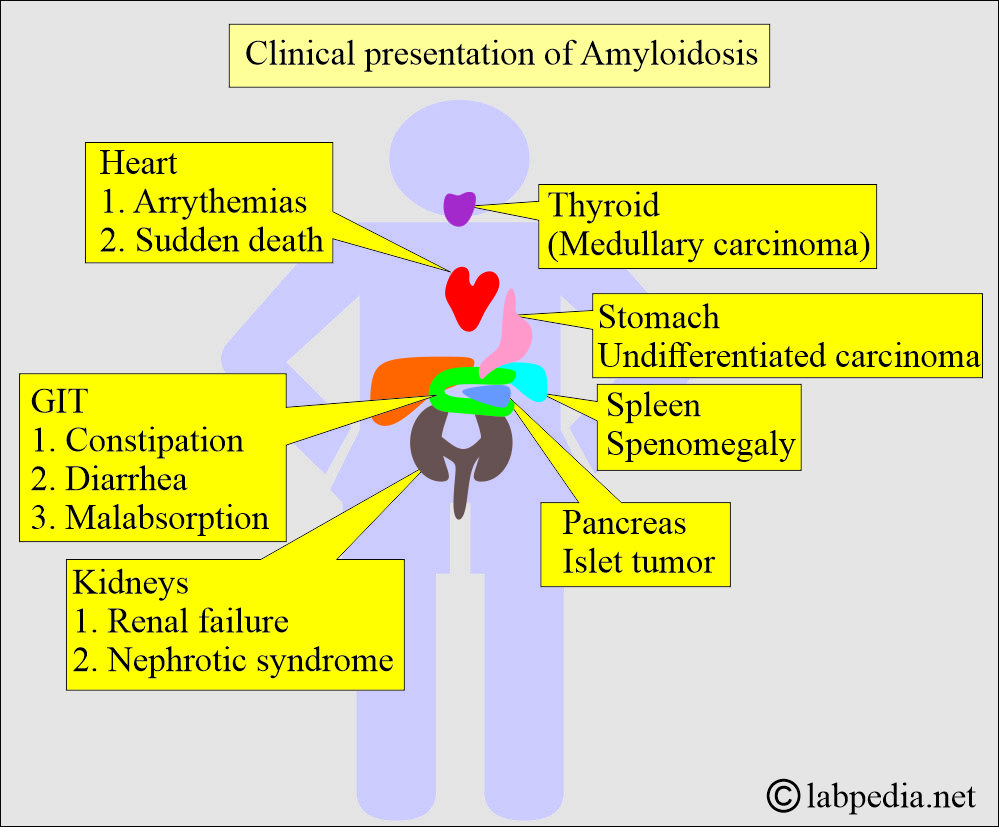
How would you discuss signs and symptoms of Amyloidosis?
- Except for the familial type of amyloidosis, it is seen in older patients with an average age of 60 years.
- These depend upon the organ involved.
- There are severe fatigue and weakness.
- There is a shortness of breath.
- There may be diarrhea with blood, and sometimes there is constipation.
- There may be swelling of the ankles and legs.
- The skin may show thickening or easy bruising and patches around the eyes.
- The most commonly involved organs are the Kidneys and the heart.
- There may be an irregular heartbeat.
- The patient may develop difficulty in swallowing.
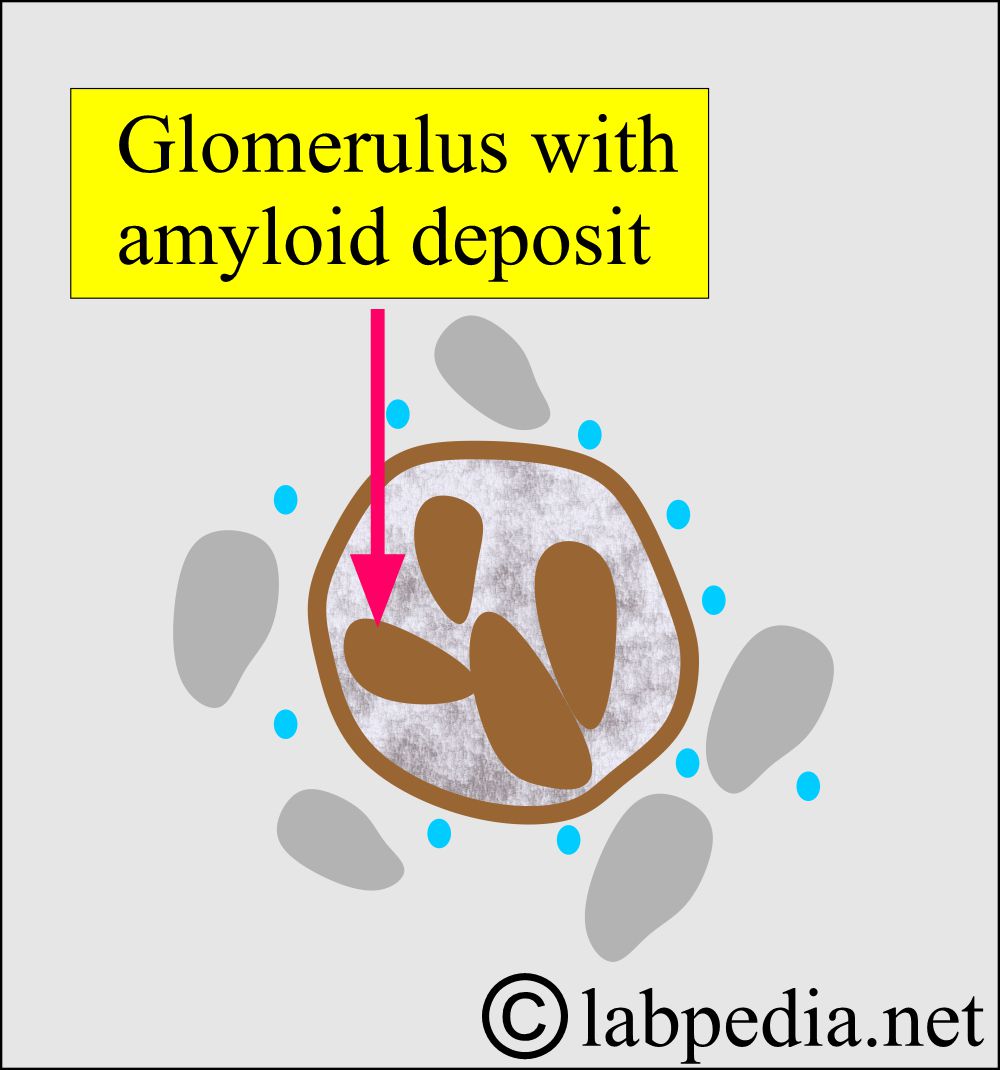
- Kidney involvement leads to nephrotic syndrome. There may or may not be raised creatinine and blood urea.
- The kidney is involved in 90% to 96 % of the cases with the amyloid type of AA.
- Immunoglobulin light-chain associated (AL) Amyloidosis associated organs involvement:
- This primary amyloidosis gives the S/S of the organ involved.
- Kidneys’ involvement will show proteinuria and nephrotic syndrome.
- The cardiovascular system shows cardiac failure.
- Carpal tunnel syndrome with weakness and paresthesia of the hands may be an early feature.
- Sensory neuropathies are common.
- Physical examination shows hepatomegaly, rarely splenomegaly, cardiomyopathy, polyneuropathy, and bruising may be seen.
- Macroglossia may be seen in 20% of the cases.
- Familial transthyretin-associated amyloidosis (ATTR):
- There is peripheral sensorimotor and autonomic neuropathy, and it is more common with symptoms of diarrhea and weight loss.
- Macroglossia is not seen in this type.
- Cardiac dysfunction is of conduction.
- Reactive or secondary (AA) amyloidosis:
- This is usually due to chronic inflammatory conditions like rheumatoid arthritis, inflammatory bowel disease, and untreated Mediterranean fever.
- It has been seen in patients with tuberculosis, bronchiectasis, and osteomyelitis in developed countries.
- Local amyloidosis: Amyloid fibrils are locally deposited in various organs, such as the skin, heart, and brain.
- Cerebral amyloidosis: Intracerebral and cerebrovascular amyloid deposits are seen in Alzheimer’s disease.
- In hereditary spongiform encephalopathies, several cerebral amyloid plaques are seen.
What are the risk factors leading to amyloidosis?
- Age: The most common age group involved is people 50 or older, except for the younger age group.
- Family history: Some amyloidosis is hereditary.
- Sex: The majority of the patients are male.
- Dialysis: This also leads the patients to amyloidosis.
- Chronic diseases: It will also predispose to amyloidosis.
What are the complications of amyloidosis?
- The kidney, when involved, will ultimately lead to renal failure.
- Kidney size may be normal or enlarged.
- Amyloid deposits in the glomeruli.
- Amyloidosis is also seen in the interstitium and the wall of blood vessels.
- The cardiovascular system leads to heart failure and arrhythmias.
- The heart size may increase from minimum to moderate enlargement.
- Amyloid deposits are found in the myocardium.
- The spleen may be enlarged moderately to a large size.
- Amyloid deposit is limited to splenic follicles and gives a sago spleen appearance.
- Liver amyloidosis causes massive enlargement.
- The amyloid deposit first appears in the space of Disse.
- Later on, it encroaches on the adjacent liver parenchyma.
- The late stages involve the sinusoids.
- The central nervous system leads to various complications, such as diarrhea, constipation, numbness of the fingers, and dizziness.
How will you diagnose Amyloidosis?
- Take a biopsy from the clinically affected tissue.
- Congo-red test: Congo-red binds the amyloid and gives apple-green fluorescence under polarized light.
- This test is positive in one-third of the primary amyloidosis and about two-thirds of the secondary amyloidosis of patients.
- Fat aspiration from the subcutaneous tissue showed positivity in 75% of the cases.
- 85% positive in the AL amyloidosis from the abdominal subcutaneous fatty tissue.
- Gingival and rectal biopsy is positive in one-half to two-thirds of patients.
- In the case of kidney involvement, a needle biopsy of the kidney is needed.
- Bone biopsy is positive in 30% of the multiple myeloma cases.
- Liver needle biopsy may be positive.
- In case of skin involvement, take a biopsy from the plaques.
- A biopsy of the carpal tunnel tissue in carpal tunnel syndrome is positive in 90% of cases.
- The biopsy may be taken from the GIT, spleen, and respiratory system.
- Immunohistochemical staining shows the reaction of fibrils with Kappa (κ) or lambda (λ) antisera.
- E/M is the most specific for the diagnosis of amyloidosis.
- Bone marrow may show increased plasma cells in primary amyloidosis or lymphoproliferative disorders.
- Urine may show proteinuria and light chains in AL amyloidosis.
- There may be paraproteinemia.
- Scintigraphy using the 123I-labelled serum amyloid P component is useful for diagnosing AL, ATTR, and AA amyloidosis. However, this test is not available in most labs.
How will you treat Amyloidosis?
- There is no definite treatment or cure for amyloidosis.
- However, treatment can limit the production of amyloid protein.
- There is a symptomatic treatment for Nephrotic syndrome and cardiac failure.
- Colchicine may be helpful for familial Mediterranean fever.
- Chemotherapy may show some benefits in AL amyloidosis.
What is the prognosis of Amyloidosis?
- It depends upon the type of amyloidosis and the organ involved.
- In generalized amyloidosis, the prognosis is poor, with mean survival after diagnosis of 1 to 3 years.
- Microscopic and focal deposits in older people are of no clinical significance.
- Widespread deposits are progressive and fatal.
- AL Amyloid patients with cardiac involvement have a worse prognosis; in untreated cases, the survival is less than one year.
- AA amyloid patients survive 2 to 4 years.
- ATTR amyloid patients survive for 15 years.
- For patients with multiple myeloma-associated amyloidoses, the prognosis is poor.
- Treatment is aimed at:
- Reducing the supply of precursor protein.
- Treat the bleeding problem.
- Increase motility.
Questions and answers:
Question 1: What is the special stain for amyloidosis?
Question 2: What is the best site for the diagnosis of amyloidosis?