Amyloidosis, Samples, and Diagnosis
Amyloidosis
Sample for Diagnosis of Amyloidosis
- Gingiva: The gingival biopsy is positive in one-half to two-thirds of the cases.
- Rectum: The rectal biopsy is also positive in two-thirds of the cases.
- Kidney: A needle biopsy of the kidney is needed when gingival and rectal biopsies are not helpful.
- Skin: The skin biopsy may also be the site for amyloidosis diagnosis.
- Another site depends upon the involvement of other organs like GIT, spleen, and respiratory tracts.
- Serum and urine will show a monoclonal band on electrophoresis.
Definition of Amyloidosis:
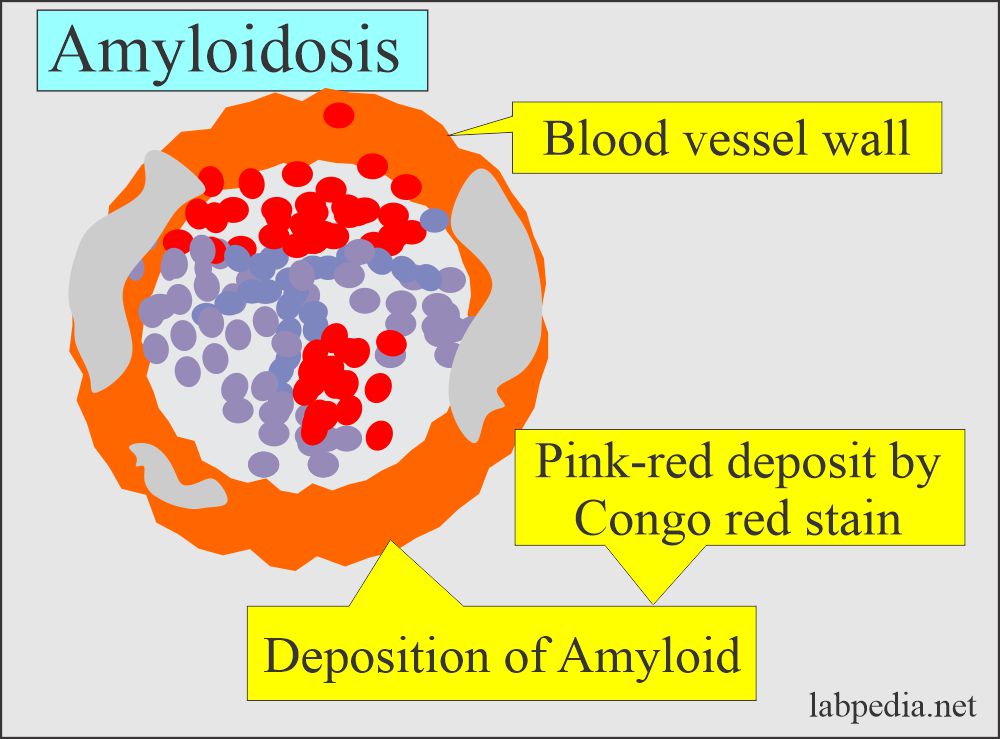
- Amyloidosis is a disorder of protein metabolism in which there is the extracellular deposition of pathologic insoluble fibrillary proteins in organs and tissues.
- Amyloidosis is the accumulation of various insoluble fibrillary proteins between the tissue cells and gives rise to the loss of the function of that organ.
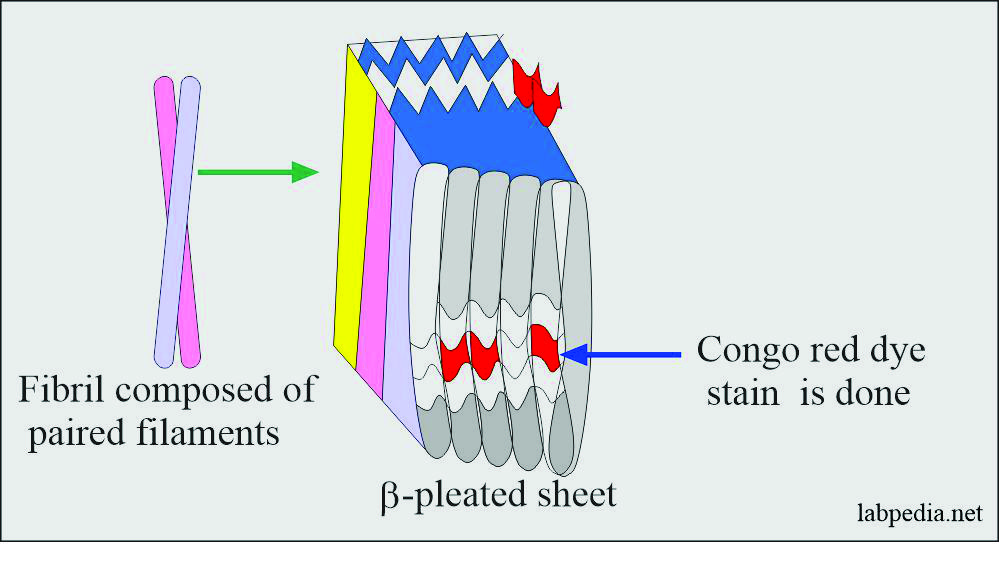
- The fibrils generally represent proteolytic fragments of various plasma proteins and possess the structure of a β-pleated sheet.
- These β-pleated sheets are insoluble and resentence to proteolysis.
- The term amyloidosis is a misnomer, as originally thought that fibrils are starch-like in nature.
- Its affinity with congo red is the basis of its definition and identification in the biopsy material.
Causes of Amyloidosis:
- Leprosy in 1/3 of the cases.
- Chronic infections like osteomyelitis and tuberculosis. Etc.
- Multiple myelomas.
- Other malignancies like renal cell carcinoma and lymphomas.
Pathophysiology of Amyloidosis:
- Amyloid is a Greek word meaning resembling starch because of staining with iodine and other dyes.
- Amyloidosis is a rare disease that occurs when a substance called amyloid (folded protein) builds up in various organs.
- The most common precursor proteins are immunoglobulin light chains.
- Amyloid is a pathological extracellular deposit that appears structureless and translucent, and it stains with iodine and various dyes.
- Under polarized light, amyloid with congo red shows apple-green fluorescence.
- Amyloid exerts pressure on the vital organs and leads to death.
- Amyloid is an abnormal protein usually produced in bone marrow, an insoluble protein, and can be deposited in any tissue or organ.
- Amyloidosis is usually seen in the heart, liver, spleen, kidney, nervous, and gastrointestinal systems.
- Amyloid is an extracellular deposit of the amyloid protein.
- Hematoxylin and eosine stains show amyloid as amorphous, eosinophilic, hyaline extracellular substances.
- It encroaches on the adjacent cells and leads to atrophy of the surrounding cells.
- This is not a single disease; rather, it is a group of diseases sharing deposition of similar appearing proteins.
Biochemistry of the amyloid:
- Amyloid is an insoluble protein resistant to normal proteolysis due to its β- conformation.
- The above feature is common to all types of amyloid, whatever their composition.
- Amyloid fibrils may have multiple soluble plasma protein precursors modified by proteolysis to make them insoluble.
- The end result of this insoluble amyloid is the disease called amyloidosis.
- This deposit may be local or systemic.
- This amyloid material exerts local pressure, resulting in the tissue’s death.
Structure of the amyloid:
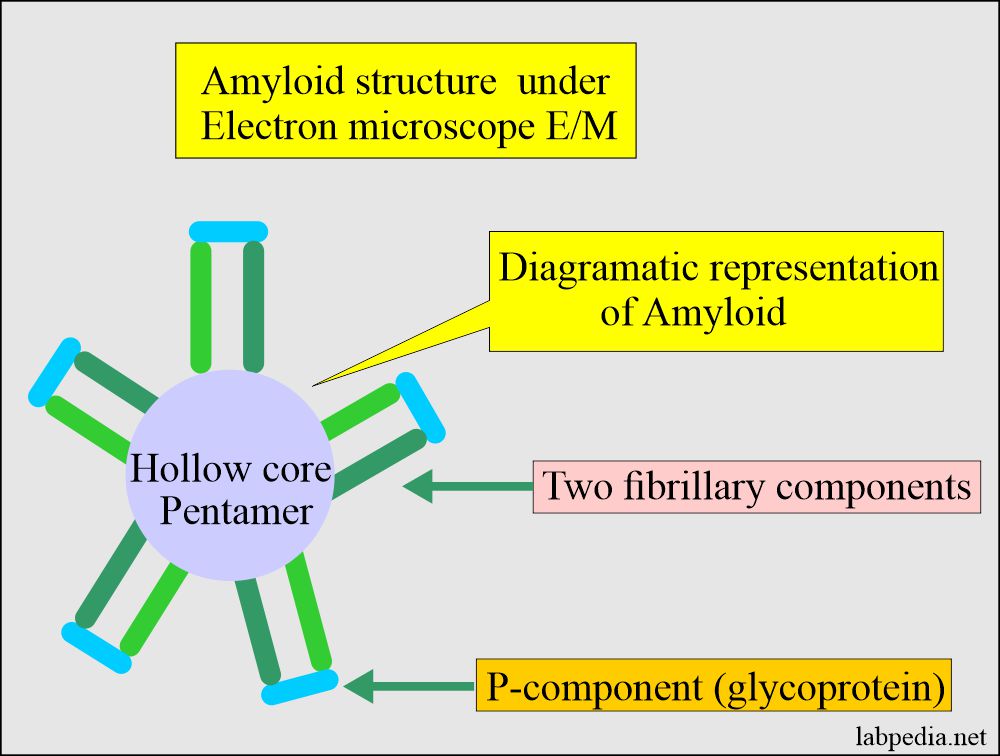
- Amyloid by electron microscopy is nonbranching fibrils 7.5 to 10 nm in width.
- The Electron microscopic picture shows:
- Two fibrillary components with characteristic periodicity.
-
- One rod-like structure P-component is a glycoprotein on their head.
Amyloid E/M structure:
- This has a hollow core and is a pentamer.
- These fibrillary components are crossed β-pleated sheets, seen by X-Ray crystallography.
- Any fibrillar proteins deposited in the tissue which look like β-pleated sheets are amyloid.
- 95% of the amyloid is fibril proteins, and the rest 5% consists of P components or glycoproteins.
Chemical nature of the Amyloid:
- There are roughly 15 amyloid proteins and three of these are very common.
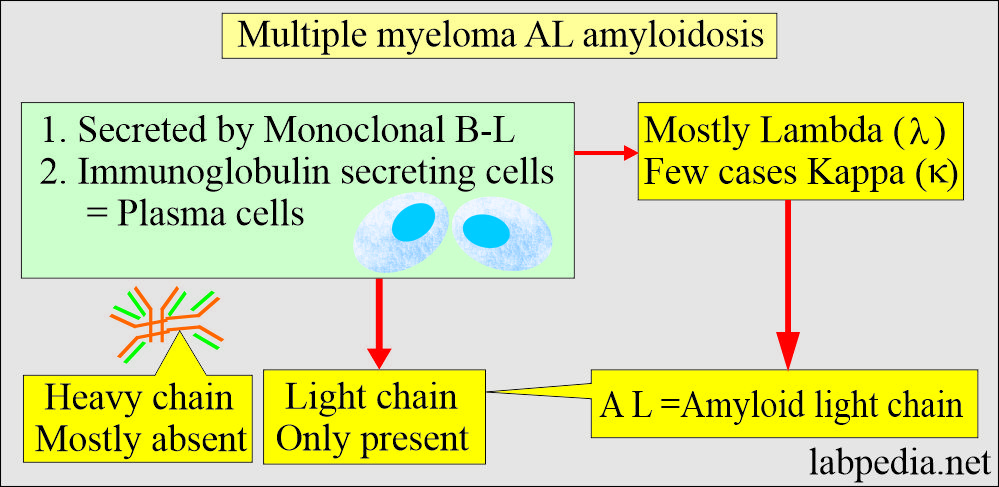
- Amyloid light chain (AL). These are derived from the plasma cells and consist of immunoglobulin light chains.
- This may be light chain κ or λ.
- This is seen in plasma cell neoplasm, lymphomas, cardiomyopathy, macroglossia, and hepatosplenomegaly.
- Amyloid-associated amyloid (AA). These are non-immunoglobulin proteins synthesized by the liver.
- This is also called serum amyloid-A protein (SAA).
- This is secondary amyloidosis. This is seen in the following:
- Chronic diseases like tuberculosis, bronchiectasis, Crohn’s disease, nephrotic syndrome, cardiomyopathy, and rheumatoid arthritis.
- αβ amyloid is a β-precursor protein and is found in:
- Patients with Alzheimer’s disease.
- Type 2 diabetes.
- β2 –Microglobulin amyloid is β2 –Microglobulin and is found in:
-
- Renal failure.
- Musculoskeletal diseases.
- Long-term hemodialysis.
-
- ATTR amyloid is transthyretin. It is found in the following conditions:
- Neuropathy.
- Cardiomyopathy.
- Senile amyloidosis with cardiomyopathy.
Classification of Amyloidosis according to etiology:
Primary Amyloidosis:
- It comprises a portion of the light chain called immunoglobulin light chain (AL) amyloidosis. This is produced spontaneously from the plasma cells, which may be seen in the cancer of bone marrow like Multiple myelomas.
- Amyloidosis is associated with multiple myeloma.
- These two types are associated with increased plasma cells (Plasmacytosis).
- There is the monoclonal proliferation of the cells giving two identical light chains known as AL amyloid.
- This primary amyloidosis is derived from the variable region of the immunoglobulin’s light chains, and the most common is lambda (λ).
Amyloidosis is associated with multiple myeloma:
- Above groups 1 and 2 are associated with plasmacytosis in the bone marrow, and these will produce an excess of the light chain of the immunoglobulins called AL amyloidosis.
- Multiple myeloma is associated with 20% to 30% of the cases.
- Electrophoresis shows the monoclonal peak in serum and urine in 50% of the cases.
- Immunoelectrophoresis is positive in the serum and urine in about 90% of the cases.
Secondary Amyloidosis (Reactive systemic):
- It results from chronic illnesses like tuberculosis, osteomyelitis, or other chronic inflammatory diseases like rheumatoid arthritis and ankylosing spondylitis.
- This is called secondary amyloidosis or AA amyloidosis.
- AA protein is an amino-terminal fragment of serum amyloid A protein with a Molecular weight of 220 to 235 kDa and forms a complex with HDL and circulates in the blood.
- AA amyloid is an acute-phase protein that increases rapidly in infectious or noninfectious inflammation.
- These are associated with chronic inflammatory diseases.
- Rheumatoid arthritis has an incidence of 20%, and Other inflammatory joint diseases.
- AA is also deposited in chronic suppurative and granulomatous diseases (TB, osteomyelitis).
- Deposits of AA amyloid most frequently occur in the kidney, liver, and spleen.
- AA may deposit in nonlymphoid tumors like renal and gastric carcinoma. This is also found in Hodgkin’s lymphoma.
- There may be nephrotic syndrome and hepatosplenomegaly.
Aging (senile amyloidosis):
- Amyloidosis is associated with the aging process.
- This is also called senile amyloidosis, and most often, the heart is involved called senile cardiac amyloidosis.
- This may also be found in the pancreas and brain.
- Nodular or infiltrative amyloid deposits s are seen in the skin, lungs, trachea, and endocrine organs (thyroid medullary carcinoma) and in long-standing diabetics (pancreas).
- These patients are usually asymptomatic except for cardiac form.
Familial Amyloidosis:
- These are autosomally dominant transmitted diseases where the mutant protein forms amyloid fibrils, usually starting in middle age.
- The most common form is a mutant – transthyretin, a tetrameric protein with four identical subunits.
- This is a transport protein for thyroxine and retinol-binding protein, and it is mainly synthesized in the liver.
- It can cause amyloid polyneuropathy or cardiomyopathy. It can involve the kidneys and blood vessels.
Classification of Amyloidosis according to clinical presentation:
- Amyloidosis may be:
- Generalized or systemic: Multiple organs are involved.
- Primary amyloidosis occurs when there is a disturbance in the immune system.
-
- Seen in multiple myeloma and monoclonal B-cell proliferation.
-
- Secondary amyloidosis when the cause is a chronic inflammatory disease.
-
- Reactive systemic amyloidosis.
-
- Primary amyloidosis occurs when there is a disturbance in the immune system.
- Localized: In this type, only one organ is involved, like amyloidosis of the heart.
- Senile cerebral changes were seen in Alzheimer’s disease.
- In medullary carcinoma of the thyroid (endocrine).
- Islets of Langerhans (endocrine).
- Isolated atrial amyloidosis.
- Hereditary or familial amyloidosis is a separate group with a different pattern of organ involvement.
- Familial Mediterranian fever.
- Familial amyloidotic neuropathies.
- Senile systemic amyloidosis. This is most often found in the heart, called senile cardiac amyloid. This may also be seen in the brain and pancreas.
- Nodular or infiltrative amyloid deposits may be seen in the skin, lungs, and trachea.
- It may be seen in long-standing diabetes mellitus in the pancreas.
- It may be seen in the thyroid in the case of medullary carcinoma.
-
- These forms are asymptomatic except for the heart.
-
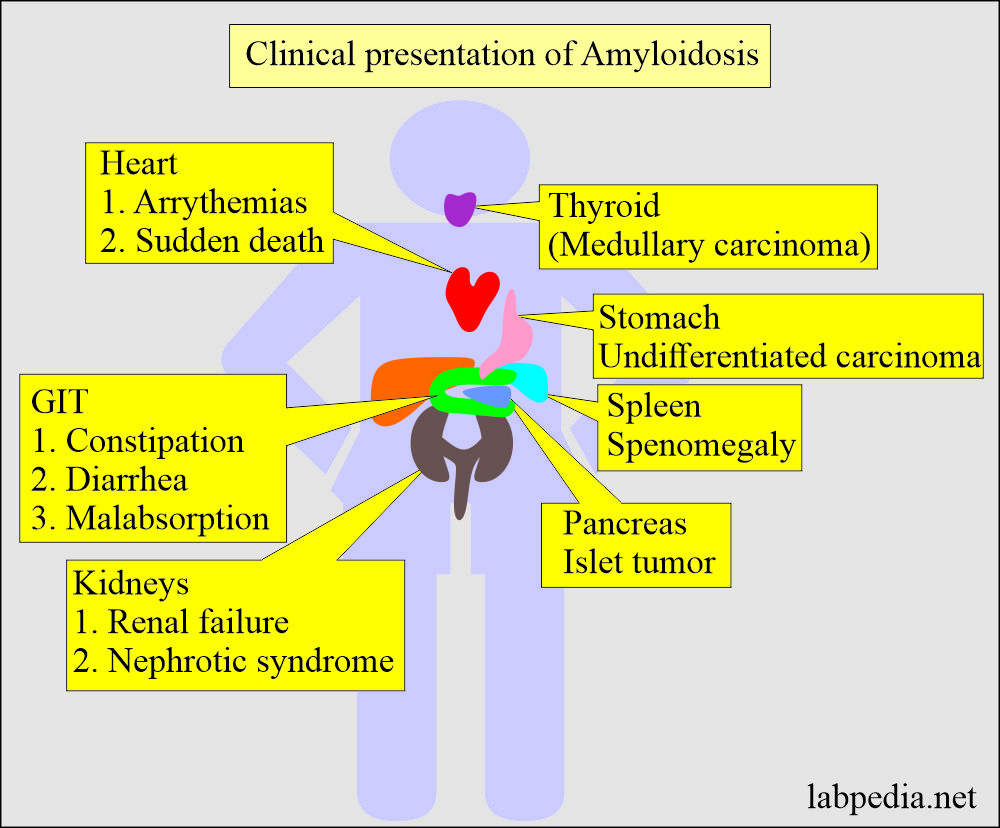
The sign and symptoms of Amyloidosis:
- Except for the familial type of amyloidosis, it is seen in older patients with an average age of 60 years.
- These depend upon the organ involved.
- There are severe fatigue and weakness.
- There is shortness of breath.
- There may be diarrhea with blood, and sometimes there is constipation.
- There may be swelling of the ankles and legs.
- The skin may show thickening or easy bruising and patches around the eyes.
- The most commonly involved organs are the Kidneys and the heart.
- There may be an irregular heartbeat.
- The patient may develop difficulty in swallowing.
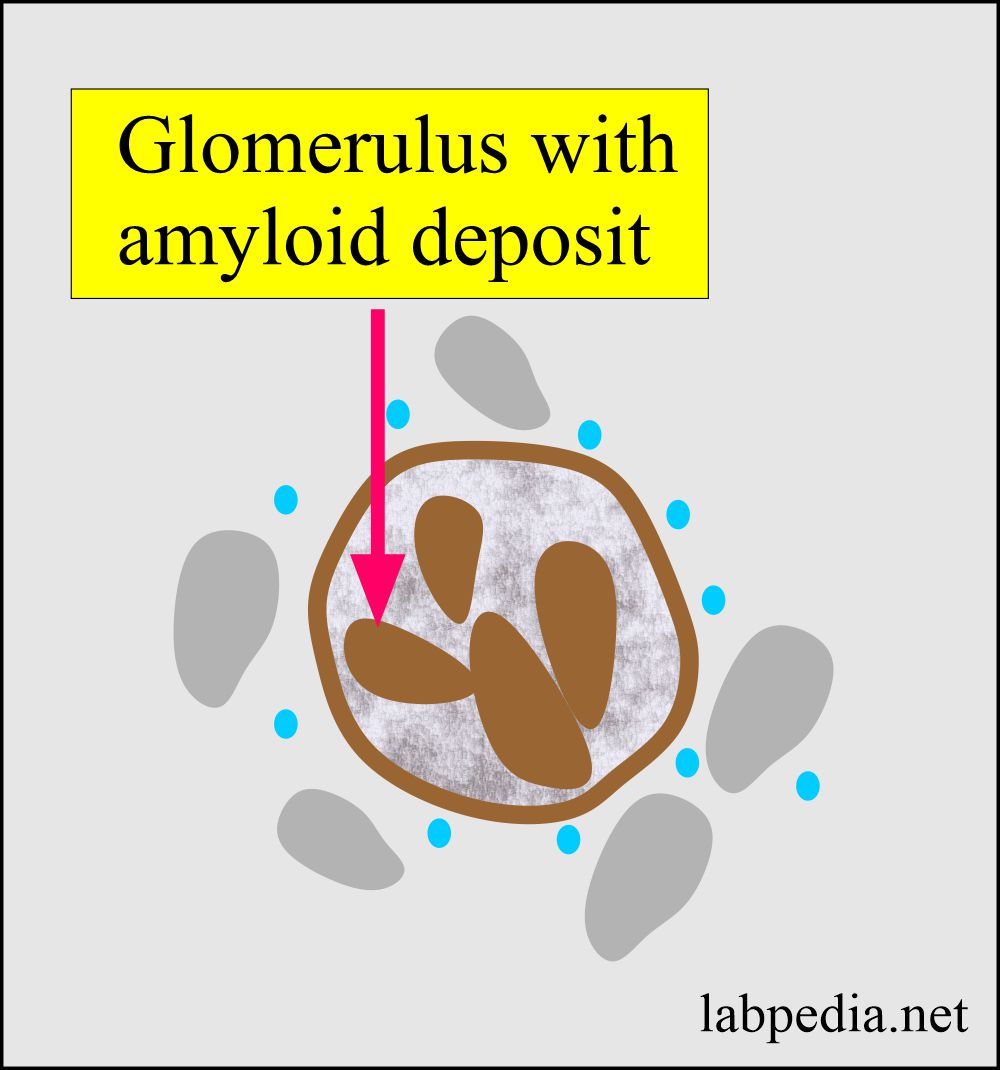
- Kidney involvement leads to nephrotic syndrome. There may or may not be raised creatinine and blood urea.
- There is the involvement of the kidney in 90 to 96 % of the cases with the amyloid type of AA.
- Immunoglobulin light-chain associated (AL) Amyloidosis:
- This primary amyloidosis gives the S/S of the organ involved.
- Kidneys’ involvement will show proteinuria and nephrotic syndrome.
- The cardiovascular system shows cardiac failure.
- Carpal tunnel syndrome with weakness and paresthesia of the hands may be an early feature.
- Sensory neuropathies are common.
- On physical examination shows, hepatomegaly, rarely splenomegaly, cardiomyopathy, polyneuropathy, and bruising may be seen.
- Macroglossia may be seen in 20% of the cases.
- Familial transthyretin-associated amyloidosis (ATTR):
- There is peripheral sensorimotor and autonomic neuropathy is more common with symptoms of diarrhea and weight loss.
- Macroglossia is not seen in this type.
- Cardiac dysfunction is of conduction.
- Reactive or secondary (AA) amyloidosis:
- This is usually due to chronic inflammatory conditions like rheumatoid arthritis, inflammatory bowel disease, and untreated Mediterranean fever.
- It has been seen in patients with tuberculosis, bronchiectasis, and osteomyelitis in developed countries.
- Local amyloidosis: There is a local deposit of amyloid fibrils in various organs like the skin, heart, and brain.
- In cerebral amyloidosis: There are intracerebral and cerebrovascular amyloid deposits seen in Alzheimer’s disease.
- In hereditary spongiform encephalopathies, several cerebral amyloid plaques are seen.
Risk factors leading to amyloidosis:
- Age, the most common age group involved is 50 or older people except for the younger age group.
- In family history, some amyloidosis is hereditary.
- Sex, the majority of the patients are male.
- Dialysis of the patient also leads to amyloidosis.
- Chronic diseases predispose to amyloidosis.
The complication of amyloidosis:
- The kidney, when involved, will ultimately lead to renal failure.
- Kidney size may be normal or enlarged.
- Amyloid deposits in the glomeruli.
- Amyloidosis is also seen in the interstitium and the wall of blood vessels.
- The cardiovascular system leads to heart failure and arrhythmias.
- The heart size may increase from minimum to moderate enlargement.
- Amyloid deposits are found in the myocardium.
- The spleen may be enlarged moderately to a large size.
- Amyloid deposit is limited to splenic follicles and gives sago spleen appearance.
- Liver amyloidosis causes massive enlargement.
- The amyloid deposit first appears in the space of Disse.
- Later on, encroach the adjacent liver parenchyma.
- In late stages involve, the sinusoids.
- The Central nervous system leads to various types of complications like diarrhea, constipation, numbness of fingers, and dizziness.
Diagnosis of Amyloidosis:
- Take a biopsy from the clinically affected tissue.
- Congo-red test: Congo-red binds the amyloid and gives apple-green fluorescence under polarized light. This test is positive in one-third of the primary amyloidosis and about two-thirds of the secondary amyloidosis of patients.
- Fat aspiration from the subcutaneous tissue showed positivity in 75% of the cases.
- 85% positive in the AL amyloidosis from the abdominal subcutaneous fatty tissue.
- Gingival and rectal biopsy is positive in one-half to two-thirds of patients.
- In the case of kidney involvement, a needle biopsy of the kidney is needed.
- Bone biopsy is positive in 30% of the multiple myeloma cases.
- Live needle biopsy may be positive.
- In case of skin involvement, take the biopsy from the plaques.
- In carpal tunnel syndrome, a biopsy from the carpal tunnel tissue is positive in 90% of the cases.
- The biopsy may be taken from involved areas like GIT, spleen, and respiratory system.
- Immunohistochemical staining shows the reaction of fibrils with Kappa (κ) or lambda (λ) antisera.
- E/M is the most specific for the diagnosis of amyloidosis.
- Bone marrow may show increased plasma cells in primary amyloidosis or lymphoproliferative disorders.
- Urine may show proteinuria and light chains in AL amyloidosis.
- There may be paraproteinemia.
- Scintigraphy using the 123I-labelled serum amyloid P component is useful for diagnosing AL, ATTR, and AA amyloidosis. But this test is not available in most of the labs.
Treatment of Amyloidosis:
- There is no definite treatment or cure for amyloidosis.
- But treatment can limit the production of amyloid protein.
- There is a symptomatic treatment for nephrotic syndrome and cardiac failure.
- Colchicine may be helpful for familial Mediterranean fever.
- Chemotherapy may show some benefits in AL amyloidosis.
Prognosis of Amyloidosis:
- It depends upon the type of amyloidosis and the organ involved.
- In generalized amyloidosis, the prognosis is poor, with mean survival after diagnosis of 1 to 3 years.
- Microscopic and focal deposits in older people are of no clinical significance.
- Widespread deposits are progressive and fatal.
- AL Amyloid patients with cardiac involvement have a worse prognosis; in untreated cases, is less than the survival is one year.
- AA amyloid patients survive 2 to 4 years.
- ATTR amyloid patients survive for 15 years.
- For patients with multiple myeloma-associated amyloidoses, the prognosis is poor.
- Treatment is aimed at:
- Reducing the supply of precursor protein.
- Treat the bleeding problem.
- Increase motility.
Questions and answers:
Question 1: What is the special stain for amyloidosis?
Question 2: What is the best site for the diagnosis of amyloidosis?