Semen:- Part 4 – Workup of Infertile Couple
Workup of Infertile Couple
How will you define infertility?
- Infertility is the inability to conceive after one year of intercourse without contraceptive devices or medications.
- Infertility is divided into:
- Primary infertility is the infertile couple who had no previous successful pregnancy.
- Secondary infertility affects individuals who had a previous successful pregnancy but are now unable to conceive.
- To evaluate infertility and fertile couples, hormones and semen workups are needed.
How will you do Male Workup for Fertility?
Semen analysis:
- It includes count, ejaculate volume, pH, and motility, as discussed in Part 1.
How will you check Sperm functions?
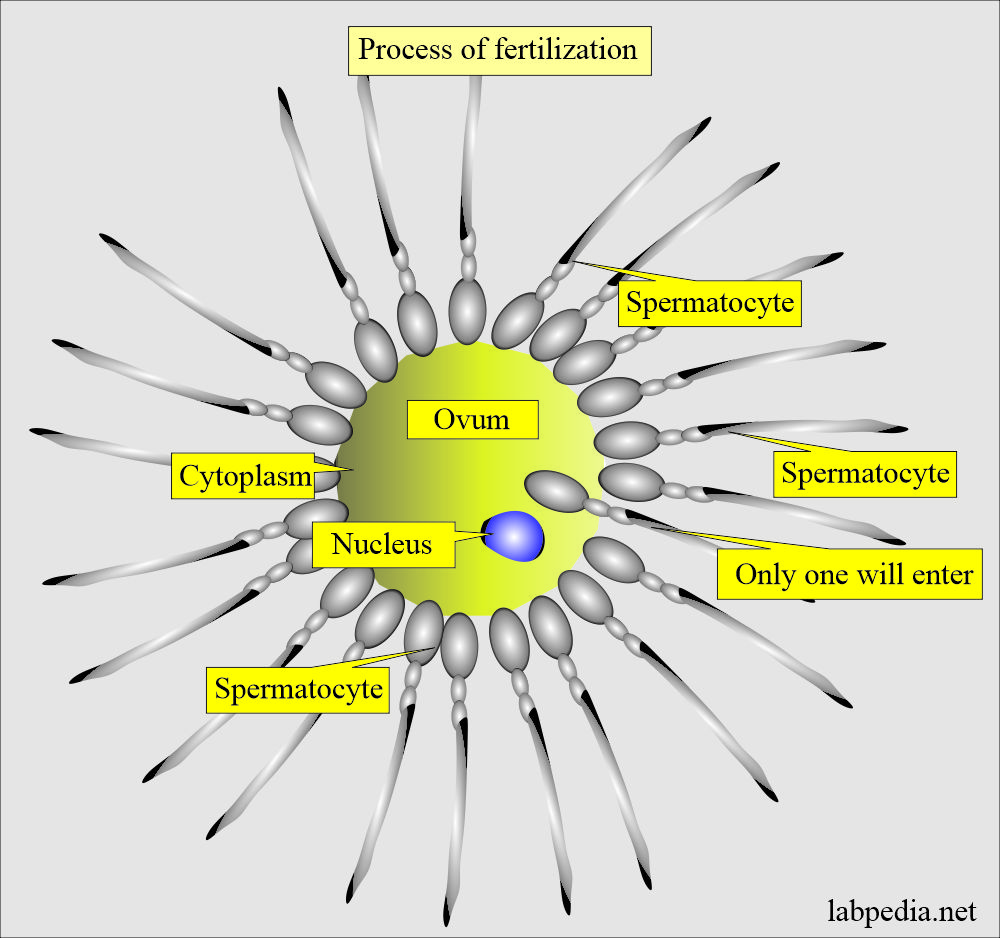
- The sperm should reach the ovum through directed motion, undergo capacitation, and fuse with the oocyte membrane.
- Only one sperm will enter the ovum.
- Then, it will be incorporated into the oocyte cytoplasm.
How will you summarize the sperm function tests?
| Sperm function tests | Details of the test and interpretations |
|
|
|
|
|
|
|
|
How will you demonstrate Sperm-mucous penetration?
- This will tell us the ability of the sperm to travel through the vaginal mucous to reach the uterus.
- In vitro test to check the penetration ability:
- Bovine cervical mucus is taken in the capillary tube.
- The migration of the sperm in the tube is measured.
- The following factors are noticed:
- Migration distance.
- Penetration density.
- Duration of the progressive movement.
- Migration reduction.
How will you assess the sperm motility?
- The presence of sperm capable of forwarding the progressive movement is critical for fertility.
- This progressive movement propels the sperm through the cervical mucus to the uterus and fallopian tubes and to the ovum.
- This should be done on well-mixed, liquefied semen within one hour of the collection.
How will you grade Sperm motility?
| Grade of the motility | Criteria for the motility |
|
|
|
|
|
|
|
|
|
|
How will you assess sperm viability testing?
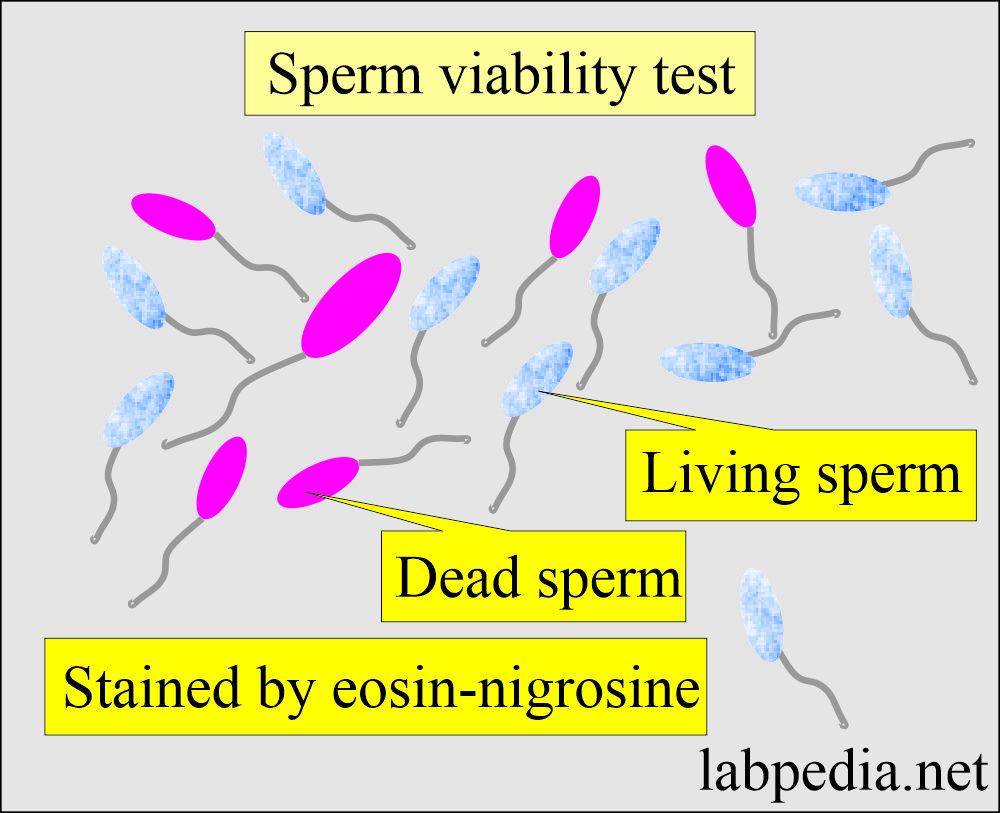
- Decreased sperm viability will lead to infertility.
- Procedure to check sperm viability:
- Mix semen with eosin-nigrosine stain.
- After a few minutes, make the smear.
- Now count the number of dead sperms per 100 sperms.
- Living sperms will not take the dye and will have a bluish-white color.
- The dead sperm will stain red against the purple background.
- Normal viability requires 75% of the living sperm.
How will you assess the Seminal fructose?
- Low sperm concentration is caused by the lack of a support medium in the seminal fluid, such as fructose.
- If fructose is low or absent in the seminal fluid, this will lead to low sperm concentration in the semen.
- The normal fructose level is 13 µmol per ejaculate.
- The resorcinol test judges the fructose concentration:
- Resorcinol reagent consists of:
- 50 mg resorcinol in 33 mL of concentrated HCL.
- Make the volume 100 mL by adding the distle water.
- Procedure:
- Mix 1 mL of semen with 9 mL of resorcinol reagent.
- Boil the test tube.
- Result: Observe the orange-red color.
- The specimen should be tested within 2 hours of the semen collection or frozen to prevent fructolysis.
How will you check the Antisperm antibodies?
- Antisperm antibodies may be present in both males and females.
- These antibodies may be detected in the following samples:
- Semen.
- Cervical mucosa.
- Serum.
- Antisperm antibodies are identical in the male and female infertility evaluation; these can be detected by:
- Agglutination.
- Immobilization.
- Radioimmunoassay (RIA).
- Immunofluorescent assay.
- Enzyme-linked immunoabsorbent assay (ELIZA).
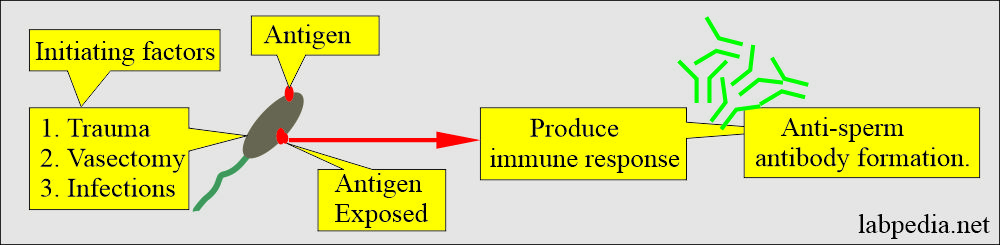
- Both partners may show antisperm antibodies, which are more common in males.
- Under normal conditions, the blood test barrier will prevent sperm exposure to the immune system.
- There is the exposure of the sperm to the immune system in the case of vasectomy, trauma, and infections.
- An antigen on the sperm will produce the antibody, damaging the sperm.
- The damaged sperm produces antibodies in the female.
- Antibodies are suspected in males when sperm clumping is seen in routine semen analysis.
- The presence of antisperm antibodies in the female can be seen:
- Mix the sperm with the cervical mucosa or the serum.
- Observe the agglutination.
- Other tests for the antisperm antibodies are:
- Mixed agglutination reaction:
- This is a screening procedure to detect IgG antibodies.
- Semen containing motile sperm is incubated with IgG antihuman globulin (AHG).
- Latex suspension or treated RBCs coated with IgG.
- The bivalent AHG will bind the sperm and the other side to latex-coated particles (or IgG-coated RBCs).
- This reaction will give rise to microscopically agglutination or clumping of the sperms.
- Result: <10% of the motile sperms attached to the latex particles are considered normal.
- Immunobed test:
- This is a more specific test, and it can detect IgG, IgM, and IgA antibodies.
- This will also show which area of the sperm, head, neck, or tail is affected.
- Antibodies against the head will interfere with the penetration of the sperms to the ovum or cervical mucosa.
- Procedure: Sperms are mixed with polyacrylamide beads coated with either anti-IgG, anti-IgM, or anti-IgA.
-
- Examine under the microscope, showing the beads attached to the sperm at a particular area.
- Result: The presence of beads <20% of the sperms is normal.
-
- Simes-Hunter test:
- This post-coital test rules out any factors present in the cervical mucosa.
- Procedure: This is usually done in the mid-cycle ovulatory phase with maximum cervical mucus.
- After 2 to 3 hours of the post-coital period (after the intercourse).
- Expose the cervix and take mucus from the endocervix.
- Examined the aspirated material under the microscope.
- Result: Report the total number of sperms/HPF and the percentage of motile sperms.
How will you Evaluate the level of hormones in Males?
How will you estimate Serum testosterone levels in males?
- This is important when the secondary sex characters’ development is deficient.
- I/M 5000 IU of CG (Chorionic gonadotropins) was injected to evaluate the Leydig cell function.
- Measure the serum testosterone level between 48 and 96 hours after the injection.
- Males with hypogonadism will have a decreased testosterone response to the injection.
How will you evaluate FSH levels in males?
- It will be measured in patients with a count of 5 to 10 million/mL semen.
- Elevated FSH level = Sertoli cell dysfunction.
- Males may show azoospermia.
- Primary germinal cell failure.
- Klinefelter syndrome.
- Elevated FSH + LH + low testosterone + oligospermia in males = Primary testicular failure or andropause (decreased sexual satisfaction, reduced body hairs).
How will you assess abnormal semen?
- Decreased count of sperm:
- There may be a lack of seminal fluid nutrients for the sperm-like fructose.
- Advise fructose level and test.
- Decreased motility with normal count:
- There is a viability issue.
- Advise Eosin-nigrosin test.
- Normal count with continued infertility:
- Check for the female antisperm antibodies.
- Advise immunobead test.
- Check for sperm agglutination with female serum.
- Decreased motility with clumping:
- There may be male antisperm antibodies.
- Mix sperm with male serum for agglutination.
- Advise Immunobead test.
- Advise mixed agglutination reaction.
How will you summarise male infertility factors?
| Abnormality in the fertilizing organs | Causes or etiology of infertility |
|
|
|
|
|
|
|
|
|
|
How will you do Female Workup for Fertility?
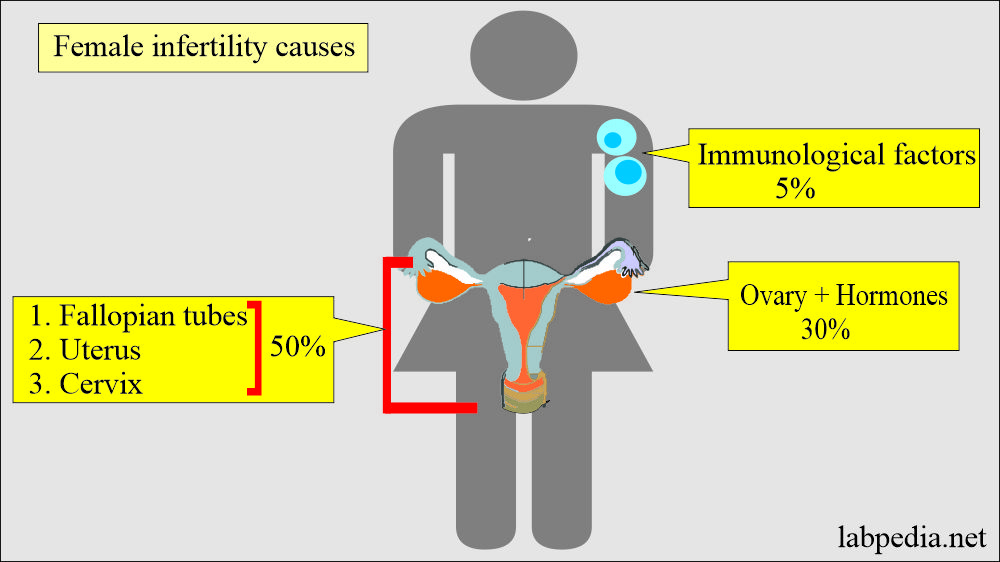
- In females, mostly infertility factors are attributed to ovaries and hormones in almost 30% of the cases.
- While the pelvic factors include fallopian tubes and cervix.
- Uterine diseases account for almost 50% of the cases.
- Immunological factors are involved in roughly 5% of infertile ladies.
- Ovarian dysfunction can develop regardless of whether the female has regular menses, making it difficult to diagnose ovarian dysfunction.
- Product of conception (PCO) results in androgen excess is the most common cause of anovulation.
- Ovulatory dysfunction is caused by liver and thyroid diseases.
How will you Evaluate female infertility?
- It includes the detailed history of the patient and physical examination.
- If you find the obvious cause, then treat that.
- In the case of abnormal menstrual history, further evaluation of the hormones is done.
How will you perform the Post-coital test?
- The post-coital test is the quick assessment of multiple factors affecting fertility.
- Procedure: Collect the post-coital cervical mucus in the middle of the cycle.
- Place it on the glass slide with two coverslips.
- The mucus with adequate estrogen stimulation is clear and thin.
- This mucus forms a 6 cm or greater thread in length when the coverslips are separated from the slide.
- When examined under the microscope, air-dried mucus, which has an adequate estrogen effect, forms a fern-like pattern.
- Before mucus gets dried, >20 motile sperms are seen under a microscope/HPF.
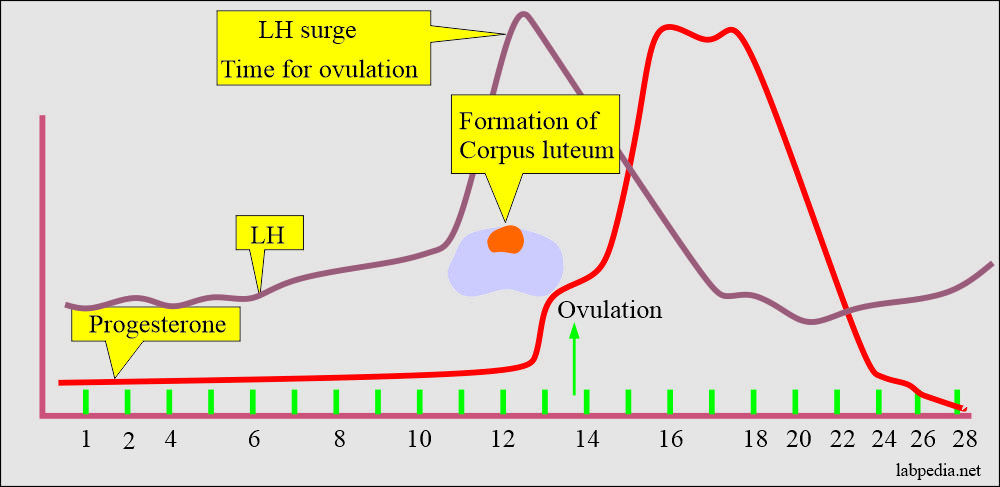
How will you assess Progesterone levels in females?
- Measurement of the progesterone level is the primary assay used to evaluate ovulation.
- After ovulation, the blood progesterone level rises, and the peak is within 5 to 9 days ( day 21 to day 23).
- If there is no ovulation, then there is no formation of the corpus luteum and no rise in the progesterone hormone.
- A progesterone level of >10 ng/ml suggests normal ovulation.
- While a progesterone level of <10 ng/mL indicates an anovulatory cycle.
How will you assess luteinizing hormone (LH) surge?
- LH appears in the urine just after the physiologic LH surge, which occurs 24 to 36 hours before ovulation.
- LH surge confirms the ovulation and guides the time for intercourse.
- There are kits available to check the LH surge and find the time of ovulation.
What are the Hormonal changes in females?
FSH (Follicular stimulating hormone):
- In the case of primary ovarian failure (Hypergonadotropic hypogonadism), there is repeatedly elevated basal FSH level (>30 IU/L).
- Or a single elevated level of >40 IU/L.
- Patients with hypergonadotropic hypogonadism also have low estrogen levels (Hypoestrogenic). These patients have estradiol <20 IU/L.
Hypogonadotropic (hypogonadism) case shows:
- Estradiol = <40 pg/mL (110 pmol/L).
- LH = <10 IU/L (LH level is decreased).
- FSH = <10 IU/L (FSH level is decreased).
Prolactine level:
- Hyperprolactinemia causes hypergonadotropic hypogonadal infertility in these patients.
- Prolactin levels may be high in patients taking drugs like antidepressants, cimetidine, and methyldopa.
- Prolactin level will be raised in products of conception (PCOS).
TSH (Thyroid-stimulating hormone):
- TSH level should be measured to rule out hypothyroidism.
Pituitary gland:
- Radiographic imaging is needed to rule out pituitary adenoma or empty sella syndrome.
How will you summarize female infertility factors?
| Etiological factors | Causes (Etiology) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Questions and answers:
Question 1: What is the value of fructose in the semen?
Question 2: What is the value of raised FSH in males?