Gliadin Antibodies IgA, IgG, Endomysial Antibodies, Celiac disease and Sprue
Gliadin Antibodies IgA, IgG
What sample is needed for Gliadin Antibodies IgA and IgG?
- Collect the venous blood to prepare the serum.
- A fasting sample is not necessary.
- An intestinal biopsy may be advised, and it gives characteristic changes.
What are the Indications for Gliadin Antibodies IgA and IgG?
- These antibodies are detected in gluten-sensitive enteropathy.
- This test is done to diagnose Celiac disease and sprue.
- These antibodies are used to monitor the disease.
- In successful treatment with a gluten-free diet, these antibodies will disappear from the serum.
What are the precautions for Gliadin Antibodies?
- Other gastrointestinal diseases like colitis, Crohn’s disease, and lactose intolerance can raise the value of Gliadin antibodies.
- Get the list of foods eaten in the last 24 hours.
How will you define Celiac disease/Sprue?
- It is also called Celiac disease, Gluten-sensitivity enteropathy, nontropical sprue, or idiopathic steatorrhea.
- Gluten-induced enteropathy includes Sprue and Celiac disease.
- Both these diseases involved duodenum and jejunum predominantly.
- The celiac disease is sometimes called non-tropical sprue, celiac sprue, or gluten-sensitive enteropathy.
- Celiac disease is an autoimmune multisystem disease.
- Celiac disease is also called childhood non-tropical sprue.
- A gluten-free diet cures the celiac disease.
- The sprue is an infectious process that is cured by antibiotics.
- Sprue is a broad, nonspecific term that describes several conditions characterized by malabsorption affecting the small intestine.
- Sprue can be referred to as nonspecific celiac disease and is also known as celiac sprue.
- It also includes tropical sprue and non-celiac gluten sensitivity.
- Tropical sprue is similar to celiac disease, but it occurs in tropical regions with different underlying causes.
- In short, Sprue is a broad term, including celiac disease and other conditions with similar symptoms and malabsorption.
How will you differentiate between Celeic disease and sprue?
| Parameters | Celiac disease | Sprue |
|
|
|
|
|
|
|
|
|
|
|
|
How will you discuss the epidemiology of Celiac disease?
- It is found predominantly in Europe and, uncommonly, in African -America.
- It is rare in Asia.
- It is 10 to 15 times more common in IgA-deficient persons.
- It is 1% to 3% in patients with diabetes mellitus type 1.
- There is an association between T-cell lymphoma and juvenile rheumatoid arthritis.
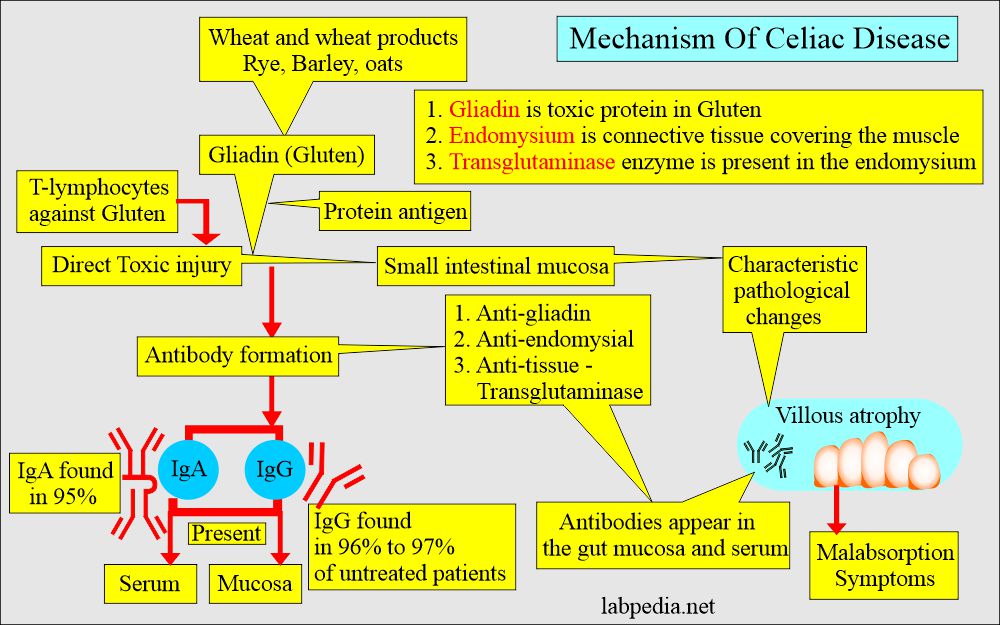
How will you discuss the pathogenesis of Celiac disease and sprue?
- Celiac disease is also called Gluten-sensitive enteropathy, Nontropical sprue, or idiopathic steatorrhea.
- Meanwhile, sprue is a broad term characterized by malabsorption, like Celiac disease.
- Gliadin is the toxic protein of gluten
What are the auto-antigens of Celiac disease?
- Gliadin is the complex of gluten and tissue transglutaminase.
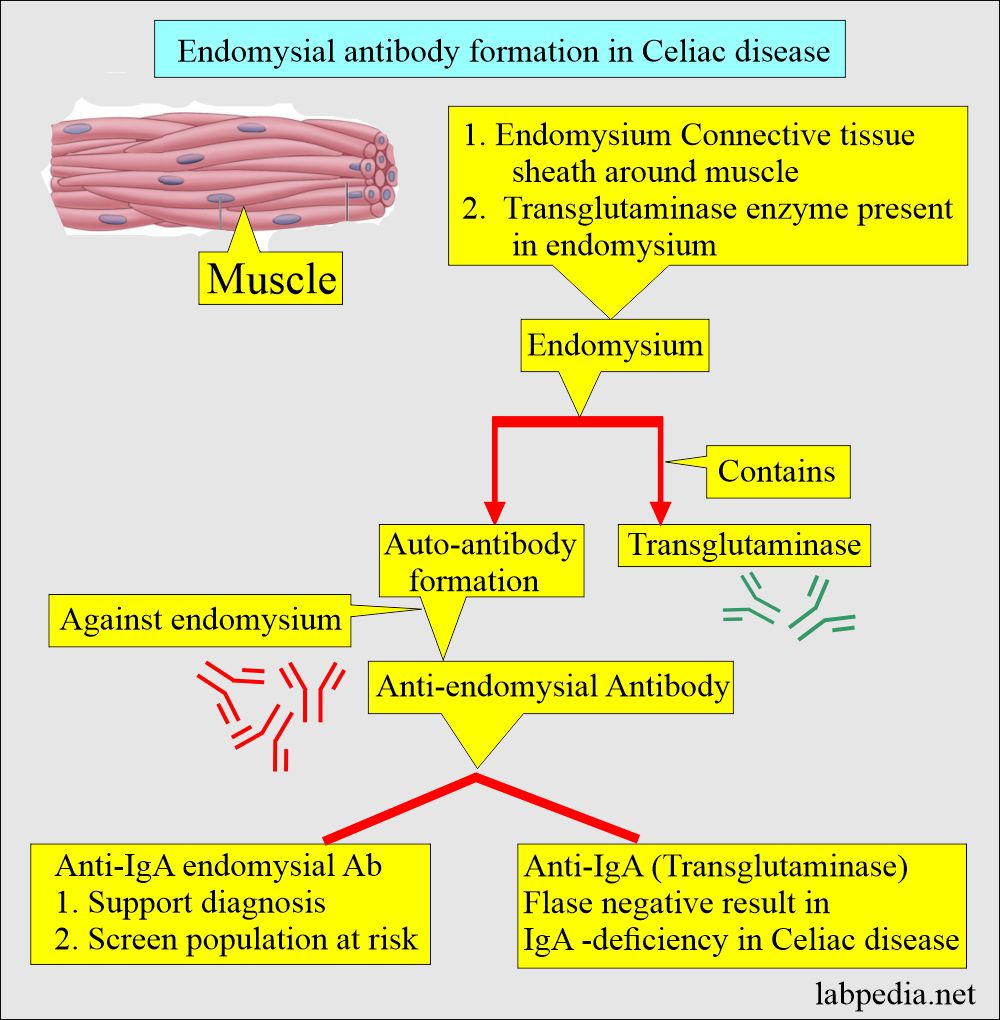
- Tissue transglutaminase is present in the thin connective tissue covering the muscles.
- Gliadin is the toxic protein of the gluten.
- Gluten = Gliadin + tissue transglutaminase.
- The small bowel (mainly duodenum and jejunum) tissue Transglutaminase is the auto-antigen.
- Pathogenesis of the disease is believed to involve an interaction between transglutaminase and the gliadin peptide in genetically susceptible people.
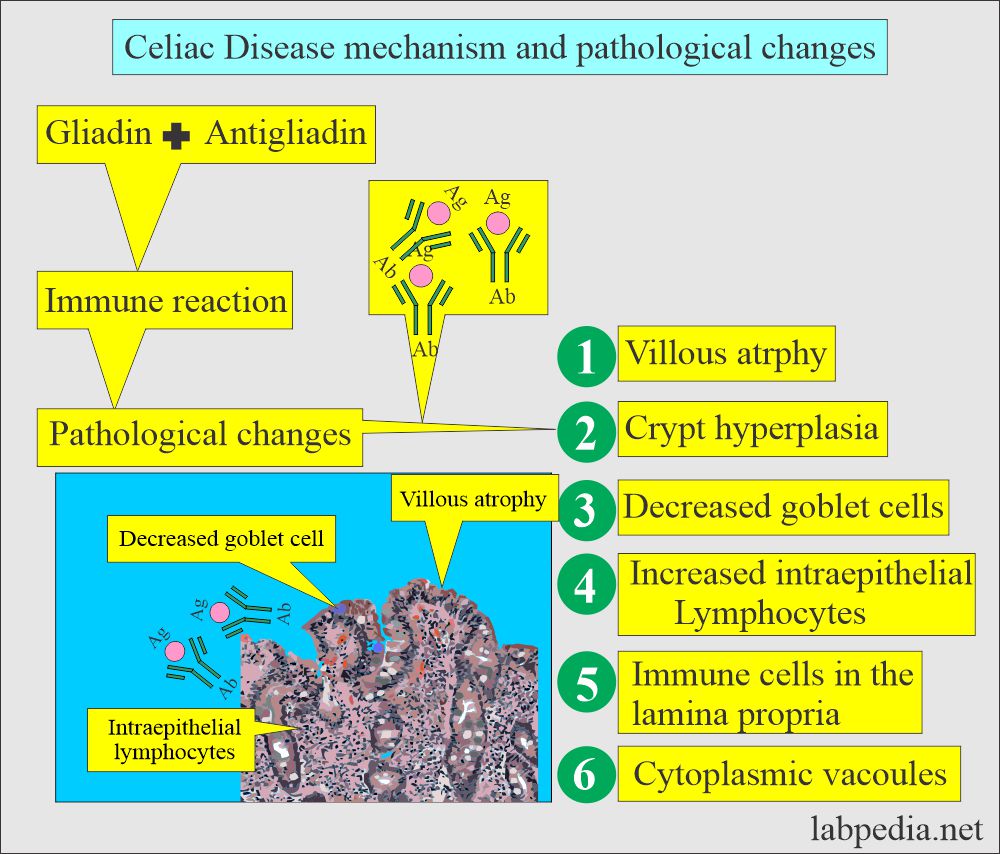
- In both conditions (celiac disease and sprue), T-lymphocytes mediate an immune reaction against gluten.
- Gluten is found in wheat, rye, barley, and maybe oats.
- There is a genetic predisposition, and it runs in families.
- 10% of the first-degree relatives have this disease.
- There is an association in HLA-DR3 in 90% of the patients and the same for dermatitis herpetiformis.
- Another reference says a genetic component is present in the HLA chromosome 6.
- The major toxic protein of wheat is gliadin.
- There is sensitivity to Gliadin (gluten), which are the proteins found in:
- Wheat.
- Wheat products.
- Rye.
- Barley.
- Possible oats.
What antibody forms in Celiac disease?
- Antibodies to gliadin are toxic agents in celiac disease.
- Patients with celiac disease cannot tolerate the proteins gliadin + gluten in wheat or wheat products.
- Gliadin + gluten is toxic to the small intestinal mucosa and leads to characteristic pathologic changes seen on biopsy.
- Endomycelium: It is a thin layer of connective tissue surrounding the muscle.
- These patients develop antibodies against:
- Gliadin = anti-gliadin antibody (IgA and IgG)
- Endomysial = anti-endomysial antibody.
- Tissue = anti-tissue transglutaminase.
- These patients have severe intestinal malabsorption.
- The only treatment for these patients is to avoid wheat and wheat products.
- These antibodies are present in the mucosa and the blood.
- The celiac disease starts in infancy when cereals are given to the baby.
- IgG-antigliadin antibody is more sensitive but less specific than IgA.
- Anti-gliadin antibodies are found in 95% of those with Celiac disease and nontropical sprue.
- Anti-IgG gliadin antibodies are found in 96% to 97% of untreated patients. 80% may have Celiac disease.
- Anti-IgA gliadin antibodies are found in 75% of the cases, and these are 95% specific for Celiac disease.
- Anti-gliadin antibodies IgG and IgA are positive in 45% to 85% of dermatitis herpetiformis.
- False positive cases are seen in ulcerative colitis and Crohn’s disease.
What are the pathological changes in Celiac disease?
There are typical changes on the intestinal (jejunal) biopsy like:
- There is villous atrophy.
- Goblet cells are decreased or absent.
- It shows crypt hyperplasia.
- Intestinal epithelial cells show vacuoles.
- The intestinal mucosa first shows blunting of the mucosal villi. . There is mild widening and shortening.
- It is followed by flattening and loss of villi.
- There is a lymphocytic infiltrate in the mucosa and submucosa. Also, these cells will infiltrate the lamina propria.
What are the signs and symptoms of Celiac disease?
- Mostly, the symptoms are seen in children when they start cereals.
- The most common presentation is:
- There is easy fatigability.
- There is abdominal bloating and pain.
- There may be vomiting.
- The patient will have chronic diarrhea.
- The stool is foul-smelling, pale, and fatty.
- Sometimes, these patients will be constipated.
- The stool is hard to flush.
- There are aphthous ulcers.
- The patient will have weight loss.
- These children are irritable.
- Delay in the growth pattern.
- Sometimes, it is difficult to thrive, and the patient may have osteomalacia.
- There is a strong association with other autoimmune diseases like diabetes mellitus type 1 and autoimmune thyroid diseases.
What are the complications of Celiac disease?
- There is anemia.
- 15% to 20% of patients develop intestinal lymphoma or adenocarcinoma.
- There is an increased incidence of gastric and esophageal carcinoma.
- There may be neuropathy.
- These patients may have hyposplenism.
What is the normal Gliadin-antibody?
- Values are given for the child of age >2 years:
- Negative = < 25 U/L .
- weak positive = 25 to 50 U/L.
- Positive = >50 U/L.
Source 6
- Gliadin IgA/IgG = 0 to 2 years = <20 EU.
- 0 to 3 years and older = <25 EU.
- Endomysial IgA = all ages = negative.
- Tissue transglutaminase IgA = all ages = <20 EU.
How will you diagnose celiac disease?
- An elevated level of anti-gliadin and anti-endomysial antibodies.
- IgA and IgG antibody sensitivity are 90% for the active untreated disease. When both antibodies are done, the specificity is also 90%.
- These antibodies will detect the following:
- Celiac disease will 100% have IgA endomysial antibodies.
- Celiac sprue.
- Dermatitis herpetiformis 70% shows IgA endomysial antibodies.
- Intestinal (jejunum) biopsy shows typical changes in villous atrophy.
- On jejunal biopsy, we will see villous atrophy.
- Increased intra-epithelial lymphocytic infiltrate.
- There is hyperplasia of the crypts.
- These changes may reverse on a gluten-free diet. This will not occur in the sprue.
- In Celiac disease, anemia may be either macrocytic or hypochromic microcytic anemia.
What are the serological tests for Celiac disease?
| Antibody | Specificity | Sensitivity |
| IgA- antigliadin antibody | 95% | 75% to 95% |
| IgA- endomysial antibody | >99% | 80% to 100% |
What are the diagnostic criteria for the Celiac disease
- Provisional diagnosis:
- Positive serological (anti-gliadin antibody) test.
- Typical pathological findings on biopsy of the small intestine.
- The confirmatory test is:
- When a gluten-free diet is given, then patients become symptom-free.
- Serological tests become in the normal range or negative.
- The pathological changes will improve or disappear if a biopsy is done.
How will you treat Celiac disease?
- Start a permanently gluten-free diet.
- Avoid wheat, barley, rye, and oats.
- Another reference excludes oats, which are allowed in the list of eatable foods. Be sure there is no wheat, barley, or rye mixing.
- Or any food containing them, like bread, cake, and pies.
- Rice, soya, potatoes, maize, jam, and sugar are allowed.
- Gluten-free flour, bread, and pasta are available.
- Try steroids if diet therapy is not helpful.
Questions and answers:
Question 1: What are the false positive conditions for Anti-gliadin antibodies?
Question 2: What is the result of Celiac disease?