Folic Acid and Folate
Folic Acid and Folate
What Sample is Needed for Folic Acid and Folate?
- Fasting venous blood is needed to prepare the serum.
- Some of the labs take a sample without fasting.
- Protect the blood from light.
- If RBC folate is needed, then blood in EDTA is taken.
- The sample is stable for 24 hours at 4 °C.
- 6 to 8 weeks at -20 °C.
- Also, perform hematocrit.
- Avoid hemolysis.
- Avoid repeated freezing and thawing.
What are the precautions for Folic Acid and Folate?
- Certain drugs decrease folic acids like Alcohol, PAS, Ampicillin, Antimalarial, Erythromycin, Methotrexate, Oral contraceptives, Chloramphenicol, Penicillins Phenobarbital, Aminopterin, Tetracyclines, and Phenytoin.
- Avoid administration of radionuclides for at least 24 hours.
- Hemolysis gives a false elevated level.
- Iron deficiency anemia gives a false increase.
- Draw blood before the administration of the B12 injection.
What are the Indications for folic acid?
- It is advised in megaloblastic anemia.
- This test is advised in the following conditions:
- To rule out the folic acid deficiency.
- In iron-deficiency anemia.
- In Hypersegmented neutrophils.
- It is advised in pregnancy.
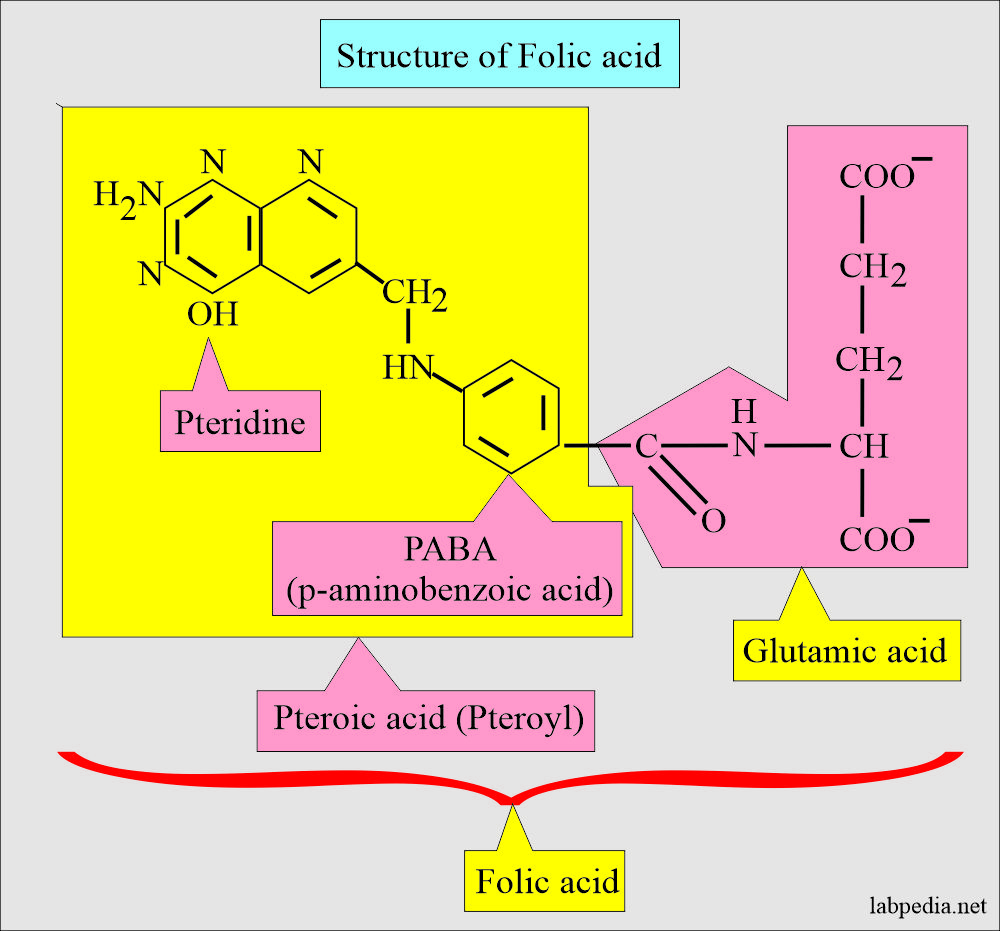
How will you define the structure of folic acid and Folate?
- Folic acid and folate are different types of vitamin B9.
- Folates are naturally occurring compounds with a structure similar to folic acid.
- Folic acid is a synthetic form given as a supplement and fortified food.
- Folic acid and Folate are used for a family of compounds related to Pteroic acid.
- Folic acid or pteroylglutamic acid is the parent compound of the folate complex.
- Folacin is the generic term for folic acid and related substances that have the activity of folic acid.
- Folic acid or folates consists of:
- A pteridine is a base.
- It is attached to one molecule of p-aminobenzoic acid.
- And glutamic acid.
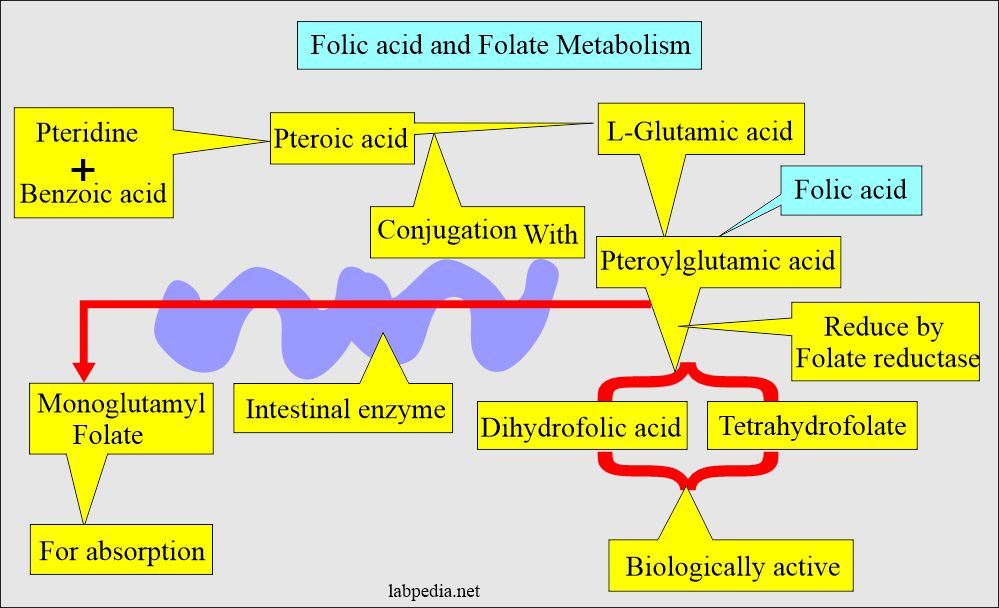
- Pteridine and p-aminobenzoic acid are called Pteroyl.
- The rest of the names are given according to the number of glutamic acids, such as pteroyl monoglutamate or pteroyl polyglutamate.
- Folic acid /folates are a generic term for a family of compounds that function as coenzymes for processing one-carbon units.
- Another definition:
- Pteroic acid, combined with one molecule of L-glutamic acid, will form pteroylglutamic acid (Folic acid).
- It will reduce to dihydrofolic acid or tetrahydrofolate. These reduced forms are biologically active.
- Folic acid and folates are forms of water-soluble vitamins like Vit. B 12.
What are the differentiating features of folic acid and folate?
| Clinical parameters | Folic acid | Folate |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What are the important facts about Folic Acid and Folate facts?
- Humans cannot synthesize p-aminobenzoic acid or attach glutamic acid to pteridine.
- This is the reason that folates occur naturally in food like:
- Yeast.
- Liver.
- Leafy vegetables.
- Folic acid is a synthetic form of the vitamin.
- Folate activity is around 95% in the RBCs.
- The activity in the serum is about 40% and is protein-bound.
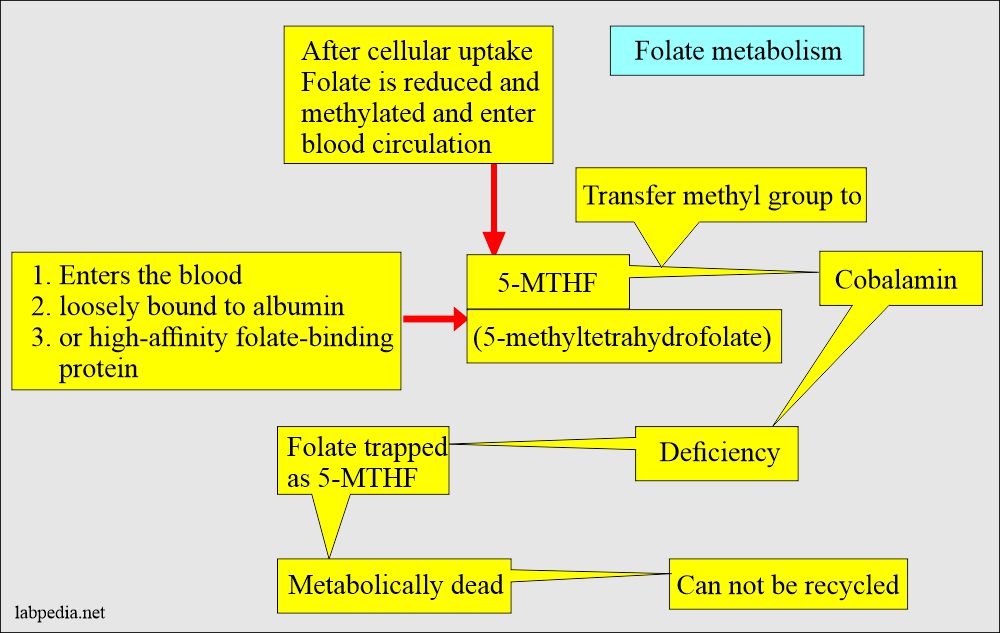
- Vitamin B12 and Folate are linked by the transfer of the methyl group from the 5-methyltetrahydrofolate (5-MTHF).
-
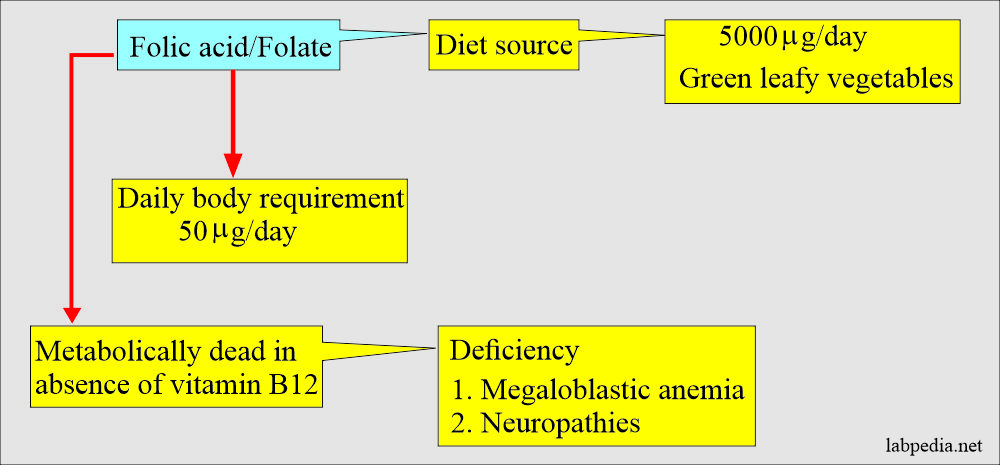
- In the case of cobalamin deficiency, 5-MTHF is metabolically inactive.
-
What are the requirements of Folic Acid and Folate?
- A normal diet consists of 500 to 700 µg of Folate, and 50 µg is absorbed daily.
- Another source says that the normal dietary intake of Folate is 200 to 250 µg.
- The minimum daily adult requirement is 100 to 150 µg.
- Another source says daily requirements are 60 to 280 µg to replace the losses.
- The body storage is 10 to 12 mg and is sufficient for 4 months (another source storage for one month).
- Another source says total body stores are 12 to 28 mg.
What is the synthesis and site of absorption of Folic Acid and Folate?
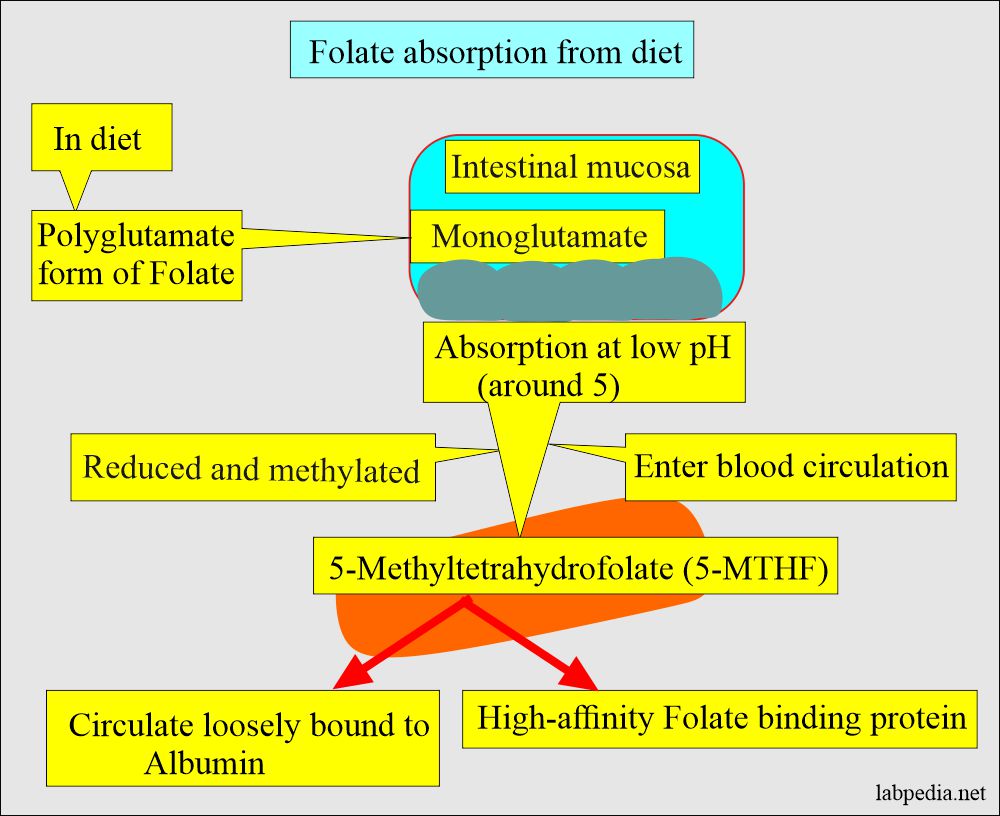
- Its absorption site is the duodenum and jejunum.
- The bacteria form folic acid in the intestine.
- Folic acid is stored in the liver.
- A liver biopsy shows half of the body’s stores of folates.
- 0.5 to 1% of the body’s stores are catabolized or excreted daily.
- The intestinal enzyme cleaved folate derivatives in the diet to monoglutamyl Folate for absorption.
- Enzyme folate reductase reduces it into tetrahydrofolate by using NADPH as a donor.
What are the sources of Folic Acid and Folate?
- It is present in:
- Eggs and milk.
- Leafy vegetables (spinach, broccoli, and lettuce).
- Okara, and asparagus.
- Fruits (bananas, melons, lemons).
- Orange juices and tomato juices.
- Beans, yeast, mushrooms, and meat (beef liver and kidney).
- Liver.
- Yeast.
- Orange juice.
- Folic acid is added into:
- Cereals.
- Bread.
- Flour.
- Pasta.
- Bakery items.
- Cookies.
- This is stable in an acid solution and rapidly absorbs in an empty stomach.
- This is unstable in light.
- Supplemental folate absorption is 100% in comparison to dietary folates.
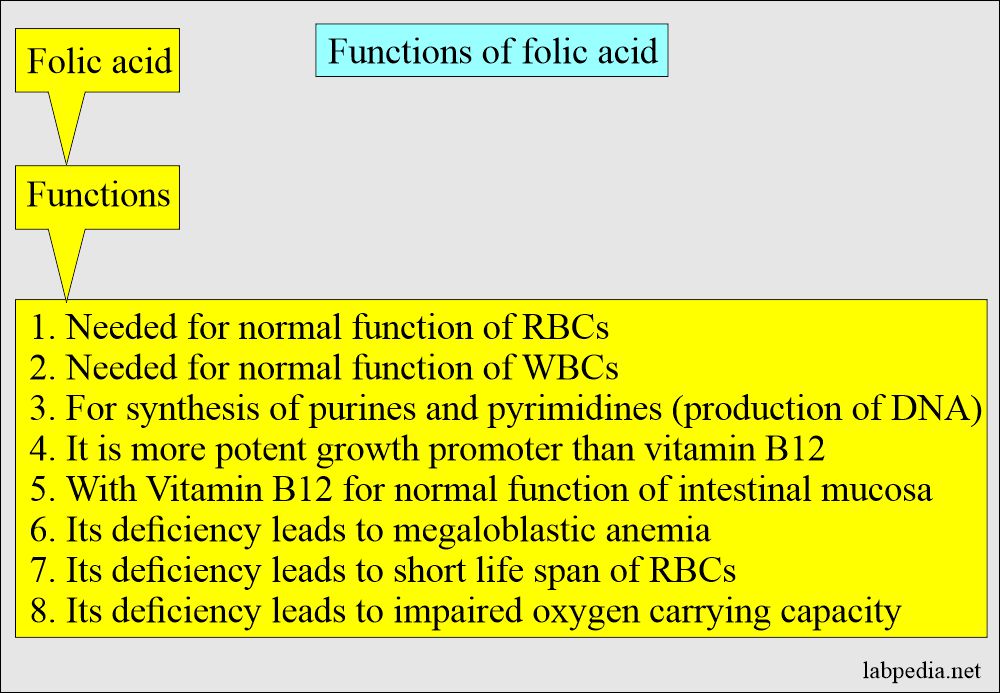
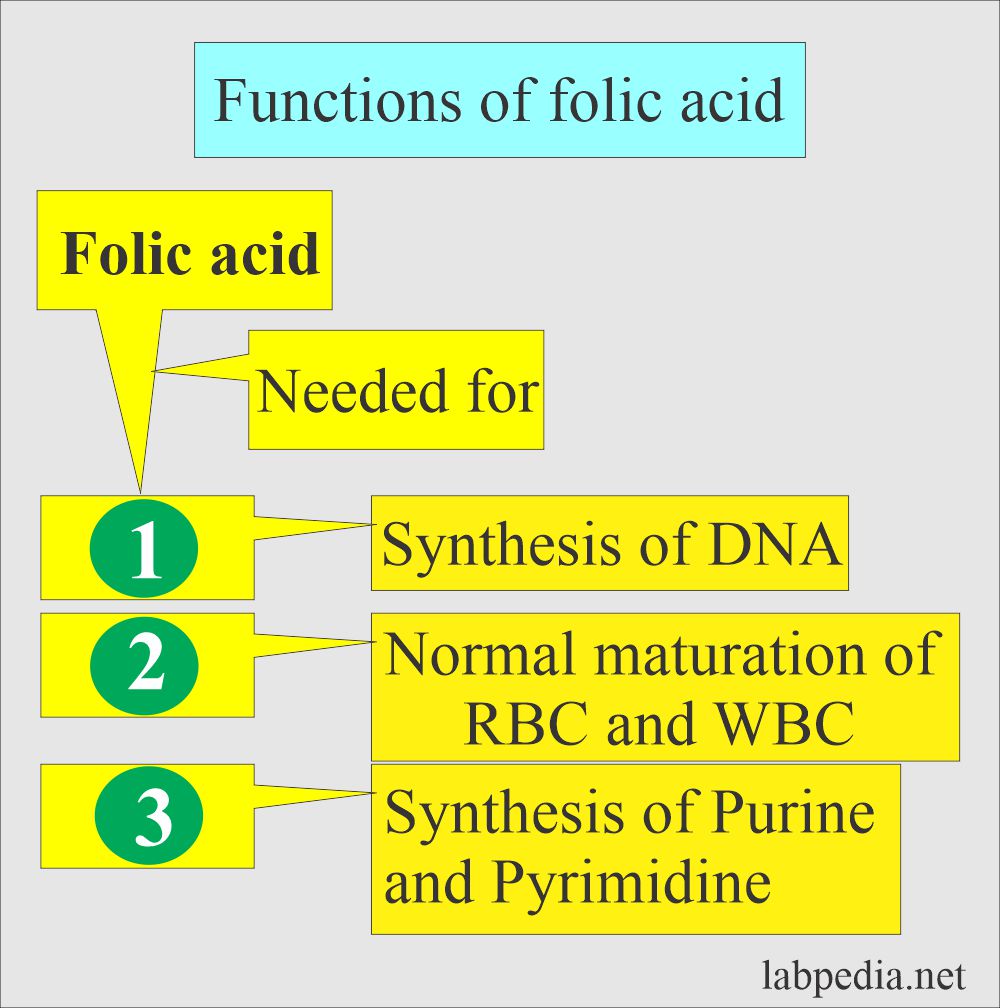
What are the functions of the Folic Acid and Folate?
- Folic acid produces and maintains new cells.
- It prevents changes in the DNA, which may lead to cancer.
- Folic acid is needed for the normal function and maturation of RBCs and WBCs.
- Folic acid is a potent growth promotor, and it depends upon the normal functioning of the intestinal mucosa for absorption.
- Folic acid is also needed to synthesize purine and pyrimidines, which, in turn, are precursors of cell DNA.
- Folic acid is needed to synthesize purines and pyrimidines, a precursor of cell DNA.
- Folic acid is needed for the DNA.
- Folate is also needed for methionine synthesis, histidine catabolism, and serine and glycine metabolism.
- It is a hypothesis that folic acid is involved in congenital abnormalities.
- Methylation of homocysteine to methionine.
- Methionine is converted to S-adenosylmethionine, a universal donor of a methyl group to:
- DNA.
- RNA.
- Hormones.
- Neurotransmitter.
- Membrane lipids.
- Proteins.
- The elevation of homocysteine concentration has shown an increased risk for coronary artery disease and cerebrovascular disease.
- Methionine is converted to S-adenosylmethionine, a universal donor of a methyl group to:
What are the sources of Folic Acid and Folate?
- Folates occur naturally in foods, and folic acid is the synthetic form.
- Folic acid has been added to cold cereals, flour, bread, pasta, bakery items, cookies, and crackers, as required by federal law from 1998.
- Foods rich in folates are spinach, lettuce, broccoli, okra, asparagus, and rich fruits, including bananas, watermelon, lemon, orange juice, and tomato juices.
- Folic acid is present in eggs, milk, yeast, liver, fruits, leafy vegetables, and fruits.
- Folate is also present in beef liver and kidneys.
- Folic acid is a more potent growth factor than Vit.B12.
- Determination of serum folic acid and RBC folic acid is the best measure to rule out folic acid deficiency.
- Vit B12 is needed to incorporate folic acid into tissue cells.
What are the causes of Folic Acid and folate deficiency?
- Megaloblastic anemia is the major manifestation of folate deficiency.
- Folic acid deficiency causes megaloblastic anemia and can not be differentiated from pernicious anemia in laboratory tests except the Schilling test without intrinsic factor (IF).
- Neurological symptoms are absent in folic acid deficiency.
- Pernicious anemia is due to a deficiency of vitamin B12 and not a folic acid deficiency.
- It is important to differentiate B12 from folic acid.
- The absence of intestinal bacteria (sterilized gut).
- Poor intestinal absorption may be seen after surgery or sprue.
- Insufficient dietary intake.
- Excessive demands, as in pregnancy, liver diseases, or malignancies.
- Treatment with antifolate drugs like methotrexate anticonvulsant therapy.
- In alcoholics.
What are the toxic effects of an overdose of Folic Acid and Folate?
- Can Precipitate neuropathy in patients having a deficiency of Vitamin B12.
- It masks vitamin B12 deficiency.
- This may delay the treatment of deficiency and allow progress to the neuropathy.
What are normal folic acid and folates?
Source 4
- Adult (fasting) = 3 to 20 ng/mL, (11 to 57 nmol/L)
- Adult (serum) = 2 to 20 ng/mL, (4.5 to 45.3 nmol/L)
- Children (serum) = 5 to 21 ng/mL (11.3 to 47.6 nmol/L)
- Infants = 14 to 51 ng/mL (31.7 to 115.5 nmol/L)
- RBCs folate:
- Adults = 140 to 628 ng/mL (317 to 1422 nmol/L)
- Children = >160 ng/mL (>362 nmol/L)
Another source
- <60 years adults = 1.8 to 9.0 ng/mL (4.1 to 20.4 nmol/L)
- >60 years adults = 1.2 to 12 ng/mL (1.2 to 12 nmol/L)
What is the equivalent of dietary folate (DEF)?
- It is dietary daily requirements of the body:
- 0 to 6 months DEF = 65 µg/day.
- 1 to 3 years DEF = 150 µg/day.
- 4 to 8 years DEF = 200 µg/day.
- 9 to 13 years DEF = 200 µg/day.
- 19 years to older DEF = 300 µg/day.
- 14 to 18 years DEF = 300 µg/day.
- Pregnant women DEF = 600 µg/day.
Source 1
Normal Folate
- 2 to 16 years = 5 to 21 ng/mL.
- >16 years = 3 to 20 ng/mL.
- To convert into SI unit x 2.265 = nmol/L
Source 2
Normal folic acid (Folate)
- 5 to 25 ng/mL (11 to 57 nmol/L)
Another source
- Adult fasting serum folate = 3 to 20 ng/mL (7 to 45 nmol/L).
Source From Medscape
- Adult = 2 to 20 ng/mL
- Children = 5 to 21 ng/mL
- Infants = 14 to 51 ng/mL
RBC folate
- Normal range = 5 to 15 ng/mL
- Borderline range = 3 to 5 ng/mL (variable hematologic findings)
- <3 ng/mL range = Positive hematologic findings
What is the purpose of folic acid treatment?
- Memory loss.
- Age-related hearing loss.
- Alzheimer disease.
- It reduces the aging effect.
- Sleep problems, nerve pain, depression, and muscle pain.
- In a patient with methotrexate treatment.
- Some people recommend preventing colon cancer and cervical cancer.
How will you do a Lab diagnosis of folic acid/folate deficiency?
- Serum measurement of the folic acid diagnoses folic acid deficiency.
- RIA assay is simpler than the bacterial method.
- RBC folate level may be advised.
- Draw-backs of serum folate assay:
- The small laboratory can not perform this test.
- Serum folate levels fall below normal limits 3 to 4 weeks after the dietary or absorption-induced deficiency begins.
- RBC folate levels become abnormal about 3 months later than serum folate.
- Anemia develops 5 months after the onset of folate deficiency.
- A diet full of folate may increase the serum folate level. While RBC folate will be low.
- Serum folate levels may be low in severe liver and kidney diseases.
- A therapeutic trial of the folate may be advised.
When will you see an increased level of folic acid?
- Pernicious anemia.
- Massive blood transfusion in recent times.
- Vegetarian food contains more folic acid.
When will you see a decreased level of folic acid/Folate?
- Malnutrition. Dietary deficiency is the most common cause.
- Dietary deficiency is most common in alcoholics.
- It is postulated that alcohol inhibits folate absorption and interferes with folate metabolism.
- Malabsorption syndrome, e.g., Sprue, Celiac disease.
- This is the second most common cause and is due to primary small bowel disease.
- Pregnancy.
- This may be seen in 10% to 25% of pregnant ladies with some degree of folic acid deficiency.
- In pregnancy, folic acid deficiency is due to diet and increased fetal demands.
- More severe deficiency (<5%) may be seen in the third trimester.
- Hemolytic anemia.
- Megaloblastic anemia.
- Liver diseases.
- Malignancies.
- Chronic renal disease.
- Vit.B12 deficiency.
- Malignant tumor-like metastatic carcinoma, acute leukemias.
- Myelofibrosis.
- Crohn’s disease.
- Ulcerative colitis.
- Intestinal resection and jejunal bypass procedure.
- In chronic alcoholics.
- In the case of anorexia nervosa.
- Drugs like:
- Anticonvulsant drugs like phenytoin show in roughly 30% of the cases. It is also seen in primidone.
- Cytotoxic drugs like methotrexate exert an antitumor effect by interfering with folate metabolism.
- Colchicine, para-aminosalicylic acid (PAS), and neomycin interfere with folic acid absorption in some of the patients.
- Diet, pregnancy, and anticonvulsant drugs show normal Schilling test.
What are the drugs that act as an antagonist to folic acid?
-
- Anticonvulsant.
- Methotrexate and aminopterin.
- Antimalarial.
- Heavy use of antacids.
- Oral contraceptives.
Questions and answers:
Question 1: What is the main function of the folic acid?
Question 2: What is the antagonist to the absorption of folic acid?