Entamoeba Histolytica (Amebiasis), Life cycle, And Diagnosis
Entamoeba Histolytica (Amebiasis)
What sample is needed for Entamoeba Histolytica?
- Take a fresh stool sample.
- Examine the stool when it is still warm.
- Rectal scrapings can also be used.
- In a dysenteric stool, take the sample from the blood and mucus on the slide and cover it with a cover glass.
- Then, press gently on the cover glass with tissue paper to get a thin preparation.
How will you define Entamoeba Histolytica?
- Amoeba is a Greek word meaning “to change.” It has two forms:
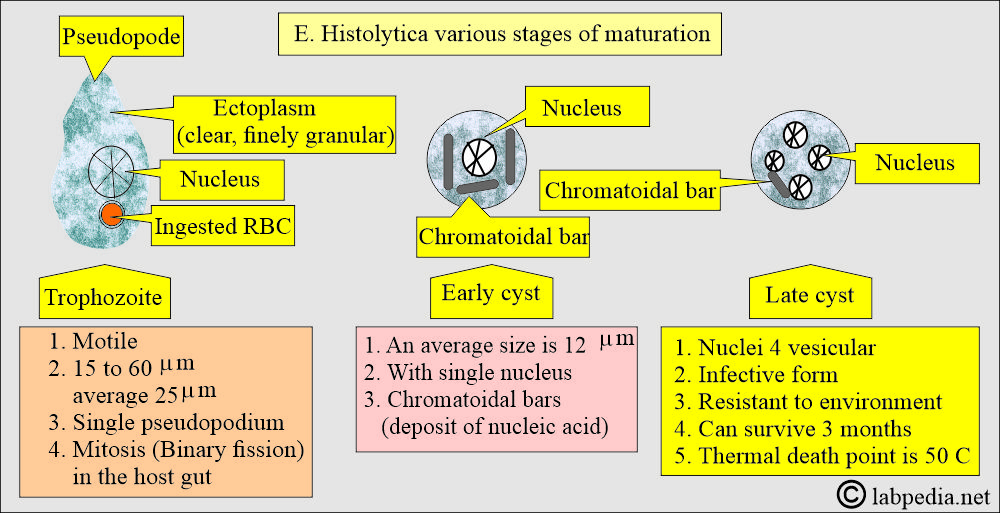
- Trophozoite:
- Its form is a Latin word meaning “to nourish.” It represents the motile, living, feeding stage in humans.
- Cyst:
- Its form is the nonmotile, resting, and infective stage. Cysts can survive outside (around 3 months) and resist the environment.
- Unicellular organism:
- E. histolytica is a unicellular organism with a single-nucleus protozoan.
- It infects 10% to 12% of the world’s population.
- The majority of cases are in the tropics.
- This is common in male homosexuals, 20% to 32%.
- Entamoeba Histolytica causes amoebiasis. This is from histo (tissue) and lysis (destruction).
How do you define amebiasis?
- Amoebiasis presentation may be:
- Intestinal amebiasis (Intestinal dysentery).
- Many patients are asymptomatic.
- The virulent organisms cause amoebic dysentery (abdominal pain and diarrhea with cramping).
- Extraintestinal amebiasis leads to the involvement of the liver and, rarely, other organs.
- In the liver, it may cause an abscess (amoebic abscess, anchovy paste-like material).
- It may involve other organs like the spleen, lungs, and brain.
What does the genus Entamoeba Histolytica include?
- The genus Entamoeba includes:
- Commensals are:
- E. gingivalis.
- E. coli.
- E. hartmani.
- E. dispar.
- Pathogenic are:
- E. histolytica.
- The cysts are passed in the stool.
How will you Compare Human Enteric amoebae?
Amoeba in human E. Histolytica E. Coli E. gingivalis Endolimax nana Iodoamoeba butschlii Dientamoeba fragilis Trophozoite
Size of trophozoite 25 µm (15 to 60) 25 µm (15 to 40) 15 µm (5 to 35) 9 µm (5 to 14) 10 µm (6 to 25) 10 µm (6 to 25) Motility of trophozoite - Active
- Directional
- Progressive
- Sluggish
- Nondirectional
- Nonprogressive
- Moderately active
- Progressive
- Like E.Coli
- Like E.Coli
- Active
- Progressive
Nucleus after stain - Delicate envelope
- Chromatin central
- Endosome
- Course envelop
- Chromatin eccentric
- Endosome
- Similar to E. Histolytica
- Large endosome
- No peripheral chromatin
- Large endosome
- Surrounded by granules
- Similar to E. Histolytica
- The endosome is divided into 4 to 6 granules
Pseudopodes - Finger-like, explosive
- Short, blunt
- Broad and slow
- Blunt
- Rapidly formed
- Similar to E. Coli
- Similar to E. Coli
- Thin, leaf-like
- Multiple, rapidly formed
Cyst Size of Cyst 12 µm (10 to 20) 17 µm (10 to 30) None 9 µm (5 to 14) 10 µm (5 to 18) None Inclusion of glycogen Diffuse Ill-defined None Absent Large mass None Nuclei 1 to 4 1 to 8 None 1 to 4 1 Chromatoidal bar In young cysts, the rounded ends In young cysts, splintered ends Occasional granules Usually absent
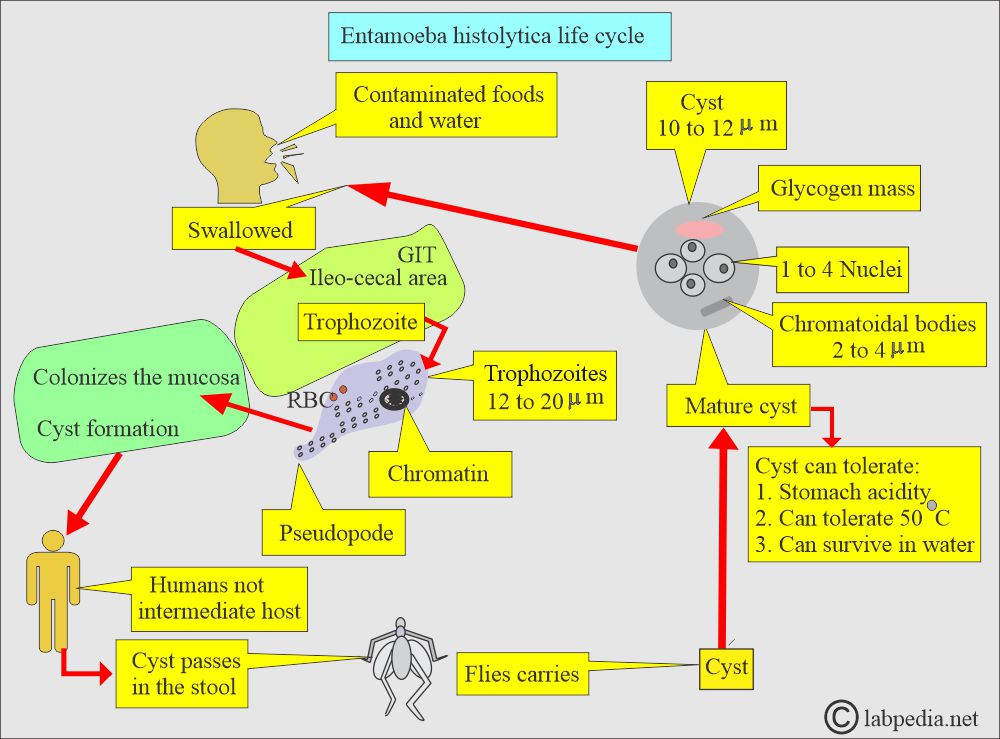
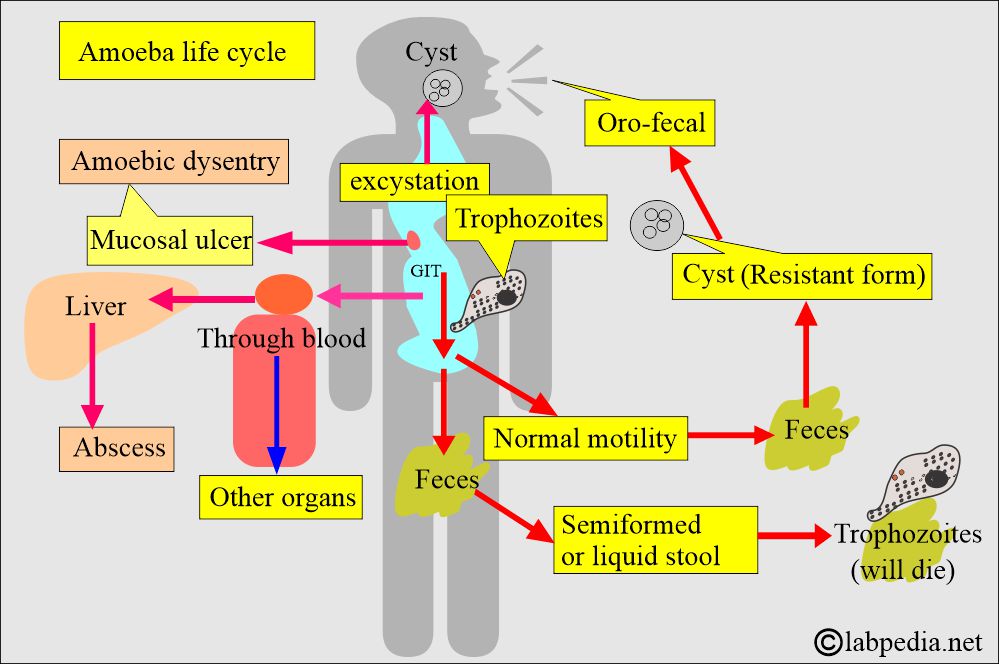
How would you discuss the Oro-fecal mode of spread?
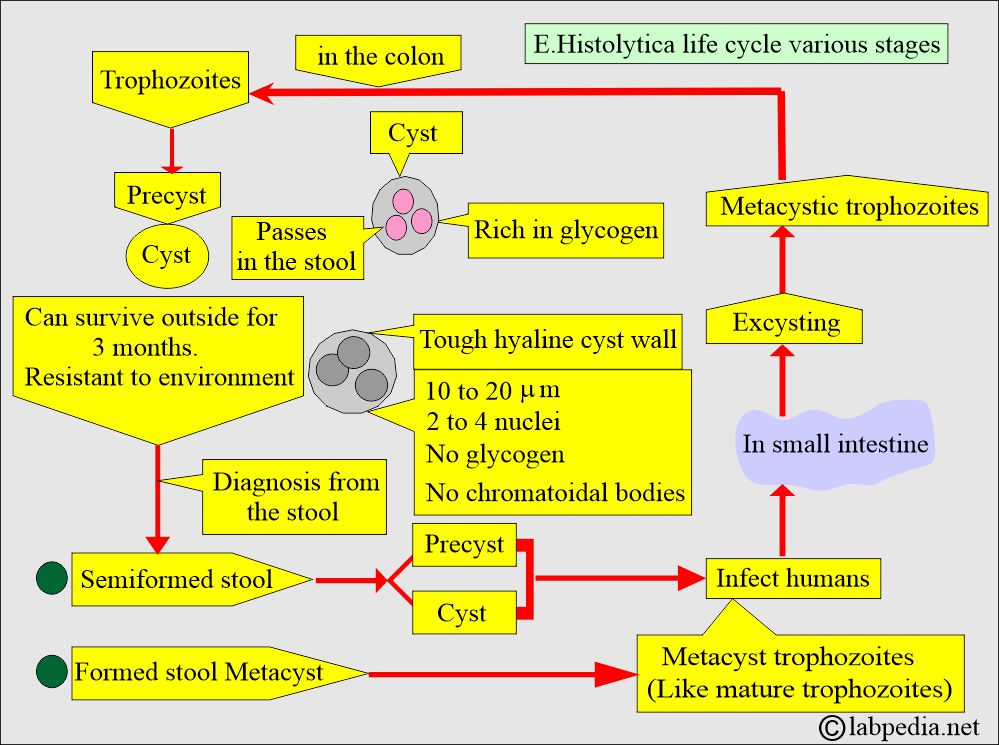
How will you discuss the Cystic stage?
- These cysts are ingested and enter the lower part of the small intestine.
- These cysts can survive in the atmosphere for almost 3 months. These cysts are resistant to the environment.
- Under the influence of the enzymes, a cyst disintegrates and forms a quadrinucleate amoeba.
- The amoeba may escape through the wall and form 8 trophozoites.
- A cyst is resistant to desiccation and even to some chemicals like chlorinated compounds and fluorides.
- The cyst can survive in water for a month, while those in feces on land can survive for more than 12 days (another reference says 3 months).
- The cyst can tolerate temperatures up to 50 °C.
- The cyst can tolerate the stomach’s acidity and reach the small intestine, the ileum, where excystation occurs. An intestinal alkaline medium is good for excyctation.
- After excyctation, the tetranuclear organism undergoes mitosis, giving rise to 8 small metacystic trophozoites.
- These will move to the large intestine, where they feed, grow, and reproduce.
- These will settle in the cecal area.
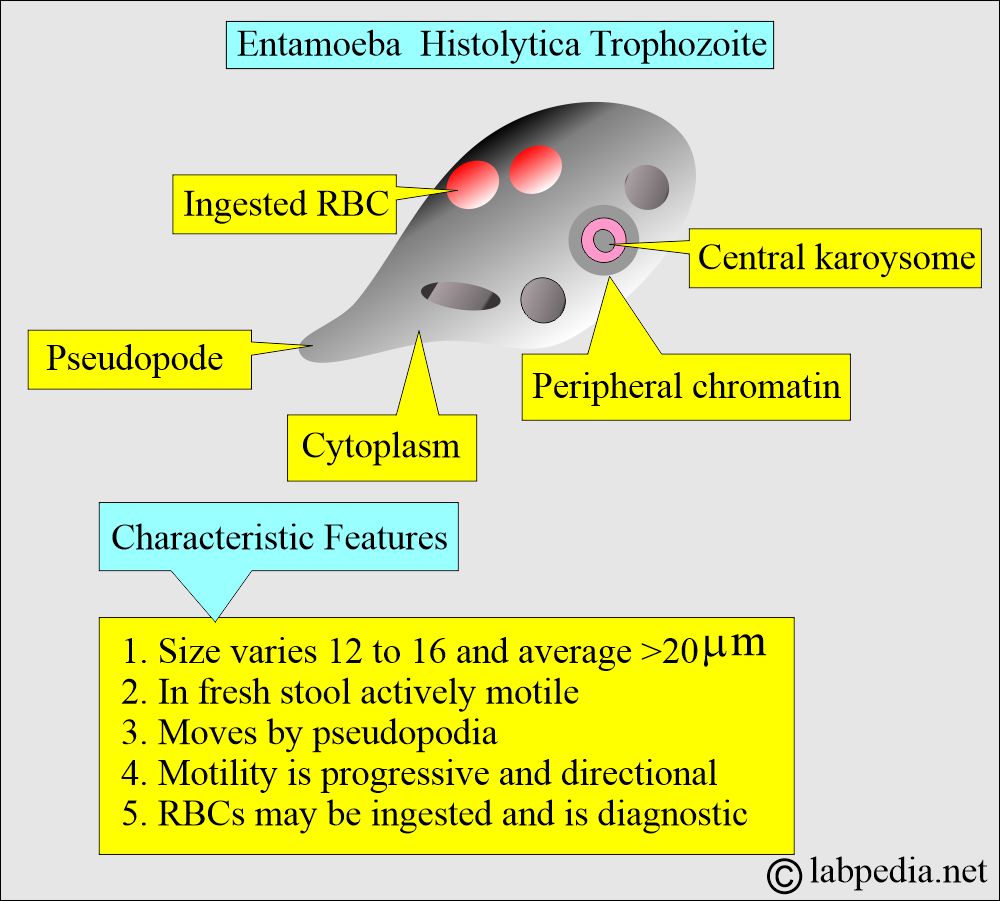
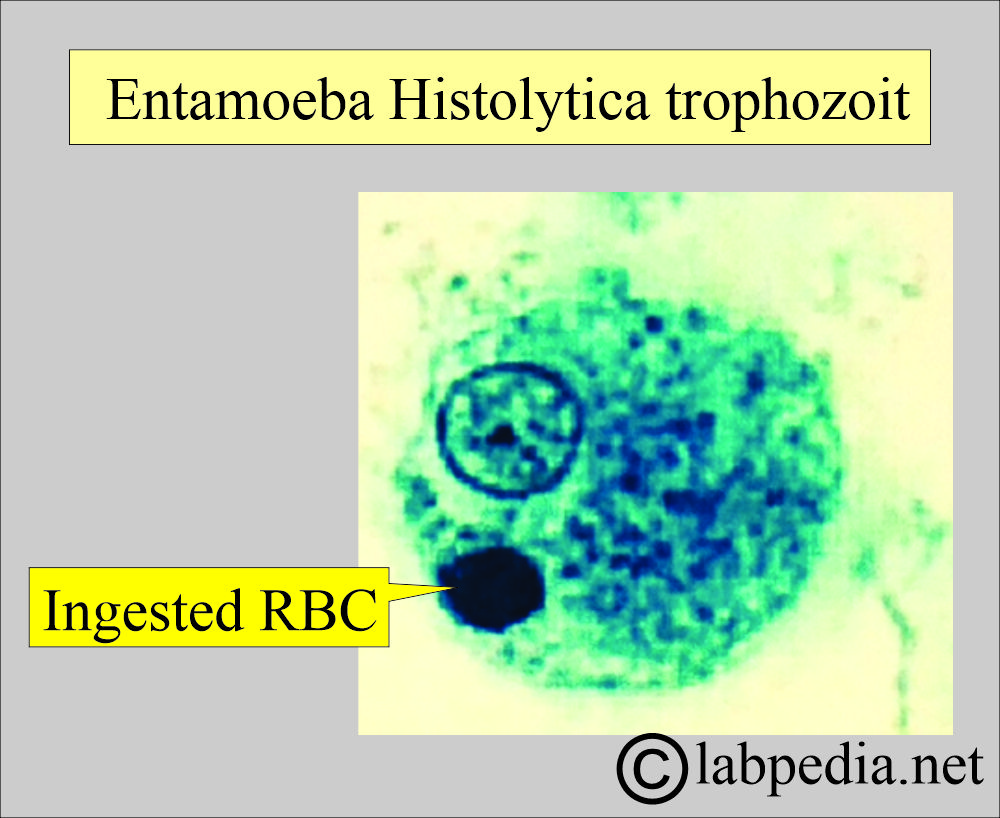
How will you discuss the trophozoite stage?
- Trophozoites migrate to the large intestine and establish infection in the colon (the cecum is the most common site).
- In the intestine, trophozoites form the flask-shaped ulcer.
- From these ulcers, the trophozoites may enter the bloodstream and form extra-intestinal abscesses.
- Trophozoites live in the intestinal lumen.
- They invade the crypts and feed on RBCs.
- Ultimately, form the ulcer.
- Trophozoites enter the blood and spread to distant organs, such as the liver.
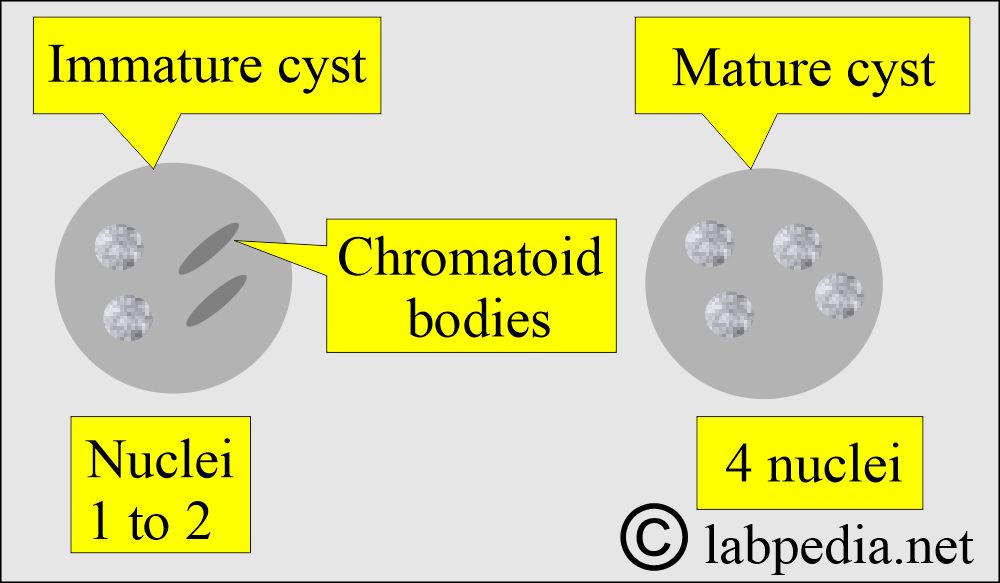
- Trophozoite transforms into the precyst with two nuclei and chromatoid bodies.
- The precyst transforms into a cyst containing approximately 4 nuclei.
- Trophozoites transform into cysts and are passed in the stool.
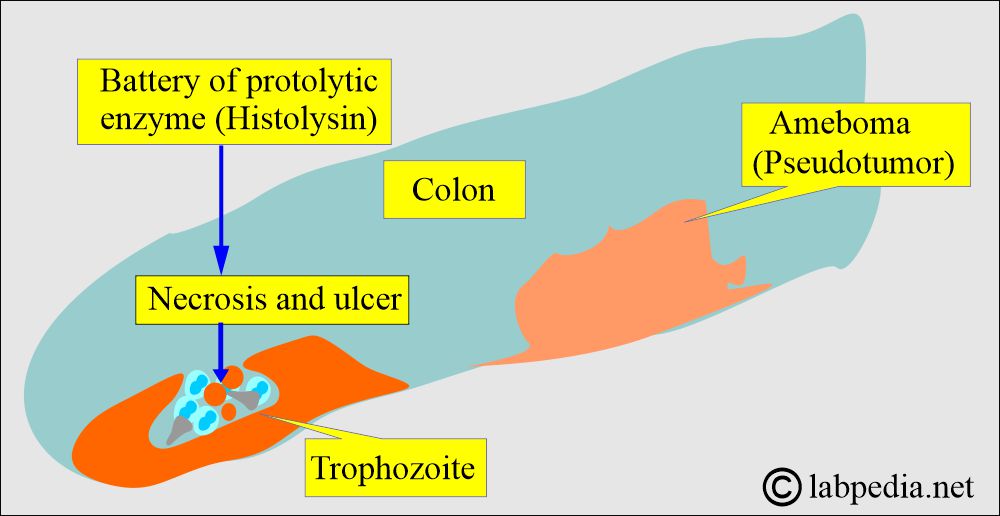
How will you discuss the pathogenesis of amebiasis by E. Histolytica?
- Trophozoites cannot survive outside, so they are not infective, unlike the cysts.
- Trophozoite moves in the intestine.
- They can eat bacteria.
- They can eat protozoa.
- They can eat intestinal cells.
- They can ingest RBCs into their body.
- E. Histolytic secretes a battery of enzymes; one of these is called histolysin, which will enable trophozoites to invade the submucosal tissue.
- In the infected person who develops dysentery, the mucosal ulceration deepens and destroys a vast area of the intestine. The overlying epithelium sloughs off and exposes the necrotic area.
- The destructive process is usually followed by a regenerative process, leading to the thickening of the wall due to fibrosis.
What organs are damaged by amoeba (Entamoeba Histolytica)?
- Trophozoites enter the portal circulation and may cause liver abscesses.
- This may give rise to hepatic amoebiasis and even amoebic hepatitis.
- The hepatic abscess may be single or multiple.
- From there, it can cross the diaphragm and form a lung abscess.
- Other organs involved are the heart, brain, spleen, gonads, and skin, which cause secondary amoebiasis.
- Flies and cockroaches are responsible for mechanical vector transmission.
How will you discuss the Host-protective mechanism of Entamoeba Histolytica?
- Little is known about the host-protective mechanism in amoebiasis.
- These patients have serum antibodies.
- These serologic antibodies can be used to diagnose amoebiasis.
- Their role in protection is not clear.
- Trophozoites activate the complement system via both the alternative and classical pathways.
- Complement is amoebicidal, but the pathogenic strains are resistant to complement-mediated lysis.
- How will you classify E. Histolytica?
- E. Histolytica has two different enzymes on analysis and is divided on that basis into:
- One of the strains can invade the tissue (10% of the lesions), and cause diarrhea with or without mucosal ulceration. This strain can enter the bloodstream, produce liver abscesses, and involve other organs.
- The second strain is the most common, and this can be asymptomatic and cause mild diarrhea, which is usually not severe.
How will you discuss the epidemiology of Entamoeba Histolytica?
- E. histolytica was first described in 1875 by a young Russian peasant in the port of Arkhangelsk.
- This was discovered in 1873 by the clinical assistant D.F. Losch in St.Petersburg, Russia.
- He found abundant amoeba in the stool of the peasant.
- His discovery was confirmed after 40 years.
- This is a cosmopolitan disease.
- Nearly 500 million people are infected, and roughly 100,000 die per year.
- Amoebiasis is the third most common cause of parasitic death worldwide.
- Distribution is more closely related to inadequate environmental sanitation and poor personal hygiene.
- It is not related to climate.
- It is considered that Entamoeba histolytica infects 10% of the world’s population.
- The actual prevalence is maybe 1% of the world population.
- This disease is more common in tropical and subtropical countries with poor sanitation.
- It is endemic in many parts of tropical and subtropical Africa, Asia, Mexico, China, and South America.
What is the Mode of spread of Entamoeba Histolytica?
- The feco-oral route involves ingestion of the infective cyst via food, water, or contaminated hands.
- Asymptomatic carriers are individuals with cysts and trophozoites that lack ingested RBCs.
- Active disease is characterized by trophozoites ingesting RBCs.
What is the clinical presentation of Entamoeba histolytica (Amebiasis)?
- WHO (1969) classified amoebiasis into the following categories:
- Asymptomatic infection.
- Symptomatic infections:
- Intestinal amoebiasis:
- Dysentery.
- Nondysenteric colitis.
- Extraintestinal infection:
- Hepatic infections:
- Acute nonsuppurative hepatitis.
- Liver Abscess.
- Pulmonary abscess.
- Extraintestinal involvement is rare in other areas.
- Hepatic infections:
- Intestinal amoebiasis:
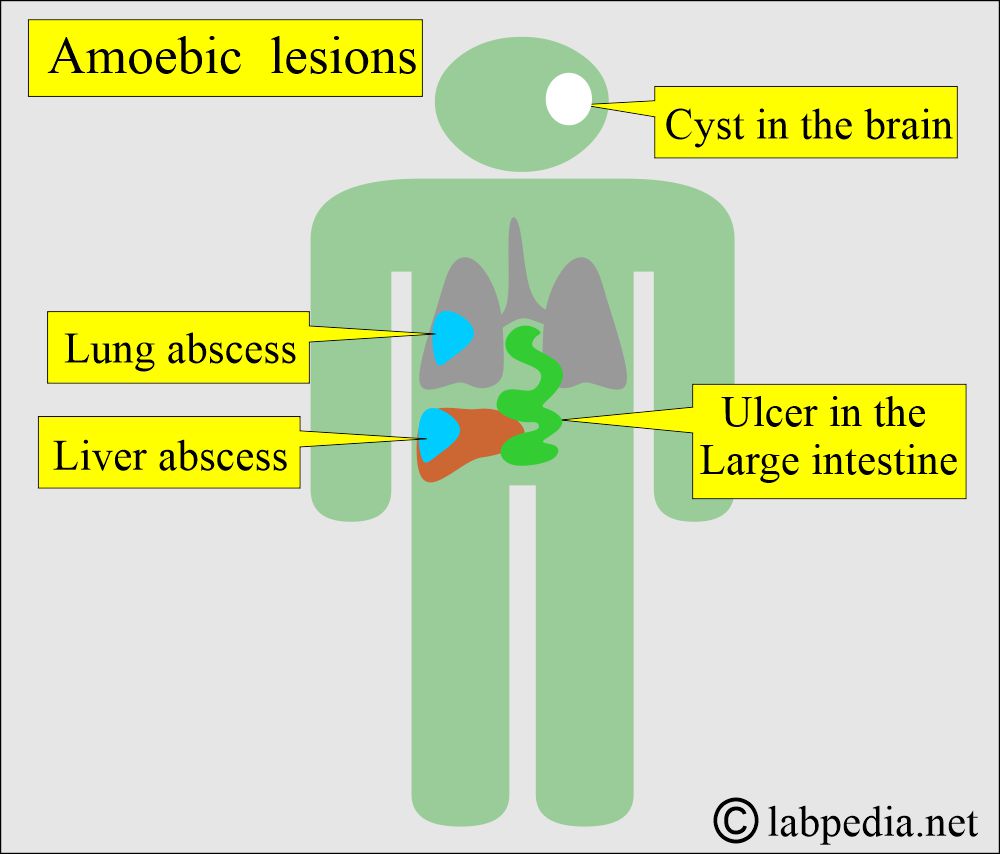
Amoeba lesions (Entamoeba Histolytica lesion)
- Invasive amebiasis has two types of presentation:
- Acute Amebic dysentery or acute intestinal amoebiasis:
- It is severe diarrhea with blood and mucus in the liquid stool.
- There is usually an incubation period of 1 to 4 weeks, accompanied by a fever of 100 °C to 102 °C.
- This is diagnosed by finding the characteristic trophozoites or cysts in the stool.
- Chronic amebiasis:
- There may be continuous attacks of diarrhea or recurrent attacks with intervening periods of mild intestinal problems.
- Amoebic dysentery is less acute than bacillary dysentery.
- The patient may have dysentery (amoebic dysentery).
- Nonspecific abdominal symptoms.
- There is diarrhea, dysentery, abdominal pain, and cramping in acute amoebiasis.
- There may be flatulence, anorexia, weight loss, and chronic fatigue.
- There may be abdominal cramps and bloody diarrhea.
- This parasite can cause mucosal ulceration.
- This can give rise to amoebic liver disease (amoebic abscess). This will be accompanied by fever and abdominal pain.
- Amoebic colitis presents no bloody diarrhea and no abdominal cramps.
- There is ulceration of the large intestine, penetrating the submucosal layers and ultimately reaching the muscle.
- A proliferation of histiocytes and connective tissue leads to granuloma formation, especially in the cecum and sigmoid colon, a condition known as Amoeboma.
- The most frequent sites are the cecum, the ascending colon, and the rectosigmoid colon, but any segment of the colon may be involved.
- There may be mild diarrhea alternating with constipation.
- This amoeboma may give rise to intestinal obstruction.
- Acutely ill patients usually have normal WBC counts and Hb levels and are afebrile.
- Patients with severe amoebic colitis or amoebic liver abscess will show leucocytosis 10,000/cmm to 20,000/cmm and mild anemia. These patients may have a low-grade fever.
- Amoebiasis usually does not produce eosinophilia.
- E. Histolytica has been seen rarely in cerebral, optic nerve, and facial infections, with severe consequences.
How will you do a laboratory diagnosis of Entamoeba histolytica?
- Stool examination: Examine fresh stool. You can use direct stool smear and concentration methods, such as zinc sulfate floatation or the formalin-ether technique.
- Find motile trophozoites in the fresh warm stool or trophozoites and cysts in the fixed stool specimen.
- Use stool examination for three consecutive days unless positive results are found.
- How to make a good thin smear:
- Using a wire loop, take a small amount of blood and mucus on one side of the slide.
- Cover it with cover glass without saline addition and press gently to make a thin smear.
- Make another slide with the eosine drop. Mix and cover with a cover glass.
- Eosin does not stain living amoebae, but the motile amoebae are in the pink background.
- Examine the preparation immediately.
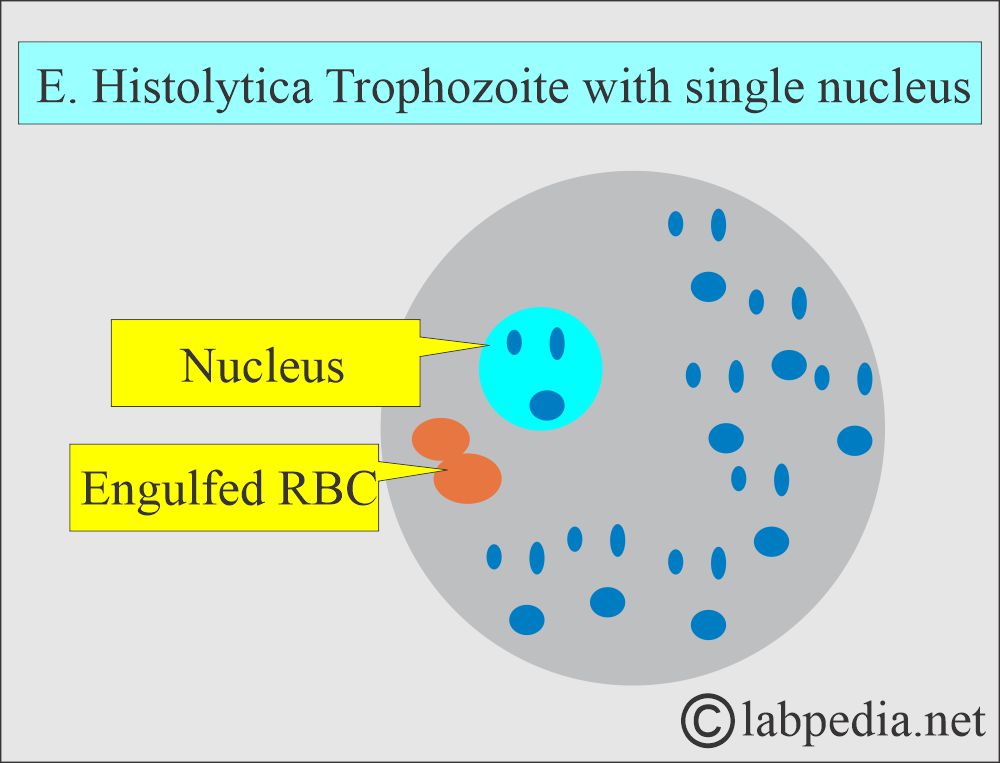
- Can see trophozoites measuring 15–20 µm with a small central nucleus. There may be the inclusion of RBC in the cytoplasm. Occasionally, bacteria may be seen.
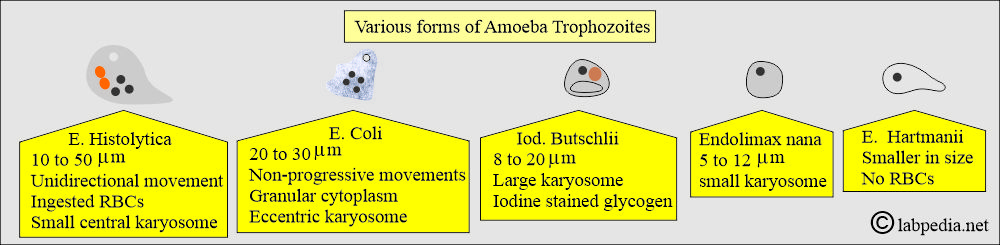
- Trophozoite of E. histolytica shows characteristic features:
- The average size is around 20-25 µm.
- It shows only active amoeboid movements, seen only in fresh, warm stool.
- Amoeba shows ingested RBC, and this is diagnostic.
- There is a single nucleus with a central karyosome.
- Trophozoites move in one direction and have an invisible nucleus in a fresh stool saline mount. The cytoplasm contains RBCs but no bacteria; the possible diagnosis is E. Histolytica.
- If the trophozoite does not move in one direction, it has an occasionally visible nucleus in the saline mount smear. The cytoplasm is granular, with bacteria but no ingested RBCs; the possibility is E. Coli.
- If >50% of the trophozoites have two nuclei, the possibility is Dientamoeba fragilis.
- Trophozoites <12 µm are possibly Endolimax nana with a large karyosome.
- Macrophages in freshly mounted slides are nonmotile and contain RBCs and bacteria.
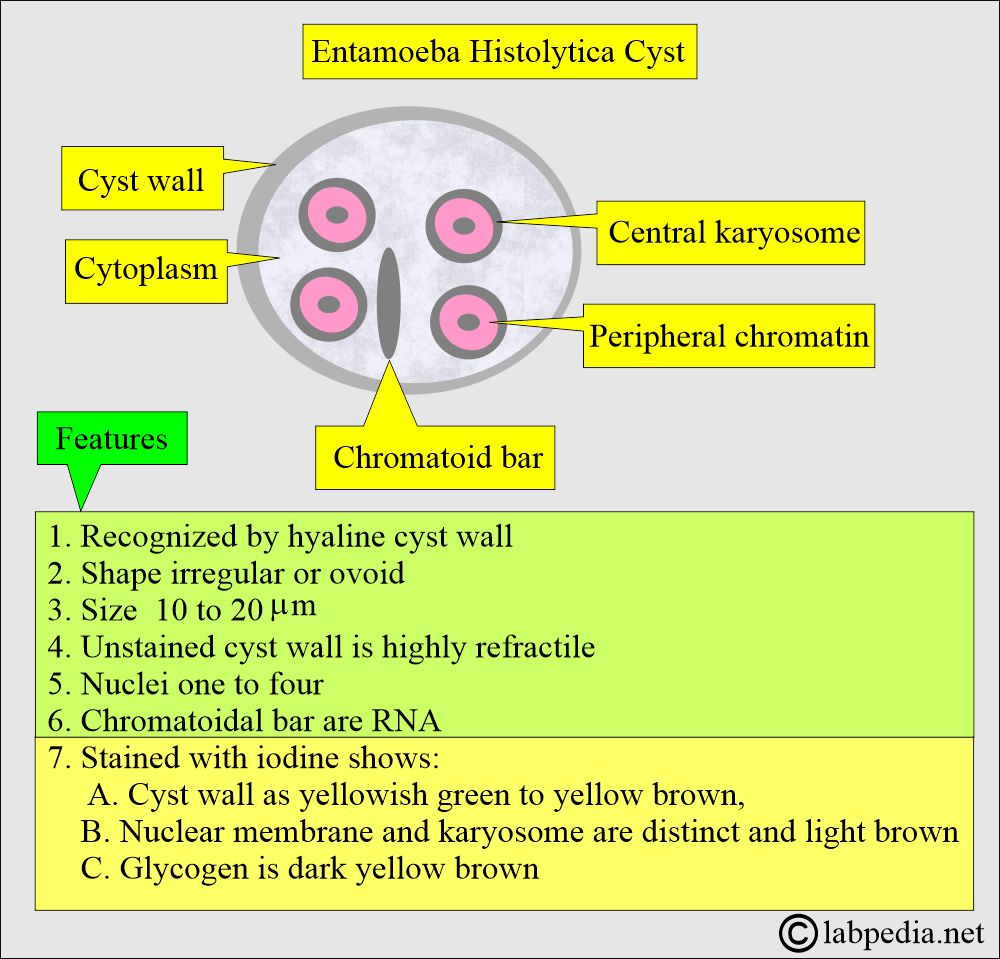
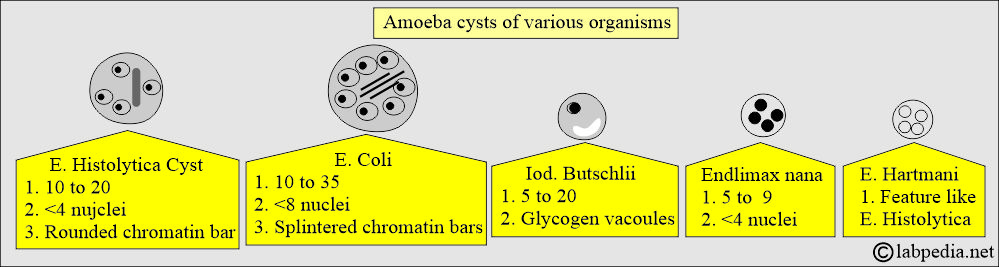
- Cyst of E. histolytica shows characteristic features:
- It is round, measuring 10 to 15 µm (>10 µm).
- It contains 1 to 4 nuclei with small karyosomes and rounded chromatoidal bars.
- Immature cysts may have 1 to 2 nuclei.
- The mature cyst may have around 4 nuclei.
- Chromatoid bodies can usually be seen in immature cysts.
- These will not stain with iodine.
- Staining these bodies requires special stains, such as Burrow’s or Sargeant’s.
- The E. Coli cyst has 8 nuclei, small karyosomes, and splintered chromatoidal bars.
- Cysts <10 µm are either E. nana, which will have 4 nuclei and large karyosomes.
- E. harmani has 4 nuclei and a small karyosome.
- Iod. butschlii has 1 to 2 nuclei and large iodine-stained glycogen vacuoles.
- How will you classify Amoeba cysts?
- Amoeboid movements may be seen, which is characteristic.
- Wet-mount preparation of a formalin-ethyl acetate concentrate of stool. This smear can be stained with D’Antoni’s iodine.
- Gomori’s stain is used and is very helpful.
- The serological test is used to diagnose amoebiasis. The antibody-dependent test is done by EIA.
- Antigen-dependent tests are also available.
- Various ELIZA methods are also used.
- Intestinal amoebiasis, asymptomatic cases, can be detected in 10%.
- Carriers with mild diarrhea can be detected in <50% of the cases.
- Patients with invasive amoebiasis are detected in 85% to 90% of the cases.
- ELIZA, IHA, and LA tests are more sensitive than gel diffusion.
How will you treat Entamoeba histolytica (Amebiasis)?
- The drug of choice is Metronidazole. This can be supplemented by iodoquinol.
How will you prevent and control the disease (Amebiasis)?
- Avoid fecal contamination of the environment using closed latrines.
- Avoid contamination of the water supplies from fecal material.
- Always wash your hands with soap at least 3 times after defecation.
- Wash your hands before you start eating.
- Control the spread of disease by flies that act as cyst carriers.
- Protect food from cockroaches.
- Boil water at 55 °C, and E. histolytica cysts are killed.
- Avoid uncooked and green salad, which may contain cysts.
- Thoroughly wash the fruits and vegetables.
- Health education, particularly for food handlers, schools, and community health centers.
- Avoid human feces fertilizers.
- Good sanitation for garbage disposal.
- Screen the carrier in the food industry.
Questions and answers:
Question 1: What is the % of serological tests for invasive amoebiasis?
Question 2: What is the difference between mature and immature cysts of E. histolytica?

So good notes
Thanks.
i really love this labpedia! help me a lot thankyou sooo muchh
Thanks, you are welcome.
can biologist work in clinc if undersoodn these materia?
I believe you have to attend some school for training. My website material will help you in your study.